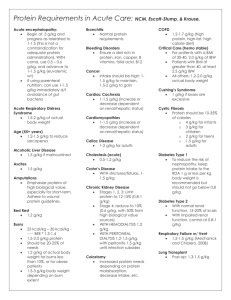
Others
advertisement

Locomotor Disorder– core How common is it Core symptoms Biological causes/risk factors Investigations e.g. to confirm diagnosis, exclude physical causes etc Treatment Biological e.g. specific drugs Gout an inflammatory arthritis Increasing in developed countries; 0.2% in Europe and USA (though hyperuricaemia = ~5% pop); M>F 10:1; rarely before young adulthood or premenopause; increasing in older women due to use of diuretics Hyperuricaemia causes 4 clinical scenarios: acute sodium urate synovitis – gout = typical presentation chronic polyarticular gout = unusual except in elderly on diuretics or in renal failure chronic tophaceous gout urate renal stone formation (p. 610). Typical presentation: Middle-aged man, sudden pain, swelling and redness of first MTPJ; often precipitated by too much food or alcohol, by dehydration of by starting a diuretic. Untreated, resolves within a week with desquamation of the skin. Severe attacks may cause overlying crystal cellulitis and be difficult to distinguish from infective cellulitis – if in doubt = do blood and joint fluid cultures. Due to one of two types of crystal (which account for crystal-induced arthritis) = intra-articular sodium urate, and hyperuricaemia (defined as a serum uric acid > 2 standard deviations from the mean (420 μmol/L in males, 360 μmol/L in females). This is close to the limit of solubility. Most people with hyperuricaemia are asymptomatic despite crystals in their joints. Serum uric acid levels ↑ with age, obesity, a high-protein diet, a high alcohol consumption (particularly beer drinkers), a high fructose intake from sweetened drinks, combined hyperlipidaemia, diabetes mellitus, ischaemic heart disease and hypertension (metabolic syndrome, p. 799). There is often a family history of gout. Note, often no obvious cause is found. Either due to impaired excretion of uric acid relative to ingestion/production (main cause; eliminated by either kidneys 66% or intestine 33%), or due to increased production or uric acid (via ↑ purine acid production) Causes: 1. Impaired excretion of uric acid Chronic renal disease (clinical gout unusual) Drug therapy, e.g. thiazide diuretics, low-dose aspirin Hypertension Lead toxicity Primary hyperparathyroidism Hypothyroidism Increased lactic acid production from alcohol, exercise, starvation Glucose-6-phosphatase deficiency (interferes with renal excretion) 2. Increased production of uric acid Increased purine synthesis de novo due to: Hypoxanthine-guanine-phosphoribosyl transferase (HGPRT) reduction (an X-linked inborn error causing the Lesch–Nyhan syndrome) Phosphoribosyl-pyrophosphate (PRP) synthase overactivity Glucose-6-phosphatase deficiency with glycogen storage disease type 1 (patients who survive develop hyperuricaemia due to increased production as well as decreased excretion) Increased turnover of purines due to: Myeloproliferative disorders, e.g. polycythaemia vera Lymphoproliferative disorders, e.g. leukaemia Others, e.g. carcinoma, severe psoriasis Often diagnoses clinically (and confirmed with rapid response to NSAIDs or colchicines): 1. Joint fluid microscopy: most specific 2. Serum uric acid: usually ↑ >600mol/L (if not, recheck after a few weeks as the levels fall immediately after an attack) 3. Serum urea and creatinine: monitor for signs of renal impairment NSAIDs or coxibs in high doses to reduce pain and swelling naproxen: 750 mg immediately, then 500 mg every 8–12 hours diclofenac: 75–100 mg immediately, then 50 mg every 6–8 hours lumiracoxib: 100 mg once daily indometacin: 75 mg immediately, then 50 mg every 6–8 hours. Although regarded as the ‘gold standard’ treatment by some, the frequency of side-effects is unacceptably high with indometacin. In people with renal impairment (and because NSAIDs can ↑ this) use: colchicine: 1000 μg immediately, then 500 μg every 6–12 hours, but this causes diarrhoea corticosteroids: intramuscular or intra-articular depot methylprednisolone. Treatment – social Allopurinol: only when attacks are severe and frequent despite dietary changes or when NSAIDs and colchicine are difficult to tolerate; never start during an acute attack, and always start once pt has taken NSAIDs/colchicine for 2 weeks (and continue them for 4 weeks afterwards) as allopurinol may precipitate an acute gout. Allopurinol blocks xanthine oxidase, which converts xanthine into uric acid; reducing serum uric acid over time. Febuxostat is a new non-purine analogue inhibitor of xanthine oxidase. Often the first attacks are managed symptomatically, but people should reduce alcohol (beer) which is ↑ in purines, reduce calorie and cholesterol intake, avoids such foods as offal, some fish and shellfish and spinach. Disorder– core How common is it Who does it affect Core symptoms Biological causes/risk factors Osteoporosis: disease characterised by low bone mass and micro-architectural deterioration of bone tissue, leading to ↑ bone fragility and ↑ risk of fracture; WHO = bone density 2.5SD <young healthy adult mean value; values between -1 and -2.5SD = ‘osteopenia’ Many pts have radiological evidence but are asymptomatic. ½ women and 1/5 men aged 50 years will have an osteoporotic fracture during their remaining lifetime. Risk of fracture ↑ exponentially with age and changing population demographics will see an ↑. Fracture is the only cause of symptoms in osteoporosis. Normally proximal femur Sudden onset of severe pain in the spine radiating round to the front = vertebral crush fracture though only 1/3 are symptomatic; also leads to increasing kyphosis, height loss, abdominal protuberance Fall on outstretched arm = Colles’ fracture likely Pathogenesis: ↑ bone breakdown by osteoclasts (by increased MMPs and decreased TIMPs) and ↓ formation by osteoblasts => ↓ bone mass; Bone mass will ↓ with age but depends on the ‘peak’ bone mass attained in adult life and the rate of loss in later life; genetic factors = most significant factor for peak bone mass (genes for collagen type1A1, vit D receptors, oestrogen receptors); Nutritional factors, sex hormones and exercise also affect peak bone mass attained Risk Factors: Oestrogen deficiency is major factor Elderly: vit D deficiency and consequent hyperparathyroidism = bone resorptioin and weak bones Glucocorticoids: induce a high turnover state initially, with increased fracture risk evident within three months of starting therapy. More prolonged use leads to a reduced turnover state but with a net loss due to reduced synthesis Investigations e.g. to confirm diagnosis, exclude physical causes etc Plain X-ray: ?fracture DEXA scan: bone density scanning (actually mineral/surface area rather than density per se) of lumber spine or proximal femur; gold standard in osteoporosis diagnosis as accurate, cheap, low radiation dose Quantitative US of the calcaneum: not diagnostic, v cheap and useful as a screening tool prior to DEXA Quantitative CT scanning: true volumetric scanning, expensive, more radiation dose, no clinical adv Management e.g. overall plans, referrals to other services Treatment Biological e.g. specific drugs Investigations to exclude other disease are also useful, esp in men where secondary causes are more likely Fractures in elderly due to osetoporosis are a major cause of mortality and morbidity. . Purpose of management is to reduce absolute risk of fracture; as bone scans are not very sensitive, use BMD-independent RF +/- bone scan to calculate a 10-year risk. 1. Symptomatic management: vertebral fracture = bed rest for 1-2weeks with strong analgesia; TNS may be helpful as are muscle relaxants; physio; 2. Calcium and vit D: Daily intakes of 700–1000 mg of calcium (ideally 1500 mg postmenopausally) and 400–800 IU of vit D are recommended; supplements if these can’t be maintained 3. Exercise: 30 mins of weight-bearing exercise 3x/week to increase BMD 4. Smoking cessation: smoking = lower BMD and increased fracture risk 5. Reduce falls: physio therapy and home assessment If risk factors are ‘skeletal’/ BMD-dependent: bone directed treatment If risk factors are ‘non-skeletal’/ BMD-independent: intervention eg reduction in falls risk needed 1. 2. 3. 4. 5. 6. 7. 8. Bisphosphonates (alendronate): synthetic analogue of bone pyrophosphate; inhibit osteoclasts; increase BMD; decrease risk of fractures; commonly given once weekly doses (70mg); should be taken while fasting, standing/sitting upright with a large drink of water; avoid food and drink for 30 mins after; upper GI s/e (oesophagitis) common. Caution if pt has CKD. ?effect on suppression of bone turnover longterm. Strontium ranelate: two strontium atoms attached to ranelic acid; mechanism unclear; weak antiresorptive properties; ↓ risk of fractures in postmenopausal women; dose is 2g ON; alternative to bisphosphonates esp for elderly Raloxifene: selective oestrogen-receptor modulator (SERM); activates oestrogen receptors in bone preventing BMD loss though only ↓ fracture rates of spine Recombinant human parathyroid hormone peptide 1–34 (teriparatide) and recombinant human parathyroid hormone 1–84: Calcium given with vit D: ↓ non-vertebral fractures in elderly in residential care HRT: 2nd line option for osteoporosis except in early postmenopausal women at high fracture risk due to adverse effects on breast cancer and CVD risk Calcitriol (1,25-(OH)2D3): may ↓ fractures but not enough evidence and monitoring required Calcitronin: nasal/subcut; not enough evidence For glucocorticoid-induced osteoporosis: before beginning long course (3months) of glucocorticoids, check for other RF (age, previous fracture, hormone status). Use DEXA results as a guide for therapy. Disorder– core Core symptoms Biological causes/risk factors Investigations e.g. to confirm diagnosis, exclude physical causes etc Treatment Biological e.g. specific drugs Prognosis Septic/ infective arthritis = joint infection; inflammatory reaction in the joint space (arthritis) caused by infection = MEDICAL EMERGENCY Often young, previously fit people = agonisingly painful, swelling, redness (inflammation), limitation of movement due to muscle spasm (in elderly presentation may not be so obvious) AND systemic upset (fever, chills, night sweats). Duration of symptoms depends on causative organism. Can result from direct invasion of the joint or due to an immune response. Direction infection subdivided into: 1. native (natural) joint infection: organisms enter via blood (haematogenous) or trauma (surgery or injection); synovial tissue is v vascular and lacks a basement membrane ?facilitating seeding of infection; cartilage erosion causes joint space narrowing = impaired function; RF: RA, trauma, IVDU, immunosuppression 2. prosthetic (artificial) joint infection: organisms enter via blood (haematogenous), during surgery or wound infection; joint prosthesis and cement provide surface for bacterial attachment; RF: prior surgery at the site of the prosthesis, RA, corticosteroid therapy, DM, poor nutrition, obesity, ↑ age Causative organisms: most common is Staph A 1. Viruses: parvovirus B19, Rubella, Mumps 2. Bacteria: Staph A, Streptococci (A, B, C, G), G-ve bacilli, Anaerobes, mycobacteria a. Specific for native joints: H influenza, N gonorrhoea, N meningitidis b. Specific for prosthetic: Coagulase –ve staph, enterococci, corynebacteria, propionibacteria 3. Fungi: Candida Investigations: Aspirate: the joint and send fluid for gram staining; usually purulent; also examine for crystals (gout can mimic infection) Blood cultures: often +ve Leucocytosis: total WCC and differential WCC (>75% polymorphs in infection); ESR and CRP raised X-rays: of no diagnostic value except in acute septic arthritis Skin wound swabs, sputum, throat swab, urine: may be +ve and indicate source of infection Wash joint to remove purulent material Immobilise joint initially then start physio to prevent joint stiffness and muscle wasting Empirical IV Abx for 1-2weeks after blood cultures and joint aspirate taken; 1-2g fluoxacillin every 6hrs then fusidic acid orally every 8hrs Directed IV Abx depending on microbiology results Oral switch for ~6weeks Infected prostheses may require removal, replaced with Abx-impregnated spacer for 3-6weeks before a new prosthesis is inserted ? surgery if osteomyelitis present Weight-bearing as soon as the inflammation subsides Resolution of septic arthritis within days-weeks; may lead to secondary OA Disorder– core Core symptoms Biological causes/risk factors Osteomyeltis = infected bone As for septic arthritis