Protocol for the Addition of Contrast to Echocardiography Studies
advertisement
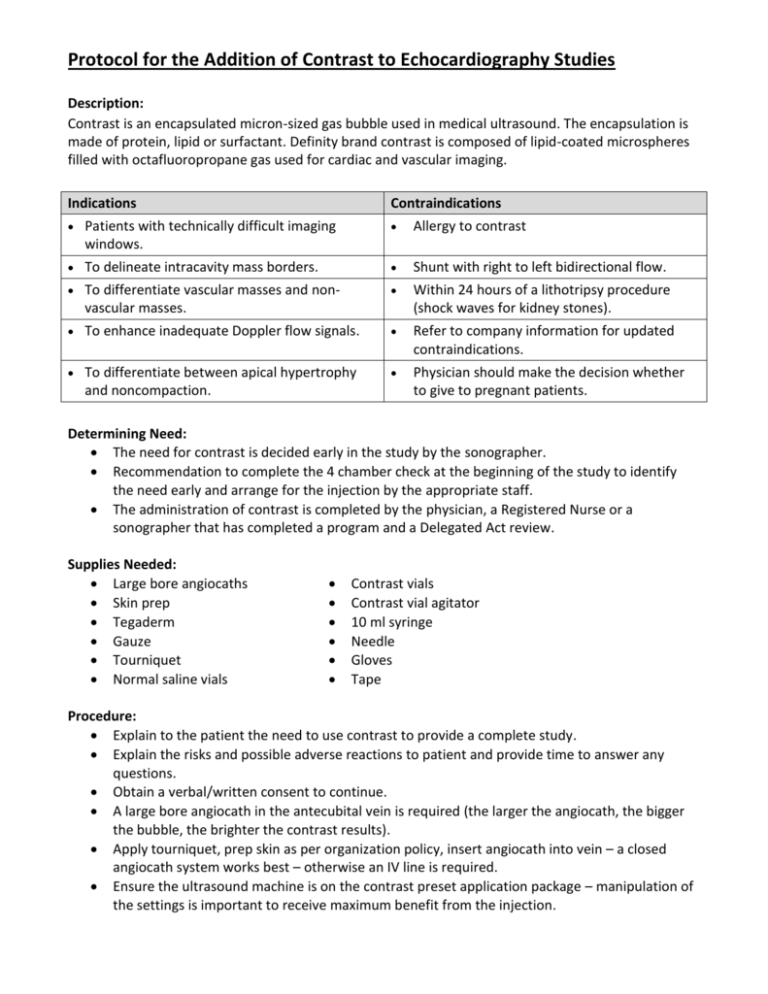
Protocol for the Addition of Contrast to Echocardiography Studies Description: Contrast is an encapsulated micron-sized gas bubble used in medical ultrasound. The encapsulation is made of protein, lipid or surfactant. Definity brand contrast is composed of lipid-coated microspheres filled with octafluoropropane gas used for cardiac and vascular imaging. Indications Contraindications Patients with technically difficult imaging windows. Allergy to contrast To delineate intracavity mass borders. Shunt with right to left bidirectional flow. To differentiate vascular masses and nonvascular masses. Within 24 hours of a lithotripsy procedure (shock waves for kidney stones). To enhance inadequate Doppler flow signals. Refer to company information for updated contraindications. To differentiate between apical hypertrophy and noncompaction. Physician should make the decision whether to give to pregnant patients. Determining Need: The need for contrast is decided early in the study by the sonographer. Recommendation to complete the 4 chamber check at the beginning of the study to identify the need early and arrange for the injection by the appropriate staff. The administration of contrast is completed by the physician, a Registered Nurse or a sonographer that has completed a program and a Delegated Act review. Supplies Needed: Large bore angiocaths Skin prep Tegaderm Gauze Tourniquet Normal saline vials Contrast vials Contrast vial agitator 10 ml syringe Needle Gloves Tape Procedure: Explain to the patient the need to use contrast to provide a complete study. Explain the risks and possible adverse reactions to patient and provide time to answer any questions. Obtain a verbal/written consent to continue. A large bore angiocath in the antecubital vein is required (the larger the angiocath, the bigger the bubble, the brighter the contrast results). Apply tourniquet, prep skin as per organization policy, insert angiocath into vein – a closed angiocath system works best – otherwise an IV line is required. Ensure the ultrasound machine is on the contrast preset application package – manipulation of the settings is important to receive maximum benefit from the injection. Agitate contrast vial as directed to go from a clear solution to a milky colour. Vent vial to release air; do not inject air into the vial. In a 10 ml syringe, draw up 1 ml of contrast and 9 ml of saline. Roll in palms of hands to mix. Draw up a saline flush syringe. There are several ways to administer contrast: directly, or mixed in a mini bag and infused by pump. Occasionally there is a blackout in the far field – this will resolve after approximately 10 beats. Swirling in the left ventricle may require lowering of mechanical index. Acquire images and/or Doppler. Zoom into the apex and assess for mural thrombus. A good time to do an RVSP is when the contrast weakens. Contrast bubbles can be broken down by changing the preset back to full strength and imaging. Remove angiocath, apply pressure and apply bandage. Considerations: Echo Lab should have an antihistamine kit in case of an adverse reaction. Crash cart should be close by. Patient should be kept for a minimum of 20 minutes from the time of injection to ensure they have been properly assessed for a reaction. Oxygen saturation monitor available in case of breathing difficulties – COPD or asthmatic patients may require monitoring. If a patient has an RVSP of greater than 70 mmhg: a physician should make the decision whether to give contrast or not. Pre-printed order forms in place for administration. Any adverse reaction (most common are rashes and back pain) should be documented and reported to the supervising Cardiologist so the patient can be assessed. Contrast can be used for TTE, TEEs to help define LAA thrombus, and with stress tests to better define all the LV walls. Reasons to Use Contrast: Patient obesity. Horizontal or vertical cardiac placement. Pneumothorax. Patient immobile and cannot be positioned properly. Pectus excavatum. Narrow rib spaces. Patient uncooperative or agitated.