except that systemic upset is uncommon; classic = fever, localised pain and overlying erythema Haematogenous: bacteria in blood eg endocaditis or a boil or TB in lung/GIT (spine is commonly involved = Pott’s disease) Contiguous focus: spread from adjacent area of infection eg diabetic foot ulcer infection Direct inoculation: trauma and surgery Malnutrition, debilitating disease and ↓ immunity play a role too. Classification: Cierny and Mader 1985 Stage I: Medullary necrosis of medullary contents or endosteal surface (haematogenous) Stage II: Superficial necrosis limited to the exposed surface Stage III: Localised full thickness cortical sequestration, stable before and after debridement Stage IV: Diffuse extensive, unstable bone Investigations e.g. to confirm diagnosis, exclude physical causes etc Management e.g. overall plans, referrals to other services Staphylococcus causes of 90% acute cases (normal skin flora!) H influenza, Streptococci (A, B), enterococci, Salmonella, Klebsiella, mycobacteria, Brucella also involved sometimes Investigations: Cultures and histology of bone/needle aspirate: gold standard Blood cultures = 50% +ve Superficial swabs are of limited value Leucocytosis is not diagnostic CRP raised and used to monitor response to therapy Immobilisaition Abx – as for septic arthritis; IV – penetration into bone is low Removal of bone (sequestrum) may be indicated but recurrence is common Disorder– core How common is it Who does it affect Core symptoms Osteoarthritis (OA) Commonest joint condition; ↑ with age; most people >60yo will have some radiological evidence of it but only 25% will be symptomatic; occurs world-wide; F 3x> M, usually >50yo; usually primary but nay be secondary to joint disease or other conditions (haemochromotosis); there is a familial pattern of inheritance with DIPJ involvement in nodal OA and also in primary generalised OA Many diverse clinical patterns; hip and knee => major cause of disability; there may be some flare-ups due to inflammation (↑ ESR and CRP) Joint pain, gelling (stiffness and pain after immobility), instability, loss of function Localized OA Nodal OA Joints of hand affected one by one – DIPS commonly Onset painful with associated with tenderness, swelling and inflammation and impairment of hand function. Enthesitis can bee seen on MRI at this stage. Inflammatory phase settles after some months/ years, leaving painless bony swellings: Heberden’s nodes (DIPs) and Bouchard’s nodes (PIPs) – along with stiffness and deformity. PIP deformity may prevent gripping. XR shows the nodes are marginal osteophytes and a loss of joint space. Squaring of hand causes by CMC swelling and fixed thumb adduction => severe compromise in function. Hip OA Affects 7–25% of white adult Caucasians, less so in black Africans and Asians. Two major subgroups defined by XR: a. superior-pole hip OA: joint space narrowing and sclerosis predominantly affect the weight-bearing upper surface of the femoral head and adjacent acetabulum. Commonest in men and unilateral presentation at first b. medial cartilage loss: common in women and associated with hand involvement (nodal generalized OA – NGOA), and is usually bilateral. It is more rapidly disabling. Knee OA Prevalence of symptomatic knee OA is 40% in individuals >75yo. F>M; linked to obesity; bilateral disease with polyarticular OA of the hand (as part of generalised OA) Medial compartment is most commonly affected and leads to a varus (bow-legged) deformity. Previous trauma, meniscal and cruciate ligament tears are RF. Primary generalized OA/ nodal general OA (NGOA) Hands, knees, 1st MTP, hip and IV discs affected; onset is sudden and severe Erosive OA Rare; DIPs and PIPs are inflamed and equally affected but poor functional outcome. Large subchondral cysts; may develop into RA Signs Biological causes/risk factors Crystal-associated OA Commonly seen with calcium pyrophosphate deposition in cartilage (chondrocalcinosis); ↑ with age but is usually asymptomatic; affects wrists, ankle, shoulders; if severe => chronic arthropathy (pseudo-OA); ass with gout; rapidly destructive arthritis in old women Joint tenderness, crepitus, limitation of movement, instability, joint effusion/ inflammation, bony swellings, wasting of muscles Aetiology and Risk Factors: 1. Genetics/ unchangeable factors: a. Genes: familial tendency to develop nodal and generalised OA; collagen type 2? i. Twin studies strongly suggest a hereditary component ii. In Caucasians, there is an inverse relationship between developing osteoporosis and OA b. Gender: higher prevalence after the menopause; F > M => female sex hormone role? i. Women: weight-bearing sports produces 3x ↑ risk of developing OA ii. Men: association between OA and certain occupation eg farming and labouring c. Age! 2. Lifestyle: a. OA is the result of active, sometimes inflammatory but potentially reparative processes rather than end-point of ageing and trauma. b. Diet: lack of antioxidants and vit C may ?predispose OA c. Obesity: increased weight on joints d. Osteoporosis: reduced risk of OA; inverse relationship with OA and osteoporosis e. Trauma: joint fractures, meniscal and cruciate ligament tears also lead to OA f. Occupation: increased use of joints = OA in those joints (miners = OA of hip, knee and shoulders; cotton workers = OA of hands) g. Sport: repetitive use and injury h. Hypermobility: reduced joint stability i. Congenital joint dysplasia: alter joint biomechanics Investigations e.g. to confirm diagnosis, exclude physical causes etc Management e.g. overall plans, referrals to other services 1. Primary OA No known cause 2. Secondary OA Pre-existing joint damage: Rheumatoid arthritis Gout Seronegative spondyloarthropathy Septic arthritis Paget’s disease Avascular necrosis, e.g. corticosteroid therapy Metabolic disease: Chondrocalcinosis Hereditary haemochromatosis Acromegaly Systemic diseases: Haemophilia – recurrent haemarthrosis Haemoglobinopathies, e.g. sickle cell disease Neuropathies Process: Focal destruction of the articular cartilage Spectrum: ranges from atrophic disease with cartilage destruction occurs without any subchondral bone response, to hypertrophic disease in which there is massive new bone formation at the joint margins. Cartilage = matrix of collagen fibres, proteoglycans and water; smooth-surfaced and shock-absorbing; normal balance between degredation and regeneration by chondrocytes o Balance is disrupted therefore cartilage becomes oedematous; focal erosion develops; o Repair is attempted but this is disordered => surface becomes fibrillated and fissured; o Cartilage ulceration exposes underlying bone to ↑ stress, producingmicrofractures and cysts; bone attempts repair but produces abnormal sclerotic subchondral bone and overgrowths at the joint margins called osteophytes. There is also some secondary inflammation. o Macrophages release VEGF; can lead to neovascularisation of the joint and this may bring new innervation of the articular cartilage so there is pain even after the inflammation has subsided Enthesophytes and chrondrophytes seen on MRI precede radiologically apparent osteophytes and joint space narrowing. XR: loss of joint space, subchondral sclerosis and cysts, marginal osteophytes Bloods: ↑ CRP?; Rh factor and anti-nuclear AB are -ve MRI: shows meniscal tears, early cartilage injury and subchondral bone changes Arthroscopy: reveals early fissuring and surface erosion of the cartilage. Aspiration of synovial fluid: (if there is a painful effusion) shows a viscous fluid with few leucocytes and occasionally calcium pyrophosphate crystals. Treat symptoms and disability not the XR appearance Education about condition: ↓ pain and ↑ compliance Exercises: quadriceps exercise to ↑ muscle strength and stability of knee; hydrotherapy helps; local heat, ice packs, NSAID gels work Analgesia: paracetamol and codeine, then NSAIDs, ↓ weight if ↑ BMI, walking aids (a stick on the contralateral side), supportive footwear, physio Intra-articular steroid injections help with symptom relief only if severe, producing only short-term improvement Arthroscopic surgery is not beneficial; Joint replacement is ultimately best way => surgery (replacement arthoplasty); complications (1%) = loosening, late blood-borne infection Disorder– core How common is it Who does it affect Core symptoms Rheumatoid arthritis (RA): autoiummune disease causing chronic symmetrical polyarthritis with systemic involvement due to synovial inflammation World-wide distribution affecting 0.5-1% of population; ↑ prevalence in Pima Indian population and ↓ in Chinese and black Africans; incidence ↓; F 2x> M; Prevalence 1% (↑ in smokers) Present at childhood (rare) to late old age. Commonest onset = 30-50yo Typically (70% cases): slowly Presentations: progressive, symmetrical, ■ Palindromic – 5% cases; Monoarticular attacks lasting 24– peripheral polyarthritis, evolving 48 hours; 50% progress to other types of RA. over weeks/months; pt usually ■ Transient – A self-limiting disease, lasting less than 12 female, 30s (nb rapid onset over months and leaving no permanent joint damage. Usually days/overnight can occur in 15% seronegative for IgM rheumatoid factor and CCP. Some of cases) these may be undetected postviral arthritis. Pain and stiffness in small joints of ■ Remitting – There is a period of several years during which hands, which are swollen: MCPJs, the arthritis is active but then remits, leaving minimal PIPs, DIPs and DTPJ of feet; wrists, damage. elbows shoulders, knees also can be ■ Chronic, persistent – The most typical form, it may be involved; 10% present as a seropositive or seronegative for IgM rheumatoid factor. The monoarthritis of the knee or disease follows a relapsing and remitting course over many shoulder or with carpal tunnel years. Seropositive (plus anti-CCP) patients tend to develop syndrome. greater joint damage and long-term disability. They warrant Pain and stiffness is worse in the earlier and more aggressive treatment with disease-modifying morning, improves with gentle agents. activity; sleep is disturbed so pt ■ Rapidly progressive – The disease progresses remorselessly feels tired; limited ROM; muscle over a few years and leads rapidly to severe joint damage and wasting also; often a normocytic, disability. It is usually seropositive (plus anti-CCP), has a high normochromic anaemia incidence of systemic complications and is difficult to treat. Signs Early: inflammation but no joint damage; joint swelling. Look for tenosynovitis or bursitis Later: joint damage and deformity: ulnar deviation of the fingers and dorsal wrist subluxation, Boutonniere or swan neck deformity of fingers, z deformity of the thumb; hand extensor tendons may rupture; foot changes are similar Extra-articular: nodules on elbows, forearms or lungs; vasculitis; fibrosing alveolitis; pleural and pericardial effusions; Raynaud’s; carpel tunnel syndrome; peripheral neuropathy; splenomegaly; sleritis; osteoporosis; amyloidosis Screening questions Biological causes/risk factors ‘How long does it take to get going in the morning?’ Genetics: Genes: account for ~60% of disease susceptibility; strong association to HLA-DR4 and HLA-DRB1; familial pattern with high concordance in monozygotic twins (15%) Gender: women before the menopause 3x> men; after menopause, frequency between sexes same => suggests a role for sex hormones; the pill has no effect (though may delay onset of disease) Immunology: complex but chronic synovial inflammation is caused by ongoing T cell activation o Presence of activated T cells and macrophages and local production of rheumatoid factor autoantibodies in the joint in RA suggests that immune dysregulation plays a fundamental role in pathogenesis o Triggering antigen remains unclear: a. maybe the glycosylation pattern of Ig is abnormal in RA; little evidence that collagen type 2 is the triggering antigen but it is in animal models b. bacterial or slow viral infection, with subsequent maintenance of clonal B cell Pathology: Widespread persisting synovitis (inflammation of the synovial lining of joints, tendon sheaths or bursae). RF (autoAB with Fc portion of IgG as antigen) self-aggregate and form immune comples and result in synovitis (nb IgM, IgG, IgA RF exist) Production of rheumatoid factors in synovium by plasma cells key Synovium is usually thin but thickens in RA and becomes a palpable swelling around joints and tendons Synovium is infiltrated by a variety of inflammatory cells (polymorphs, lymphocytes, plasma cells) Vascular proliferation and ↑ permeability of blood vessels and synovial lining layer => effusions Synovium becomes hyperplastic and spreads from joint margins into cartilage surface = this ‘pannus’ of inflamed synovium damages underlying cartilage by blocking normal route for nutrition and direct effects of inflamm cells on chondrocytes Cartilage becomes thinned and underlying bones is exposed => juxta-articular bony erosions on XR. Erosions then lead to deformities Bloods: anaemia; ↑ ESR and CRP and are useful in monitoring treatment Serology: RF is +ve in 70% cases; citrullinated peptide antibodies (anti-CCP) are highly specific but not widely available. Note that the presence/absence of RF does not rule in/out disease but is a good predictor of prognosis; persistently ↑ titre in early disease implies more persistently active synovitis, more joint damage and ↑ disability eventually => earlier use of DMARDS; anti-CCP predictsdevelopment of erosions and a worse prognosis XR of the affected joint: establish a baseline; only soft tissue swelling is seen in early disease though Aspiration of the joint: if an effusion is present; would look cloudy due to presence of white cells Investigations e.g. to confirm diagnosis, exclude physical causes etc Management Treatment Biological e.g. specific drugs Treatment - Social Prognosis Complications The American College of Rheumatology (ACR) criteria: mainly for research, 4/7 needed: 1. Morning stiffness > 1 hour (for >6wks) 2. Arthritis of three or more joints (for >6wks) 3. Arthritis of hand joints and wrists (for >6wks) 4. Symmetrical arthritis 5. Subcutaneous rheumatoid nodules 6. A positive serum rheumatoid factor 7. Typical radiological changes (erosions and/or periarticular osteopenia) Refer to a rheumatologist for specialist treatment Pt reassurance: most go on to live a normal life esp with use of DMARDS; 25% will recover completely. No cure but many drugs available to prevent deterioration 1. Symptom control: NSAIDs and ‘coxibs’: do not reduce underlying inflammation; act via COX Night sedation may be needed Corticosteroids: slows the course of disease Intra-articular injections with semi-crystallline steroid, but these are short-lived Intramuscular depot injections (methylprednisolone) helps to control severe flare ups and possibly prophylactically eg before a holiday or after a life-event 2. Slow progression of RA: 3. DMARDs: mainly act through cytokine inhibition to ↓ inflammation, swelling and the development of joint erosions and irreversible damage; but they are slow-acting agents Sulfasalazine, Methotrexate, Leflunomide Biological DMARDs: TNF-α blockers: Etanercept, adalimumab, infliximab (mAB) Drugs not commonly used: IM gold; hydroxychloroquine (antimalarial); azathioprine; cyclosporine, penicillamine, Encourage regular exercise (in a hydrotherapy pool is popular); rest during active arthritis Surgery can be considered in severe cases to remove pain, improve ROM and prevent complications (ulnar stylectomy, joint replacements) A poor prognosis is indicated by: ■ A clinical picture of an insidious rather than an explosive onset of RA, female sex, increasing number of peripheral joints involved and the level of disability at the onset. ■ Blood tests showing a high CRP/ESR, normochromic normocytic anaemia and high titres of anti-CCP antibodies and of rheumatoid factor. ■ X-rays with early erosive damage (N.B. ultrasound and MRI can show cartilage and bone damage prior to conventional X-rays). Septic arthritis Amyloidosis: resembles RA and often associated with CTS and subcutaneous nodules Disorder How common is it Screening questions to ask Biological causes/risk factors Low back pain Very common + self-limiting but there are many red flags due to malignancy, infection, inflammation; pts visit a physio more often; Chronic back pain = cause of 14% of long-term disability in the UK 1. Onset: sudden or related to trauma? 2. Motor or sensory symptoms? 3. Is the bladder or bowel affected? 4. Is there sciatica? True sciatica radiates into the buttock, back of the thigh, below knee and into calf and ankle; caused by sciatic nerve irritation due to prolapsed disc Often traumatic and work-related Age-related: 15-30yo: prolapsed disc, trauma, fractures, ankylosing spondylitis, spondylolisthesis (a forward shift of 1 vertebra over another), pregnancy 30-50yo: degenerative spinal disease, prolapsed disc, malignancy (primary or secondary from: lung, kidney, thyroid, breast, prostate) >50yo: degenerative, osteoporotic vertebral collapse, paget’s, malignancy, myeloma, spinal stenosis, Very rare: cauda equine tumours, spinal infection (discitis, usually Staphylococcal but can be E. coli, TB, S typhi; often no systemic signs Red flags: think of SOCRATES! 1. Site: Thoracic back pain (most is lumbar)/ spinal process pain; MSK back pain is well localised; ankylosing spondylitis typically occurs over the sacroiliac joints and in the buttocks; pain due to an osteoporotic crush fracture us localised to a single vertebral level; root affected by prolapsed disc determines distribution of pain 2. Onset: Age <20 and >55yo; Acute onset in elderly; ankylosing spondylitis occurs in late teenage years or 20s; acute disc prolapsed often dramatic onset during lifting, bending or twisting movement or even after prolonged sitting (car/airplane); crush fractures also sudden events after a fall for example 3. Character: Constant or progressive pain 4. Radiates: down leg? Prolapsed lumbar disc pain radiates into buttock and down one leg; thoracic crush fracture radiates around the ribs and into the abdomen; spinal or root canal stenosis causes buttock and bilateral leg pain 5. Associated symptoms: Fever, night sweats, weight loss; Neurological disturbance; Sphincter disturbance; Bilateral or alternating symptoms; Leg claudication (spinal stenosis); Current or recent infection Any numbness, paralysis or funny sensations in your legs? => weak legs = cord compression Lumbar disc prolapsed causes paraesthesiae and numbness usually in one leg; spinal or root canal stenosis causes bilateral paraesthesiae and numbness; spinal cord compression causes paralysis and is a medical emergency i. Rapidly progressing cord compression is an emergency; arm weakness (suggests cervical cord compression); bladder and anal sphincter involvement is a late presentation; Signs: check motor and sensory sensations + reflexes: normal above level of lesion, LMN signs at the level, UMN signs below the lesion; DD: 2° malignancy (breast, lung, prostate) commonest; rarer = epidural abscess, haematoma, intrinsic cord tumour, atlanto-atlas subluxation; do MRI if any doubt Any sharp shooting pain in legs? Do you still have control over your bowels? Any incontinence? Signifies spinal cord compression and is a medical emergency Can you still feel your bottom when you go to the toilet? (anal sensation) Any eye problems in the past? Ankylosing spondylitis associated with anteruir uveitis = eye pain and blurred vision 6. Timing: Nocturnal pain (tumour) or morning stiffness: inflammatory arthritis (ankylosing spondylitis), infection or spinal tumour may be cause 7. Exacerbating/relieving: Increased pain on being supine; ankylosing spondylitis and polymyalgia rheumatic usually have pain worse in mornings and relieved by exercise/movement; mechanical pain is aggrevated by movement; position makes a lot of difference to back pain but not that of bone disease; pain and muscular spasm caused by prolapsed disc is worse when sitting; symptoms of spinal canal stenosis are relieved by rest and bending forwards as that opens up the canal 8. Severity: any pain that is not relieved by analgesics 9. Others: Hx of malignancy; Immunosuppression: steroids/HIV; Abdominal mass 10. ROS: ask about depression 11. PMH: RA (can affect cervical spine), infection, TB (can lead to wedge fractures or complete vertebral collapse ‘Pott’s disease of the spine’), osteoporosis (↑ risk of fractures), malignancy (Ca, leukaemia, myeloma can infiltrate the spine and cause unremitting back pain) Yellow flags: psycho-social RF for developing persistent chronic pain and long-term disability Belief pain and activity are harmful so have sickness behaviours (extended rest) Social withdrawal Emotional problems: low mood, depression, anxiety, stress Problems with work, or compensation due to being off work Overprotective family or no support at all Inappropriate expectations of treatment so low active participation in it Investigations e.g. to confirm diagnosis, exclude physical causes etc Management e.g. overall plans, referrals to other services Treatment Biological e.g. specific drugs Treatment Psychological Complications Mechanical Inflammatory Trauma Infective lesions of the spine Muscular and ligamentous pain Ankylosing spondylitis/sacroiliitis (see p. 532) Fibrositic nodulosis Metabolic Postural back pain (sway back) Osteoporotic spinal fractures (see p. 561) Lumbar spondylosis Osteomalacia (see p. 567) Facet joint syndrome Paget’s disease (see p. 565) Lumbar disc prolapse Neoplastic Spinal and root canal stenosis Metastases Spondylolisthesis Multiple myeloma Disseminated idiopathic skeletal hyperostosis Primary tumours of bone (DISH) Referred pain Fibromyalgia, chronic widespread pain (see p. 516) CT spine only if pain presents with red flags (vertebral collapse, spondylolisthesis) MRI is preferable to CT scanning when neurological signs and symptoms are present (prolapsed disc, cord compression, cancer, infection, inflammation (sacroilitis) Bone scans are useful in infective and malignant lesions but are also positive in degenerative lesions. Full blood count, U and E, LFTs, ESR and CRP are required only when red flags present CRP: malignancy (tumour, myeloma), infection or a metabolic cause. ALP: Paget’s PSA? Most back pain presenting to a primary care physician needs no investigation. Pain between ages 20-55yo can be treated with analgesia, brief rest if necessary and physiotherapy Pts should stay active within their limits of pain Early treatment of an acute episode prevents likelihood of developing long-term back pain Physical manipulation of uncomplicated back pain = short-term relief and pt satisfaction Analgesia (NSAIDS, paracetamol and codeine) Returning to work/activities better than bed rest Avoid precipitants and seek physio if not improving If no serious pathology: education and encouragement as most are self-limiting Address psych-social issues Neurological emergencies: 1) acute cauda equina compression: alternating or bilateral root pain in legs; saddle anaesthesia, loss of anal tone on PR, bladder +/- bowel incontinence 2) acute cord compression: bilateral pain, LMN signs at level of compression, UMN and sensory loss below, sphincter disturbance a) Causes: for both = bony mets, large disc protrusion, myeloma, cord or paraspinal tumour, TB, abscess Nerve root lesions: Nerve Pain Weakness Reflex root change L2 Across upper thigh Hip flexion, adduction None L3 Across lower inner thigh Hip adduction, knee extension Knee L4 Knee to medial malleolus; inner calf Knee extension, foot inversion and Knee dorsiflexion L5 Lateral shin to dorsum of foot and big Hip extension and abduction None toe; outer calf Knee flexion Foot and big toe dorsiflexion S1 Posterior calf to lateral foot and little toe Knee flexion Ankle Foot and toe plantar flexion Foot eversion Neck lumps Disorder– core How common is it Who does it affect Core symptoms and signs Biological causes/risk factors Investigations Management e.g. overall plans, referrals to other services Prognosis Acute lymphoblastic leukaemia (ALL): malignancy of lymphoid cells, affecting either B or T cells, arresting maturation and promoting uncontrolled proliferation of immature blast cells, with bone marrow failure and tissue infiltration. Commonest cancer of childhood Children, rare in adults Marrow failure: anaemia (↓Hb) = tiredness, SOBOE, infection (↓WCC = leucopenia), bleeding (↓ platelets = thrombocytopenia) Infiltration: hepato-, splenomegaly, lymphadenopathy, orchidomegaly, CNS involvement – bulbar palsies, meningism, bilateral parotid swelling, bone pain Common infections: chest, mouth, perianal, skin, bacterial septicaemia, Zoster, CMV, measles, candidiasis, PCP Ph chromosome: CNS involvement, WCC ↑ ↑ Signs: pallor fever (due to infection, not the disease itself) petechiae, purpura, bruises, fundal haemorrhage lymphadenopathy, hepatosplenomegaly violaceous skin lesions (acute myelomonocytic leukaemia) Thought to develop from an environmental trigger in the presence of genetic susceptibility = unknown but RF are X-rays during pregnancy, and syndromes inc Down’s syndrome. Classification: Morphological: FAB (French, American, British) system divides ALL into L1, L2, L3 by microscopy Immunological: surface markers divide ALL into precursor B-cell ALL, T-cell ALL, B-cell ALL Cytogenetic: chromosomal analysis; abnormalities detected in most cases, 85% of which are translocations eg Philidelphia chromosome Bloods: blast cells on film, WCC usually ↑, Hb and platelets ↓ Blood film: blast cells seen CXR, CT: mediastinal widening or abdominal lymphadenopathy Lumbar puncture: to analyse CSF; ?CNS involvement; done when blasts cleared from peripheral blood Bone marrow aspirate: ↑ cellularity, ↓ erythropoiesis and megakaryocytes, sometimes trilineage dysplasia. Replacement by blast cells > 20% (often approaching 100%) 1. Untreated: invariably death within months 2. Supportive care: blood/ platelet transfusion, IV fluids and allopurinol to prevnt tumour lysis 3. Infections: dangerous due to neutropenia; immediate IV Abx; ?prophylactic Abx/antivirals 4. Chemotherapy: pts usually entered in to trials; a typical programme involves elements of: remission induction, consolidation, CNS prophylaxis, maintenance 5. Marrow transplant: if poor prognosis or relapse; only cure for Philidelphia chromosome t(9;22)(q34;q11) 6. Palliative Haematological remission: no evidence of leukaemia in the blood, a normal or recovering BM, and <5% blasts in normal regenerating BM Cure rates = 70-90% for children, 35% for adults (<5% if >65yo) Disorder– core How common is it Who does it affect Core symptoms Signs Chronic lymphocytic leukaemia (CLL): monoclonal proliferation of non-functional mature B-cells (T-cell CLL = 5% cases) CLL = 25% of all leukaemias therefore commonest of all of them M 2x> F; disease of the elderly where median age of diagnosis is 65yo None in 25%; infection due to functional leucopenia and immune failure (↓ Ig), anaemia due to haemolysis or marrow infiltration, painless lymphadenopathy, weight loss, sweats, anorexia (ie bone marrow suppression and infection), LUQ discomfort due to splenomegaly Enlarged bilateral rubbery, non-tender cervical lymph nodes (lymphadenopathy), splenomegaly, hepatomegaly Biological causes/risk factors Investigations Management e.g. overall plans, referrals to other services Stage 0 1 2 3 4 Lymphocytosis (L) alone (L) + lymphadenopathy (L) +spleno, hepatomegaly (L) + anaemia (L) + platelets (<100x109/L) Median survival >13years 8 5 2 1 Bloods: ↑ lymphocytes; later – autoimmune haemolysis, marrow infiltration: ↓ Hb, neutrophils, platelets Blood film: small or medium-sized lymphocytes; may be smudge cells in vitro Bone marrow: reflects peripheral blood with ↑ lymphocytes Immunophenotyping: CD19, 5, 23 Cytogenetics/ FISH: not essential but may help in assessment of prognosis Some remain in status quo for years, some regress; most usually grow and cause obstruction; death is usually due to infection (pneumococcus, haemophilus, meningococcus, Candida, aspergilliosis) Asymptomatic: monitor; chlorambuci ↓ lymphocyte count, improve marrow function Radiotherapy: for relief or lymphadenopathy or splenomegaly Supportive care: transfusions, IV human Ig if recurrent infection Prognosis is good depending on stage = ~10 years Biological causes/risk factors Chronic myeloid leukaemia (CML): uncontrolled clonal proliferation of myeloid cells (ie myeloproliferative) Accounts for 15% of leukaemias Unlike the acute leukaemias which are either rapidly reversed or rapidly fatal, CML has a more slowly progressive course which if not initially cured will be followed eventually by blast crisis (90% myeloid, 20% lymphoid) or myelofibrosis and death after 3–4 years. 40-60yo, with slight male predominance Chronic and insidious; weight loss, tiredness, SOBOE, fever and sweats in the absence of infection; features of gout (due to purine breakdown), bleeding and abdominal discomfort (splenomegaly) Splenomegaly (>75%) – often massive; hepatomegaly, anaemia = pallor, bruising; lymphadenopthy is uncommon unless during blast crisis; retinal haemorrhage due to leucostasis Philadelphia chromosome is present in >80% cases, forms a fusion gene BCR/ABL on chromosome 22 which is a tyrosine kinase that is unregulated Investigations Disorder– core How common is it Who does it affect Core symptoms Signs Treatment Prognosis Bloods: WBC ↑ ↑ with the whole spectrum of myeloid cells (neutrophils, myelocytes, basophils, eosinophils); ↓ Hb, platelets variable, ↑ urate or B 12; cytogenetic analysis of blood (or bone) shows Ph chromosome Blood film: neutrophilia of whole spectrum of myeloid precursors and some blasts; elevated basophils and eosiinophils Bone marrow aspirate: ↑ cellularity and myeloid precursors FISH: used to demonstrate cytogenetic abnormality and quantitatively monitor response to therapy. Chemotherapy: Glivec (imatinib) Stem cell transplant: using HLA matched sibling or unrelated person is the only curative treatment but carries high mortality Variable; median survival 5 years; 3 phases: 1. Chronic: lasting a few months or years of few/ no symptoms 2. Accelerated phase: ↑ symptoms, splenomegaly 3. Blast transformation: features of acute leukaemia with death looming Disorder– core How common is it Who does it affect Core symptoms Biological causes/risk factors Investigations Acute myeloid leukaemia (AML): proliferation of blast cells derived from myeloid elements of bone marrow 1/10,000/year; ↑ with age Commonest acute leukaemia in adults; seen increasingly as a complication of chemotherapy eg for lymphoma Marrow failure: anaemia, infection, bleeding; DIC in a specific subtype where there is release of thromboplastin Infiltration: hepato-, splenomegaly, gum hypertrophy, skin involvement, CNS involvement (rare presentation in AML) Morphological classification: based on WHO criteria; 5 subtypes => v complex AML with recurrent genetic abnormalities AML multi-linear dysplasia AML therapy indicated AML of ambiguous lineage AML, other Bloods: WCC ↑ often; blast cells few in peripheral blood so diagnosis depends on bone marrow biopsy; differentiation from ALL by microscopy (Auer rods in AML = crystals of coalesced granules) Prognosis Very rapidly progressing malignancy: death in 2months if untreated; 20% 3year survival after chemotherapy Treatment Biological e.g. specific drugs Complications Supportive care: as for ALLL Chemotherapy: Bone marrow transplant: pluripotent haematopoietic stem cells are collected from BM = allogenic transplants (ie destroy pt’s IS with drugs and then give HLA-matched stem cells); problems = graft vs host disease, opportunistic infection, relapse, infertility Infection is major problem eg septicaemia; AML causes fever anyway! Acute leukaemias ↑ in incidence with age Acute leukaemia generally come on quickly, and you either get better quickly or die quickly. Disorder– core How common is it Who does it affect Core symptoms Signs Biological causes/risk factors Hodgkin’s lymphoma: malignant proliferation of lymphocytes Rare; incidence of 3/100,000 M 1.3x> F; >90% in adults between 16-65yo with peak incidence in 30s and elderly Cervical lymph node enlargement, painless, rubbery, contiguous pattern of spread (also found in axillary or inguinal lymph nodes); may ↑ or ↓ in size spontaneously Hepato or splenomegaly Systemic ‘B’ symptoms: fever (25%), drenching night sweats, weight loss of >10% bodyweight 25% have constitutional symptoms: pruritis, fatigue, anorexia, alcohol-induced pain at the site of the enlarged lymph nodes Mediastinal lymph node involvement = cough, breathlessness, SVC obstruction Lymph node enlargement, cachexia, anaemia, spleno or hepatomegaly Malignant proliferation of lymphocytes that accumulate in lymph nodes = lymphadenopathy, but may also be found in peripheral blood or infiltrate organs. Cells with mirror-image nuclei = Reed-Sternberg cell Epidemiological linking links previous infective mononucleosis with HL and upto 40% of pts have ↑ titres of EB AB at the time of diagnosis and several years prior to the clinical development of HL. => EBV has a role in pathogenesis Pathology: Hallmark = presence of clonal malignant Reed–Sternberg cell in a lymph node biopsy. CD30 and CD15 are almost always expressed in the majority of cases of classical HL. Several pathways may lead to HL but ultimately B-cells not expressing Ig somehow escape apoptosis. WHO Classification: Classical HL = 95% cases can be divided into 4 subtypes: Nodular sclerosing HL: (70%) nodular growth pattern with many fibrotic bands present; seen in young adults, M=F; cervical, supraclavicular and anterior mediastinal lymph nodes Lymphocyte-rich HL: (5%) characterised by aninfiltrate of many small lymphocytes and Reed– Sternberg cells; occurs in peripheral lymph nodes; indolent disease presenting at ↑ median age. Mixed cellularity HL: (25%) mixed cellularity with lymphocytes, eosinophils, neutrophils and histiocytes. Reed–Sternberg cells are present but no fibrotic bands. M>F; B symptoms present Lymphocyte-depleted HL: (rare) lack of cellular infiltrate with numerous Reed–Sternberg cells; presents with advanced stage and B symptoms. It is seen in HL associated with HIV. Investigations e.g. to confirm diagnosis, exclude physical causes etc Management Complications In addition to classical HL, nodular lymphocyte-predominant HL (5% of cases) contains malignant L and H cells (lymphocytic and/or histiocytic Reed–Sternberg cell variants, also called ‘popcorn’ cells) which are positive for CD20, CD45, BCL6, CD79a without expressing CD15 or CD30. Lymph node biopsy: definitive diagnosis Bloods: FBC (?normocytic normochromic anaemia), U and E (↑ ESR, ↑ LDH due to release during ell turnover), LFT (often abnormal with or without liver involvement), uric acid is often ↑ CXR: mediastinal widening with or without lumg involvement CT scan: indicates intrathoracic nodes in 70%; investigation of choice for staging cancer Ann-Arbor Staging: I: confined to a single lymph node II: 2 or more nodes on the same side of the diaphragm III: involvement of nodes on both sides of the diphragm IV: spread beyond the nodes to liver or bone or marrow Divided in to A and B: A = absence of symptoms (other than pruritis) B = symptoms present: weight loss >10% in 6 months, unexplained fever >38°C, drenching night sweats Nb extra-nodal extension does not advance the stage but is indicated with a subscript ‘E’ Radiotherapy: for IA and IIA Chemotherapy: for more advanced stages; standard regime =’ABVD’ (adriamycin, bleomycin, vinblastine, dacarbazine) Radiotherapy may ↑ solid tumour risk, lung fibrosis, hypothyroidism, IHD Chemotherapy may cause myelosuppression, non-Hodgkin’s, alopecia, AML, nausea, infection 5 year survival: depends on stage and grade: 95% in I-A lymphocyte-predominant; <40% IV-B lymphocyte-depleted Disorder– core How common is it Who does it affect Core symptoms and signs Biological causes/risk factors Non-Hodgkin’s: malignant tumour of lymphoid cells; 70% are B cell origin; 30% are T cell origin 15/100,000 in developed countries ; ↑ over last 20-30years for some reason; M>F slightly Peripheral lymphadenopathy: 75%, painless, superficial Extranodal presentation: 25%, more common than in HL, involves GIT, brain, lung, tests, thyroid and skin; oropharyngeal involvement is rare but presents as sore throat and obstructed breathing (Waldeyer’s ring) Systemic symptoms (B symptoms): fever, night sweats and weight loss; less common than in HL Pancytopenia: due to involvement o fthe BM: anaemia, infection, bleeding Cause unknown; wide geographical variation = ?environmental factors EBV DNA is observed in 20% tumours and associated with Burkitt’s lymphoma Human T cell lymphocytic virus Herpes virus 8 ↑ in infection in those with HIV Helicobacter pylori is an aetiological factor in gastric MALT lymphoma. Farming and NHL - ?pesticide exposure Pathogenesis: Malignant clonal expansion of lymphocytes which occurs at different stages of lymphocyte development. o neoplasms of non-dividing mature lymphocytes are indolent o neoplasms of proliferating cells (e.g. lymphoblasts, immunoblasts) are much more aggressive Malignant transformation due to errors in gene rearrangements which occur during the class switch, or gene recombinations for immunoglobulins and T cell receptors. Burkitt’s lymphoma: childhood disease with characteristic jaw lymphadenopathy; translocation between chromosomes 8 and 14 in which the myc oncogene moves from chromosome 8 to a position near the constant region of the immunoglobulin heavy chain gene on chromosome 14, resulting in upregulation of myc. Investigations Management e.g. overall plans, referrals to other services Prognosis Classicifaction: ever-changing but based on WO criteria (2001) Previous classifications = indolent (or low grade) and aggressive (or high grade) = also in OHCM 1. Low-grade: indolent and incurable, widely disseminated at presentation a. Include: follicular lymphoma, marginal zone lymphoma (inc MALT lymphomas), lymphocytic lymphoma, lymphaplasmacytoid lymphoma 2. High grade: more aggressive but long-term cure; Hx of rapidly enlarging lymphadenopathy with systemic B symptoms a. Include: Burkitt’s lymphoma, lymphoblastic lymphoma, diffuse large B-cell lymphoma Same as for HL! Depends on subtype: Low-grade: if symptomless, none may be needed; radiotherapy if localised disease High-grade: ‘CHOP’ regime (cyclophosphamide, hydroxydaunorubicin, vincristine (oncovin), prednisolone) + rituximab, an antiCD20 mAB Worse if at presentation: >60yo, systemic symptoms, abdominal mass >10cm, ↑ LDH, disseminated disease, 30% 5 year survival for high-grade, 50% for low grade Disorder– core How common is it Classification Who does it affect Core symptoms Signs Features/ symptoms of presentation in a primary care setting Biological causes/risk factors Investigations Goitre Can be felt in up to 9% of population Thyroid cancers: ¾ affect women, presenting initially as thyroid nodules, 400 deaths annually in UK Most commonly recognised by friends and family as a cosmetic defect; majority painless; large goitres can cause dysphagia and difficulty breathing = compression of oesophagus or trachea. A small goitre may be visible on swallowing (note size, shape, consistency, mobility and whether a lower edge can be palpated. Ask about medications (esp iodine-containing preparations) and radiation exposure Puberty and pregnancy may produce a diffuse increase in size of the thyroid. Pain in a goitre may be caused by thyroiditis, bleeding into a cyst or (rarely) a thyroid tumour. Excessive doses of carbimazole or propylthiouracil will induce goitre. Iodine deficiency and dyshormonogenesis (see above) can also cause goitre. Questions to ask: 1. Is thyroid smooth or nodular? 2. Is the pt euthyroid, thyrotoxic or hypothyroid? a. Smooth, non toxic goitre: Endemic (iodine deficiency); congenital; tyroiditis; physiological; Hashimoto’s thyroiditis; b. Smooth, toxic: Graves’ disease 3. Any nodules? Many or one? If >4cm = likely to be cancer Diffuse: Simple: no clear cause; usually smooth and soft;?ass with thyroid growth stimulating Ab Autoimmune: Hashimoto’s thyroditis and thyrotoxicosis (Graves disease) are both ass with a firm, diffuse goitre of variable size Thyroiditis: acute tenderness/pain in a diffuse swelling = acute viral thyroiditis (de Quervain’s disease). May produce transient clinical hyperthyroidism with a serum ↑ in T4. Nodular: Multinodular: most common, esp in older people; pt is usually euthyroid; may cause oesophageal or tracheal compression and laryngeal palsy (hence coarse) Solitary: Single thyroid lump: common problem but difficult in diagnosis – should always be treated as malignant (5% risk), though the majority of these are cysts, adenoma, benign (and probably the largest nodule of multinodular thyroid) or malignant Fibrotic: (Reidel’s thyroiditis): rare, produces a ‘woody’ gland, irregular and hard so difficult to differentiate between malicnancy; ass with systemic symptoms of inflammation and ↑ inflammatory markers Malignancy: rapid enlargement, ass lymph node involvement, painful; RF = previous irradiation, lonhstanding iodine deficiency and a Fx. Lung and bones are most common sites for metastases. Cell type Papillary Frequency 70% Behaviour Young people Follicular 20% Middle-aged, F>M Medullary 5% Anaplastic Lymphoma <5% 2% Familial (MEN syndrome) or sporadic 80% F:M 3:1; elderly F:M 3:1; elderly Spread Local nodes, lung and bone; good prognosis esp If young Mets to bone/ lung early via blood; good prognosis if resectable May produce calcitonin; local and mets; poor prognosis V poor prognosis; Present with stridor or dysphagia; aggressive; ?responsive to radiotherapy Anterior triangle: Submandibular region: submandibular stones Pulsatile: carotid aneurysm; tortuous carotid artery; chemodectoma Non-pulsatile: o Midline: dermoid cyst; thyroid goitre; thyroglossal cyst; pharyngeal pouch o Not-n-midline: brachial cyst Posterior triangle: Cystic hygroma Cervical rib Subclavian artery aneurysm Pancoast’s tumour Thyroid function tests – TSH plus free T4 or T3. e.g. to confirm diagnosis, exclude physical causes etc Management e.g. overall plans, referrals to other services Treatment Biological e.g. specific drugs Disorder– core Biological causes/risk factors Thyroid antibodies – to exclude autoimmune aetiology. Ultrasound with fine needle aspiration = (cytology) – good for demonstrating cystic or solid lumps; multinodular thyroid may be demonstrated if only a solitary nodule can be palpated. FNA has a 5% false-negative rate Chest and thoracic inlet X-rays to detect tracheal compression and large retrosternal extensions in patients with very large goitre or clinical symptoms. Thyroid scan (125I or 131I) can be useful to distinguish between functioning (hot) or nonfunctioning (cold) nodules. A hot nodule is only rarely malignant; however, a cold nodule is malignant in only 10% of cases and FNA has largely replaced isotope scans in the diagnosis of thyroid nodules. Indications for surgery: 1. If possibly malignant/ pt considers FNA false-negative rate high 2. Cosmetic reasons 3. Compressive effects on oesophagus or trachea Papillary and Follicular (differentiated): thyroidectomy (total/partial) with radioactive iodine (RAI) ablation of residual thyroid post-op; pts are treated with suppressive doses of levothyroxine = T4 (suppress TSH) Anaplastic (undifferentiated): do not respond to RAI and external radiotherapy only offers brief respite. Medullary (MTC): arise from calcitonin-producing C cells; ass with multiple endocrine neoplasia type 2 (MEN2); 25% pts diagnosed with MTC have RET protoncogene mutation = genetic and family screening ?necessary; perform phaeochromocytoma screen pre-op; total tyroidectomy and wide lymph-node excision needed; tumour invasion likely. Most tumours are minimally active hormonally (but may produce thyroglobulin which can be detected and used as a tumour marker to guide risk of recurrence) Parotid and salivary gland selling Localised: pleiomorphic adenoma; Warthin’s tumour; adenocarcinoma; SCC; lymphoma; Generalised: mumps; sarcoid; bacterial infection; CLD; Sjogren’s syndrome; Meckuliz syndrome Neurological Disorder– core How common is it Classification Who does it affect Core symptoms Stroke and TIA; rapid onset of a cerebral deficit (usually focal) lasting >24hrs (stroke) or <24hrs (TIA), with no cause apparent other than a vascular one (TIA also results in complete recovery too) 2nd commonest cause of death (9%) world-wide; ~2/3 of global burden of strokes is in middle and lowincome countries; age-adjusted annual death rate from strokes is 200/100,000 in the UK (12% of all deaths); Uncommon if <40yo, M>F, rates greater in Asian and black Africans than Caucasians Cerebral infarction: Cerebral hemisphere infarct (50%) Variable, depending on site and extent. Following vessel obstruction, brain ischaemia occurs, then infarction. The infracted area is surrounded by a swollen area which is structurally intact but does not function (ischaemic penumbra) – this can regain neurological function. Within this ischaemic area, hypoxia => fall in ATP => glutamate release => Ca2+ channels open => free radical release => inflammation and necrosis Ant cerebral art.:supplies frontal and medial part of cerebrum; occlusion = weak, numb contralateral leg +/-similar arm symptoms; face spared Middle cerebral artery/internal carotid artery block:supplies lateral part of hemispheres: contralateral hemiplegia or hemiparesis with facial weakness, contralateral sensory loss, contralateral homonymous hemianopia (due to involvement of optic radiation), dysphasia usual when the dominant hemisphere is affected, visuo-spatial disturbance (can’t dress, gets lost) when non-dominant hemisphere is affected; weak limbs are at first flaccid and areflexic; headache unusual; consciousness preserved; after a number of days, reflexes return and become exaggerated (spastic); extensor plantar response appears; weakness recovers over days/months/years. Posterior cerebral art.: supplies occipital lobe; contralateral homonymous hemianopia with maculasparing Brainstem infarction (25%) Complex signs depending on relationship to CN nuclei, long tracts and brainstem connections Clinical feature Structure involved Hemiparesis or tetraparesis Corticospinal tracts Sensory loss Medial lemniscus and spinothalamic tracts Diplopia Oculomotor system Facial numbness Vth nerve nuclei Facial weakness VIIth nerve nucleus Nystagmus, vertigo Vestibular connections Dysphagia, dysarthria IXth and Xth nerve nuclei Dysarthria, ataxia, hiccups, vomiting Brainstem and cerebellar connections Horner’s syndrome Sympathetic fibres Coma, altered consciousness Reticular formation Locked-in syndrome caused by upper brainstem infarction Lateral medullary syndrome (occlusion of posterior inferior cerebellar artery thrombosis, vertebral art. and Wallenberg’s syndrome) is an eg of brainstem (lateral medulla and inferior cerebellar surface) infarction that presents as vertigo with other cerebellar signs: Ipsilateral: Facial numbness (Vth) Contralateral: Diplopia (VIth) Spinothalamic sensory loss Nystagmus Hemiparesis (mild, unusual) Ataxia (cerebellar) Horner’s syndrome IXth and Xth nerve lesions Lacunar infarct (25%) Small, <1.5cm, infarcts seen on MRI or at autopsy; hypertension commonly present; signs: pure motor stroke, pure sensory stroke, sudden unilateral ataxia and sudden dysarthria with a clumsy hand; may even be symptomless Others: Multi-infarct (vascular) dementia:multiple lacunes cause generalised intellectual loss seen with advanced cerebrovascular disease, with dementia in late stages Hypertensive encephalopathy: due to cerebral oedema causing severe headaches, nausea and vomiting; agitation, confusion, fits and coma if not treated; papilloedema develops following brain swelling due to multiple acute infarcts Visual cortex infarct: posterior cerebral infarct or MCA macular branch infarct =>hemianopic visual loss and cortical blindness Watershed infarct: following long periods of low perfusion, infarcts occur between areas supplied by anterior, middle or posterior cerebral arteries; cortical visual loss, memory loss, intellectual impairment common TIA: diagnosis is based on clinical history Sudden loss of function, within seconds, lasting for mins-hours (<24hrs). Site determined by type of attack: carotid/anterior circulation (TACI):amaurosisfugax, aphasia, contralateral hemiparesis or hemisensory loss, homonymous hemianopic visual loss verterbrobasilar/posterior circulation:diplopia, vertigo, nystagmus, vomiting, choking, dysarthria, ataxia, hemisensory loss, hemianopic visual loss, bilateral visual loss, tetraparesis, LOC (rare), transient global amnesia, deafness, tinnitus, cerebellar symptoms Amaurosisfugax = sudden transient loss of vision in one eye due to passage of small emboli through the retinal arteries; often first sign of internal carotid artery stenosis Transient global amnesia = amnesia/confusion lasting several hours, followed by complete recovery Signs Biological causes/risk factors Intracranial haemorrhage: Intracerebral haemorrhage:rupture of micro-aneurysms (Charcot-Bouchard aneurysms); degeneration of small deep penetrating arteries; usually massive, often fatal and occurs in chronic hypertensive and well defined sites – basal ganglia, pons, cerebellum, subcortical white matter; tends to produce a headache (infarct doesn’t) but cannot tell the difference between infarct/haemorrhage at the bedside – haemorrhage seen on CT immediately as intraparenchymal, intraventricular or subarachnoid blood. Cerebellar haemorrhage: headache, often followed by stupor/coma and signs of cerebellar/brainstem origin (egnystagmus, ocular palsies). May cause acute hydrocephalus = emergency Subarachnoid haemorrhage:8/100,000/yr; spontaneous arterial bleeding into subarachnoid space and is usually clearly recognisable from its dramatic onset: sudden devastating headache, often occipital, followed by vomiting, collapse and coma; following major SAH there is neck stiffness (‘meningism’) and +veKernig’s sign (flex hip and knee to 90°, then extend leg at knee joint => pain in the back is +veKernig sign); papilloedema sometimes present Causes: Saccular (berry) aneurysms (80%): develop within the circle of Willis: Between posterior communicating and internal carotid artery (post communicating artery aneurysm) Between ant communicating and ant cerebral art. (ant communicating + ant cerebral art aneurysm) At the bifurcation of the MCA (MCA aneurysm) Arteriovenous malformation (15%):collection of arteries and veins of developmental origin; may rupture; form cavernous haemagiomas and can (rarely) bleed No cause in <15%; ass with SLE<coarctation of aorta, polcystic kidney disease, Marfans, Ehlers-Danlos Graded I-V: grade 1, no signs, 0% mortality; grade 2, neck stiffness + CN palsies, 11% mortality; grade 3, drowsy, 37% mortality; grade 4, drowsy with hemiplegia, 71% mortality; grade 5, coma, 100% mortality Subdural haematomas: (banana shape on CT): collection of blood in subdural space following rupture of a vein between cortex and venous sinuses (deceleration injury), often following a trivial head injury; time space between injury and symptoms may be days-weeks; headache, drowsiness, confusion common, consciousness fluctuates, seizures; as haematoma develops ICP ↑ and causes midline shift leading to tentorial coning; elderly at risk as brain atrophy makes veins more vulnerable; Extradural haemorrhage: (lemon shape on CT as tough dural attachments keep it more localised): follows a linear skull vault fracture in temporal or parietal bone near temple tearing a branch of the middle meningeal artery; accumulates over mins-hours; head injury with unconsciousness, followed by recovery (lucid interval) then rapid decline due to ↑ ICP with increasingly severe headache, vomiting, confusion, fits, ipsilateral dilated pupil and contralateral hemiparesis and brisk reflexes (and upgoing plantar) with rapid transtentorial coning; bilateral fixed dilated pupils, tetraplegia and respiratory arrest follow (becomes deep and irregular). Lumbar puncture contraindicated Hypertension is the most treatable risk factor Completed stroke causes: Thrombo-embolic infarction (80%); arterial thrombosis in-situ in atheromatous carotid, vertebral or cerebral arteries with subsequent infarction; arterial embolism from a distant site (heart (which follow AF, valvular disease, prosthetic valves, cardiac surgery or MI = mural thrombi), carotid, vertebral or basilar arteries) o Cardioembolic causes = >30% source of stroke = examine the heart! Cerebral and cerebellar intracranial haemorrhage (10%): high BP, trauma or aneurysm rupture Sub-arachnoid haemorrhage (5%) Carotid or vertebra artery dissection, ateriovenous malformations, venous infarction, polycythaemia and hyperviscosity syndromes, fat and air embolism (diving), MS, mass lesions (tumours, abscess, subdural haemorrhage) In young pts: thrombophillia, vasculitis, SAH, venous-sinus thrombosis, carotid artery dissection Completed stroke: deficit has become maximal, usually within 6hrs Stroke-in-evolution: describes progression during first 24hrs Minor stroke: pts recover without significant deficit, usually within a week TIA casues: Microemboli from the heart or atheromatous plaques Fall in cerebral perfusion (cardiac dyrhythmia, postural hypotension, ↓ flow due to atheromas) Risk Factors: Heart disease (valvular, ischaemic); PVD; carotid bruit, ↑ clotting Investigations e.g. to confirm diagnosis, exclude physical causes etc Thrombocythaemia and thrombophilia (protein C deficiency, factor V Leiden) are weakly associated with arterial stroke Anti-cardiolipin and lupus anticoagulant antibodies (antiphospholipid syndrome, p. 544) predispose to arterial thrombotic strokes in young patients. Endocarditis (p. 769) – thromboembolic stroke may be the presenting feature. Low-dose oestrogen-containing oral contraceptives (the pill) do not increase stroke risk significantly in healthy women but probably do so with other risk factors, e.g. uncontrolled hypertension or smoking. Migraine is a rare cause of cerebral infarction (p. 1136). Vasculitis (systemic lupus erythematosus (SLE), polyarteritis, giant cell arteritis, granulomatous CNS angiitis) is a rare cause of stroke. Amyloidosis can present as recurrent cerebral haemorrhage (p. 1072). Hyperhomocysteinaemia predisposes to thrombotic strokes. Folic acid therapy does not reduce the incidence. Neurosyphilis, SLE, mitochondrial disease. Drugs of abuse e.g. cocaine, and possibly over-the counter cold remedies containing vasoconstrictors. Cox-2 inhibitors are associated with a slightly ↑ incidence of stroke (p. 517). Four extracranial sites for stenoses and plaques: origin of common carotid artery (1) origin of internal carotid artery (2) origin of vertebral artery (3) subclavian artery (4) and carotid artery syphon – within the cavernous sinus. To confirm clinical diagnosis and differentiate between haemorrhage and infarct To look for underlying causes and to direct therapy To exclude other causes eg tumour Search for sources of embolism (carotid bruit (setnosis), AF, valve lesion, evidence of endocarditis, previous emboli or TIA), recent MI, >20mmHg difference between right and left brachial BP (subclavian stenosis) An underlying condition may be evident: atheroma, hypertension, postural hypotension, bradycardia or low cardiac output, diabetes mellitus Management e.g. overall plans, referrals to other services Treatment Biological e.g. specific drugs Treatment Psychological Treatment - Social Prognosis Differential diagnosis CT and MRI: (CT more widely available) Non-contrast CT: will demonstrate haemorrhage but not cerebral infarct initially MRI: will indicate early infarct and a later MRI will identify penumbra Diffusion-weighted MRI (DWI): will identify infarct immediately as well as haemorrhage Do CT first, if no haemorrhage, then give thombolytic drugs Immediate management: 1. Admit to a multidisciplinary stroke unit 2. General medical measures: Airway – confirm patency and monitor O2 by mask Monitor BP Look for sources of emboli Assess swallowing (SALT; speech and language therapy) 3. Is thrombolysis needed? If yes, immediate imaging needed 4. Brain imaging – CT commonly used more 5. Cerebral infarction: CT excludes haemorrhage, give immediate thrombolytic therapy, or 300mg aspirin if contraindicated 6. Cerebral haemorrhage: give no anti-coagulants; neurosurgery may be needed (decompressivehemicraniectomy reduces ICP Later management: 1. MR angiography (MRA) or CT angiography: if suspect anterior circulation TIA; to confirm surgically accessible arterial stenoses. If US suggests carotid stenosis, normotensive pts should with TIA/stroke in ant circulation should have vascular imaging. 2. Carotid Doppler and duplex scanning: screen for carotid and vertebral stensoes and occlusion Low-dose aspirin as primary prevention if 10-year risk of CHD >10%; risk on stroke prevention is unclear 1. Risk factors should be identified and reduced. 2. Anti-hypertensive therapy: major factor in primary and secondary stroke prevention; transient raised BP, often seen following strokes, does not need control unless diastolic >100mmHg 3. Anti-platelet therapy: long-term soluble aspirin (75mg/day) reduces risk of further thromboembolic infarction; clopidogrel and dipyridamole are also used: reduce platelet aggregation 4. Anti-coagulants: heparin and warfarin: given when AF or cardiac valve lesion or cardiomyopathies. Brain haemorrhage must be excluded by CT/MRI 5. Surgery: internal carotid endarterectomy: recommended if internal carotid stenosis >70%. Successful surgery reduces risk of further TIA/stroke by <75%. Endarterectomy has a mortality of 3%, and a similar risk of stroke. For SAH, dexamethasone is prescribed to reduce cerebral oedema and ?stabalise the BBB; ?repeat CT if deteriorating; craniotomy and clipping aneurysms; intraluminal platinum coils For SDH, irrigation via burr holecraniostomy, 2nd line is craniotomy. Address cause of trauma. For EDH, burr-holes relieve pressure created = life-saving Consider social isolation, pre-existing cognitive impairment, nutrition, skin and sphincter care, swallowing; unemployment, loss of independence, finance cost, loss of self-esteem => depression At home, aids and alterations may be needed: rails, hoists, sliding boards, modified sleeping arrangements, stair lifts, wheelchairs, electric blinds, doorways, flooring Physiotherapy: within first few weeks after stroke; relieve spasticity, prevent contractures and teach pts to use walking aids Speech therapists: swallowing may be unsafe due to risk of aspiration so NG(nasogastric) or PEG(percutaneous gastrostomy Occupational therapy TIA: after 5years, 30% have had a stroke, 30% of which occur in the first year; 15% have a MI; TIAS in anterior circulation are worse than posterior circulation ~25% of people die within 2 years of stroke, 10% within the first month. Of initial stroke survivors, 3040% are alive 3 years later 1/3 of survivors return to independent mobility and 1/3 have a disability that requires institutional care Nearly ½ of SAH cases are dead or moribund before reaching the hospital. TIA: focal epilepsy (though usually +ve symptoms present; limb jerking and LOC); migraine (though usually have a headache which is not present in TIA) CNS tumour; Todd’s palsy; migraine; hypoglycaemia; overdose; Subarachnoid Haemorrhage (SAH) Description Epidemiology Cause Risk Factors Symptoms Signs Differential diagnosis Complications Investigations Treatments Drugs Spontaneous bleeding into subarachnoid space. Prevalence: 9/100 000 Age groups: 35-65yrs Saccular (Berry) Aneurysms: (70%) develop on circle of Willis and adjacent arteries: between post comm & internal carotid; between ant comm & ant cerebral art; at bi/trifurcation of middle cerebral art. Assoc: polycystic kidneys, coarctation, Ehlers-Danlos. Arteriovenous Malformation (AVM): (10%) arteries and veins within a developmental origin. No lesion found: (20%) Smoking; alcohol misuse; BP↑; bleeding disorders; mycotic aneurysm; ?post-menopausal (↓oestrogen correlates with ↑ incidence ♀:♂ 3:2 >45yrs ); FHx. Presentation Sudden thunder clap, devastating occipital headache (within seconds). “thought I’d been kicked in the head”. Vomiting; collapse; seizures; followed by vfcoma. Neck stiffness; Kernig’s sign (6hrs to develop- positive when the leg is bent at the hip and knee at 90 degree angles, and subsequent extension in the knee is painful (leading to resistance)); retinal or subhyaloid haemorrhages; focal neurology: pupil changes- CNIII palsy with post comm art aneurysm. May have previously suffered a sentinel headache: small warning leak (6%), recall bias Primary care: 25% with sudden severe headache have SAH. Meningitis, migraine, intracerebral bleeds, cortical vein thrombosis. Rebleeding →commonest cause of death (20%) in first few days; cerebral ischaemia due to vasospasm; hydrocephalus; Management CT: detects 90% within first 48hrs. Neurosurgery stat: endovascular coiling Ca2+ channel blocker: nimodipine: prevents vasospasm Disorder– core How common is it Who does it affect Core symptoms Signs Biological causes/risk factors Management e.g. overall plans, referrals to other services Treatment - Social Tension headache Very common, especially in primary care Anyone and everyone Chronic daily headache, recurrent; tight band, pressure behind the eyes, throbbing and bursting sensations are common Tenderness and tension in the neck and scalp muscles Most are of innocent nature Due to neurovascular irritation and referred to scalp muscles and tissues; exact pathogenesis unclear May be obvious precipitating factors eg worry, noise, concentrated visual effort or fumes; depression is common too Often put down to cervical spondylosis, refractive errors or high BP: evidence remains poor though May be analgesic overuse too Explanation (imaging is often needed) Avoiding evident causes eg bright lights Analgesic withdrawal Physical treatments eg massage, ice packs, relaxation Antidepressants? Drugs for recurrent headaches/migraine Lots of lost days in work; unpleasant, disabling Disorder– core How common is it Who does it affect Core symptoms Biological causes/risk factors Management e.g. overall plans, referrals to other services Treatment Biological e.g. specific drugs Migraine >20% of any population world-wide report migranous symptoms; in 90%, these begin <40yo Common around puberty and at menopause Prevalence 8%; F:M 2:1 Recurrent headache with visual or GI disturbance; ?tension headaches; some cross-over Attacks range from intermittent headaches indistinguishable from tension headaches to discrete episodes that mimic thromboembolic cerebral ischaemia Types of migraine (though may be indistinguishable): usual main steps Well-being before an attack Prodromal symptoms Main attack – headache, nausea, vomiting Sleep and tiredness after 1. Migraine with aura (classic): o Prodrome: visual symptoms – due to depression of visual cortex/ retinal function eg unilateral patcy scotomata (retina); hemianopic symptoms (cortex); teichopsia (flashes); fortification spectra (jagged lines); transient aphasia sometimes, unilateral tingling and numbness and nausea; lasts few mins-hour or so o Headache: often hemicranial (splitting the head); begins localised and becomes general; ↑ nausea and vomiting; pt is irritable and prefers dark; superficial scalp arteries dilated and engorged; passes after few hours; then deep sleep follows 2. Migraine without aura (common): o Commonest; no prodrome; similar headache and nausea o Diagnosis: >5 headaches lasting 4-72hrs with either nausea/vomiting or photo/phonophobia AND >2 of unilateral, interferes with normal life, worsened by routine activity (climbing stairs) 3. Basilar migraine: o Prodrome includes circumoral and tongue tingling, vertigo, diplopia, transient visual disturbance, syncope, dysrthria, ataxia; may occur alone or progress to headache 4. Hemiparetic migraine: o Rare; classic migraine but also stroke-like symptoms with recovery in 24hrs 5. Ophthalmoplegic migraine and facioplegic migraine: o Rare; 3rd, 6th and 7th nerve palsies with migraine; need investigation Mechanisms unclear still; Genetic factors: familial form of migraine exists associated with α1-subunit of P/Q type vgc Ca2+ channel on chromosome 19. Change in brainstem blood flow: causes an unstable trigeminal nerve nucleus and nuclei in the thalamus ; causes release of calcitonin-related peptide (CGR8), substance P and other vasoactive substances => neurogenic inflammation, pain and vasodilation of cerebral and dural vessels Dysfunction in sensory modulation of craniovascular afferents Cortical spreading depression ?causes the aura Precipitating factors: CHOCOLATE Cheese (↑ in tyramine)/chocolate (↑ in phenylethylamine) Oral contraceptives/ pregnancy Caffeine (or its withdrawal) Alcohol Anxiety Travel Exercise Weekend (time of relaxing) Noise and irritating lights Association with premenstrual symptoms In 50% cases, no triggers found Explanations Avoidance of dietary triggers Brand change if related to oral contraceptive 1. Prophylaxis: if frequency >2/month; if one drug doesn’t work after 3 months, change drug; 65% of pts will report a ↓ frequency by 50% a. Pizotifen (5-HT antag) 0.5mg ON for several days ↑ to 1.5mg b. Propanolol (β-blocker) 10mg TDS, ↑ to 40-80mg TDS c. Amitryptilline: 10mg ON d. 2. 3. 4. 5. 6. Differential diagnosis 2nd line: sodium valproate 500mg BD; methysergide; SSRIs, verapamil; topiramate; nifedipine; naproxen also used Treatment: Paracetamol; 1g QDS Antiemetic: metoclopramide 5mg Po Sumitriptan (5HT-1B/D agonist): constrict cranial arteries Ergotamine: (5HT agonist): constrict cranial arteries 1mg PO as headache starts, repeated every 30mins but no more than 3mg/day, 6mg/week Sudden migraine: SAH or meningitis Hemiplegic, visual and hemisensory symptoms: thromboembolic TIAs (nb in TIA maximum deficit is present immediately = sudden; headaches = gradual) Unilateral tingling or numbness: sensory epilepsy (partial seizures) Cluster or tension headaches Cervical spondylosis Sinusitis/ottitis media Epilepsy Description Epidemiology Cause Recurrent tendency to spontaneous, intermittent abnormal electrical activity in part of the brain that manifests as seizures. Simple= awareness unimpaired, Complex= awareness impaired. Prevalence: 1% Age groups: 2/3 idopathic (FHx); Structural: cortical scarring (head inj), developmental, space occupying lesion, stroke, hippocampal sclerosis. Non-epileptic causes of seizures: trauma, stroke, haemorrhage, ↑ICP, alcohol/ benzodiazepine withdrawal, metabolic disturbance. Risk Factors Symptoms Presentation Seizure Classification- PARTIAL: focal onset to one hemi Simple partial: awareness unimpaired, focal motor sensory autonomic psychic Sx. No post-ictal Sx. Complex partial: awareness impaired. Aura, most commonly arise from temporal lobe. Postictal confusion. Partial seizure with secondary generalisation: spreads causing convulsions. PRIMARY GENERALISED SEIZURES: throughout cortex, not localising features to one hemi. Absence Seizures: (aka petit mal) brief (<10s) pauses- stop talking mid-sentence and carry on where left off. Presents in childhood→progresses tonic clonic in adult. Tonic-Clonic Seizures: (aka grand mal) loss of consciousness. Limbs stiffen (tonic) then jerk (clonic) post-ictal confusion and drowsiness. Myoclonic seizures: sudden jerk of a limb, face, trunk. Signs Differential diagnosis Complications Investigations Treatments Drugs Vasovagal syncope, hypoglycaemia, Stokes-Adams attacks, Management Are these real seizures?→ tongue biting and slow recovery suggestive. Partial or generalised? Triggers? Flickering lights, alcohol. Tonic-clonic: sodium valporate, lamotrigine, carbamazepine Absence: sodium valporate, lamotrigine, ethosuximide Tonic, myoclonic- as for generalised but avoid carbamazepine which may worsen Sx Partial seizures: Carbamazepine Parkinson’s Disease Description Epidemiology Cause Parkinsonism: triad- tremor, rigidity, bradykinesia. Causes of Parkinsonism: Idiopathic PD; multiple cerebral infarcts; Parkinson plus syndromes; post-encephalopathy; drug induced; toxin induced (MPTP) (Wilson’s disease); Trauma Prevalence: 1.6% Age groups: mean onset 65yrs Degeneration of dopaminergic neurons in the substantia nigra, pars compacta, associated with Lewy bodies. This causes ↓striatal dopamine levels. The degeneration is thought to be related to mitrochondrial dysfunction. Risk Factors Symptoms Signs Differential diagnosis Presentation Tremor: worse at rest, characteristic ‘pill rolling’ action of thumb over 2 fingers. Rigidity: ↑tone, superimposed tremor causes ‘cog wheeling’ Bradykinesia: slowness of movement initiation, with progressive reduction in speed and amplitude of repetitive actions. Expressionless face, ↓blink rate, monotonous hypophonic speech, micrographia. Gait: reduced arm swing, festinance, freezing at obstacles and doors. Postural instability Distinguish tremor from essential: essential is tremor on movement not at rest, the opposite is for parkinsonism. Parkinsonism tremor is also slower than a cerebellar tremor (only 4-6cycles per sec) Complications Management Investigations Treatments Drugs MDT When to start L-dopa?: end of dose deterioration (duration of benefit from each dose becomes progressively shorter), and dopamine induced dyskinesias develop over time (510yrs). Start >70yrs or when PD seriously interferes with life. Dopamine agonists and MAO-B inhibitors are useful in delaying starting L-dopa. Levodopa: used combined with dopa-decarboxylase inhibitor as Co-Beneldopa (Madopar) or Co-Careldopa (Sinemet) Dopamine agonists: ropinrole, pramipexole, rotigotine. have fewer motor SE than Ldopa but more neuropsychiatric. (avoid ergot derived) Anitcholinergics: ↓tremor but cause confusion in elderly MAO-B inhibitors: selgiline, rasagiline. Reduce end of dose deterioration. COMT inhibitors: entacapone, tolcapone- lessen the ‘time off’ with those with end of dose wearing off. Prevent peripheral metabolism of L-dopa Peripheral neuropathy Neuropathy: pathological process affecting a peripheral nerve or nerves. Mononeuropathy: a process affecting a single nerve (including cranial nerves). Mononeuritis multiplex: (multiple mononeuropathy and or multifocal neuropathy) affects several or multiple nerves. Polyneuropathy: diffuse, symmetrical disease, usually commencing peripherally. The course may be acute, chronic, static, progressive, relapsing or towards recovery. Polyneuropathies are motor, sensory, sensorimotor and autonomic. They are classified broadly into demyelinating and axonal types, depending upon which principal pathological process predominates. It is often impossible to separate these clinically. Many systemic diseases cause neuropathies. Widespread loss of tendon reflexes with distal muscle weakness and sensory loss (‘glove and stocking anaesthesia’). Radiculopathy: disease affecting nerve roots and plexopathy, the brachial or lumbosacral plexus. Myelopathy means disease of the cord Pathophysiology to nerve damage: Peripheral nerves = nerve nucleus with axon and myelin sheath; blood supply via vasa nervorum 1. Demyelination: Scwann cell damage = myelin sheath disruption = slowing of conduction (Guillain–Barré syndrome, postdiphtheritic neuropathy and many hereditary sensorimotor neuropathies) 1. Axonal damage: nerve fibre dies back from periphery; conduction velocity normal though as axonal continuity is maintained in surviving fibres (toxic neuropathies) 2. Wallerian degeneration: changes following nerve section = axon and distal myelin sheath degenerate over weeks 3. Compression: focal demyelination at the point of compression (CTS) 4. Infarction: microinfarction of vaso nervorum as in DM and arteritis (polyarteritis nodosa, Churg-Straus syndrome). Wallerian degeneration occurs distal to infarct. 5. Infiltration: by inflamm cells (leprosy and sarcoid and neoplastic granulomas) Nb. Axonal regeneration = 1mm/day Types of mononeuropathy: Type Median (carpal tunnel syndrome) C6-T1 Ulnar (cubital tunnel syndrome) C7-T1 Radial (trapped in spiral groove) C5-T1 Sciatic L4-S2 Tibial S1-3 Phrenic C3,4,5 Presentation Treatment At wrist: Tinel’s sign: tap flexor/ anterior Aching pain in hand/ arm esp at aspect of wrist = tingling and pain night; parasthesiae in radial 3.5 Phalen’s test Symptoms are fingers; relieved by dangling out reproduced on passive of bed or shaking; maximal wrist flexion. Sensory loss and weakness of Rx: wrist splinting at night, local abductor pollicis brevis +/steroid injection +/- decompression wasting of thenar eminence. surgery. If pregnant, often subsides Proximal: after birth; ↓ weight Clawing of the hand due to Remove pressure on nerve at weakness of medial wrist flexors, elbow interossei, medial two lumbricals, hypothenar eminence wasting, sensory loss over medial 1.5 fingers Wrist drop and weakness of Recovery within a few months brachioradialis and wrist flexors; usual ?sensory loss to dorsal aspect of thumb Affect hamstrings and all muscles below the knee = foot drop, weak ankle dorsiflexion/eversion; loss of sensation to lateral knee Common fibular: damaged if fibular fracture Inability to stand on tiptoes (plantar flexion), invert the foot, flex the toes Other info Commonest mononeuropathy; typically not ass with any underlying disease but seen in hypothyroidism, DM, pregnancy, obesity, RA, acromegaly, amyloid, renal dialysis pts, following trauma to wrist, female Compressed at elbow so elbow trauma = cause Motor branch alone can be damaged in repeated palm trauma (from screwdriver handle, crutch, cycle handlebars) Damage via compression against the humerus eg arm draped over a hard chair for hours (‘Saturday night palsy’) Damaged by pelvic tumours or fractures to pelvis or femur Keeps the diaphragm alive: consider if orthopnoea with raised hemidiaphragm. Causes: lung Ca, myeloma, thoracic surg, Types of polyneuropathy: Type Guillain-barre syndrome (GBS) CharcotMarie-Tooth Syndrome Presentation Treatment Other info Acute (days-weeks); weakness of Diagnosis confirmed by nerve Most common (3/100,000/year); distal limb muscles +/- numbness; conduction studies – prolonged also called post-infective or acute this progresses proximally and distal motor latency; IV Ig inflammatory neuropathy; may lead to paralysis; loss of demyelinating; ?autoallergic basis tendon reflexes; respiratory and facial muscles may become weak too; monophasic – does not recur; often post minor infection eg Campylobacter jejuni and CMV which induce AB response against nerves Peroneal muscular atrophy. Distal limb wasting and weakness that slowly progresses over years. Legs resemble ‘inverted Champaign bottles’. Mild cases: pes cavus and clawing of toes. Mostly motor: Guillain-barre syndrome, lead poisoning, Charcot-Marie-Tooth syndrome Often progressive; clumsiness of hands; difficult walking; resp difficulty; signs are of LMN lesion: wasting and weakness are ↑ in distal muscles of hand of foot (wrist or foot drop); ↓ reflexes Mostly sensory: DM, uraemia, leprosy Numbness; ‘feels funny’; tingling or burning sensations affecting extremities first (glove and stocking) Others: many others including due to DM, cancers, alcohol (Wernicke-Korsakoff syndrome), autonomic neuropathy, HIVassociated neuropathy Disorder– core How common is it Who does it affect Core symptoms Signs Meningitis = Medical emergency infection of the meninges Triad: headache, neck stiffness, fever, altered mental state = meningitis unless proven otherwise; if any two co-exist give benzylpenicilin 1.2g IM/IV before admitting. Bacterial: Early intense malaise, fevers, rigors, severe headache, photophobia, cold hands and feet, abnormal skin colour, vomiting developing within mins-hrs; pt is irritable and prefers to lie still; Later: meningism: neck stiffness and Kernig’s sign (pain + resistance on passive knee extension with hip fully flexed) appear in hrs; acute septicaemic petechial (1 or 2 spots, non-blanching) rash may develop very quickly: slow cap refill, DIC, ↓ BP, ↑ temperature, ↑ pulse Much later: conscious level ↓ coma; seizures (20%) +/- focal CNS signs; Viral: almost always benign, self-limiting condition lasting 4-10days; headache may follow for some months after; there is no serious sequelae unless encephalitis develops DD Biological causes/risk factors Severe headache of SAH or migraine Chronic meningitis resembles an intracranial mess lesion with headache, epilepsy, and focal signs Also ?malaria, encephalitis, septicaemia, SAH, dengue and tetanus 1. Infective a. either directly by extension from the ears, nasopharynx, head injury or congenital meningeal defect b. or by bloodstream spread from elsewhere in the body 2. Non-infective: malignant cells, intrathecal drugs, blood following SAH RF: Immunocompromised (HIV, cytotoxic drug therapy) Investigations e.g. to confirm diagnosis, exclude physical causes etc Bacterial infection: acute: pia-arachnoid is congested with PMN and a layer of pus forms which may organise to form adhesions, causing CN palsies and hydrocephalus chronic: (TB), brain is covered by a viscous green-grey exudates with numerous meningeal tubercles; adhesions are invariable; cerebral oedema occurs in any case Neisseria meningitidis (eg petechial rash) Streptococcus pneumoniae (eg via skull fracture, ear disease, congenital CNS lesion) Staph A Haemophillus influenza (Hib): rare in Uk as vaccine available Group B strep (neonates) G-ve bacilli eg E coli (neonates) Listeria monocytogenes Myconbacterium tuberculosis Treponema pallidum N meningitides and strep pneumonia = 70% acute bacterial cases outside neonate period Viral infection: mainly a lymphocytic inflamm CSF reaction w/o pus formation, PMNs or adhesions; there is little cerebral oedema unless encephalitis develops Enteroviruses (echovirsus, coxsackie, enterovirus 70) Herpes virus family: HSV 1 + 2, varicella zoster (chicken pox), CMV, EBV HIV, poliomyelitis (eg international travel), mumps Leptospirosis (eg via work in drains, canals, polluted water, swimming pools) Fungi: rare but Cryptococcus neoformans, candida albicans Bloods: FBC, U and E, LFTs, glucose, coagulation Blood culture: Throat swabs: one for bacterial and one for viral Stool sample: for viruses Lumbar puncture if safe (contraindicated if ↑ ICP, focal signs, papilloedema, traums, middle ear pathology, major coagulopathy); send samples for MC and S, gram stain, protein estimation, glucose, virology CT scan: if CNS mass lesion/ ↑ ICP suspected (↓ consciousness) instead before coning occurs! Typical CSF changes after doing a lumbar puncture: LP: CSF Appearance Predominant cell Glucose Protein Bacteria Normal Crystal clear No PMNs and <5mm3 lymphocytes 2/3-1/2 blood glucose 0.2-0.4g/L Pyogenic Turbid Polymorphs mainly with some lymphocytes <half plasma TB Fibrin web/viscous Lymphocytes but PMNs could also be high <half plasma Viral Clear Lymphocytes only (some PMNs seen if very early stages) >half plasma 0.5-2.0g/L In smear and culture 0.5-3.0g/L Often none in smear 0.4-0.8g/L None seen or cultured Look for signs of causative organism: zoster; coldsore/genital vesicles HSV; HIV signs (lymphadenopathy, dermatitis, candidiasis, uveitis); parotid swelling (mumps); sore throat +/jaundice (glandular fever) Management e.g. overall plans, referrals to other services Bacterial meningitis is fatal unless treated. Follow hospital policy! 1. If outside hospital: IV/ IM benzylpenicillin 1.2g while awaiting transfer to hospital 2. In hospital: ABCs, O2 high-flow, ?fluid resuscitation Do septicaemic or meningitic symptoms predominate?? Septicaemic: ↓ CRT, cold hands and feet (occurs before ↓ BP), rash: do not attempt lumbar puncture; cafotaxime 2g IV; get help; assess for signs of shock – if yes then fluid resus, inotropes/vasopressors, activated protein C2, Meningitic: neck stiffness, photophobia; dexamethosone 4-10mg/6hrs IV; if no shock or ↑ ICP signs then do lumbar puncture; 2g cefotaxime IV post LP Subsequently: get help and continually monitor on ITU Notify public health Rifampacin for ‘kissing contacts’ Renal Disorder– core How common is it Who does it affect Core symptoms Signs Biological causes/risk factors Acute Kidney Injury (AKI) A significant deterioration in renal function occurring over hours-days. Should produce 0.5ml x Kg/hour = normal urine produced Incidence of hospital-acquired AKI has ↑. Incidence of community-acquired AKI on admission to hospital is ~1% in the UK (AKI superimposed on CKD accounting for 50% of these patients) Incidence of severe AKI (creatinine>500 μmol/L) is ~ 130-140/million Less severe AKI (patients with creatinine levels of up to 177 μmol/L or a 50% rise from baseline) is ~200/million/year. May be no symptoms May be no signs but oliguria (urine vol<400ml/24hr) is common. Biochemically, detected by rising [urea] and [creatinine] May be isolated problem, but often due to circulatory disturbance (severe illness, sepsis, trauma, surgery, nephrotoxic drugs) 1. Pre-renal Along with acute tubular necrosis, account for 80% cases. Due to hypoperfusion: hypovolaemia, sepsis (causing systemic vasodilation), CCF, liver cirrhosis, renal artery stenosis, NSAID and ACE-I (interfere with blood flow) 2. Renal Acute tubular necrosis (ATN): damage to tubular cells caused by: a. Ischaemia: causes of hypoperfusion above b. Vascular: vasculitis, malignant hypertension, glomerulonephritis, hepatorenal syndrome, haemolytic uraemic syndrome, cholesterol emboli c. Nephrotoxins: d. Exogenous i. Analgesics (NSAIDS) ii. Antimicrobials (gentamicin, tetracycline, sulphonamides, vancomycin, acyclovir, amphotericin B) iii. Radiocontrast media iv. Anaesthetic agents (methoxyflurane, enflurane) v. Chemotherapeutic agents (cis-platin) vi. ACE-I and angiotensin 2 receptor antagonists vii. Immunosuprresants (cyclosporin, methotrexate) viii. Heavy metal poisoning (mercury, lead, arsenic, bismuth) ix. Organic solvents (ethylene glycol, carbon tetrachloride) x. Insecticides, herbicides, snake venom, Amantia mushrooms xi. B-cell myeloma e. Endogenous i. Pigments (haemaglobinuria in haemolysis) ii. Crystals (urate) iii. Proteins (Ig) f. Aminogylcasides (gentamicin, streptomycin) i. Mild non-oliguric state 1-2 wks into therapy; give single bolus aminoglycaside instead g. Radiocontrast nephropathy: iatrogenic i. RF = diabetes mellitus, high doses of media, hypovolaemia, pre-existing renal impairment, nephrotoxic drugs; therefore stop nephrotoxic drugs peri-procedure and pre-hydrate with IV 0.9% NaCl h. Rhabdomyolysis (skeletal muscle breakdown), causes release of myoglobin, K +, phosphate, urate and CK i. Trauma ii. Prolonged immobilisation after falling iii. Crush injury iv. Excessive exercise v. Uncontrolled seizures vi. Drugs (statins, fibrates, snake bites, CO) vii. Infections (EBV, influenza, coxsackie) viii. Inherited muscle disorders (DMD, McArdle’s) 3. Post-renal Investigations e.g. to confirm diagnosis, exclude physical causes etc Urinary obstruction Assessment: 1. Is the renal failure acute or chronic? a. Suspect chronic if: i. History of co-morbidity eg Diabetes mellitus, hypertension, sign of CRF ii. Previous abnormal blood tests (GP records) iii. Small kidneys on US (<9cm) with ↑ echogenicity 2. Is there a urinary tract obstruction? a. Reversible and prompt treatment prevents irreversible damage. Always consider in pts: i. with a single functioning kidney ii. with a Hx of renal stones, anuria, prostatism, previous pelvic/retroperitoneal surgery: examine for an enlarged prostate, palpable bladder, pelvic or abdo masses 3. Is there a rare cause of AKI? a. Glomerulonephritis (ass wihhaemturia or proteinuria) Tests: 1. Blood a. b. c. 2. Management e.g. overall plans, referrals to other services 3. 4. 5. 1. 2. 3. U+E (↑ K+), FBC, LFT, clotting, CK, ESR, CRP Consider ABG, blood cultures, hepatitis serology if dialysis considered Cause unclear: do serum Ig, electrophoresis, C3/4 levels, autoantibodies (ANA, ANCA, antidsDNA, anti-GBM, ASOT) Urine a. Dipstick: WBC, nitrite, blood, protein, glucose b. Microscopy: RBC, WBC, crystals, casts c. Culture and sensitivity d. Chemistry: creatine, osmolarity, Bence-Jones protein CXR: pulmonary oedema ECG: if signs of hyperkalaemia Renal US: size or obstruction? Enlist specialist help Initial Mx of ATN is to keep pt alive until spontaneous recovery of renal function occurs Do what you can in the meantime: Treat shock US scan (check for a palpable bladder first – its absence does not rule out obstruction) Stop nephrotoxic drugs Sign of vasculitis (nosebleeds, haematuria, rash, ↑ ESR/CRP?, checlautoAb Treat exacerbating factors: hypovolaemia, sepsis, high BP Monitor: Consider transfer to ICU Daily fluid balance and weight charts (match fluid to loss +500mL for insensible loss) Correct volume depletions with fluids (colloid, saline, blood) If septic, take cultures and treat empirically. Remove potential sources (catheter) if possible. Check for nephrotoxic drugs again. Aim for normal nutritional intake Indications for acute dialysis: 1. Refractory pulmonary oedema 2. Persistent hyperalaemia (K+>7mmol/L) 3. Severe metabolic acidosis (pH <7.2 or metabolic excess <10) 4. Uraemic encephalopathy 5. Uraemic pericarditis (pericardial rub) Treatment Biological e.g. specific drugs Nb 1. Signs of hypovaolaemia: low urine output, invisible JVP, poor tissue turgor, dry mucus membranes, low BP, high pulse 2. Signs of fluid overload: gallop rhythm on cardiac auscultation, high BP, high JVP, lung crepitations, peripheral oedeama Treat complications: 1. Hyperkalaemia: may cause arrhythmia and arrest a. ECG changes (in order): tall ‘tented’ T waves, small/absent p waves, ↑ P-R interval, widened QRS, ‘sine wave’ pattern, asystole IV Ca2+: 10mL of 10% calcium gluconate via a big vein over 2mins. Repeat until ECG improves. This is cardioprotective. c. IV insulin and glucose: 10U Actrapid insulin and 50mL 50% glucose over 30mins. Insulin stimulates K+ intracellular uptake (lowers serum K+ by 1-2mmol/60mins). Check capillary glucose after 30mins of giving insulin. d. Salbutamol 5mg nebuliser e. Haemodialysis is usually required if anuric Pulmonary oedema a. Sit pt up and give high flow O2 mask b. Venous vasodilator: 2.5mg IV morphine (plus metoclopramide) c. Furosemide: 120-250mg IV over 1 hour d. Urgent haemodialysis if no response; consider CPAP (continuous positive airways pressure ventilation) Bleeding a. Stop bleed b. Give fresh frozen platelets if there are clotting problems c. Blood transfusion to maintain Hb>10g/dL and haemotcrit>30% d. Desmopressin to increase factor 8 activity and normalise bleeding times. b. 2. 3. Chronic renal failure (CRF) = Chronic Kidney Disease (CKD): Long-standing, progress, impaired renal function; most cases you are unable to reverse the primary disease process (exceptions = correction of urinary tract obstruction, immunosuppressive therapy for systemic vasculitis and Goodpasture's syndrome, treatment of accelerated hypertension, and correction of critical narrowing of renal arteries causing renal impairment); rate of progression can be slowed Disorder– core How common is it Who does it affect Core symptoms Signs CKD = GFR <60 mL/min/1.73 m2 or a GFR >60 mL/min/1.73 m2 together with the presence of kidney damage, present for >3 months Stage GFR ml/min/1.73m2 Notes 1 >90 Normal or ↑GFR with other evidence of renal damage 2 60-89 Slight ↓GFR with other evidence of renal damage 3A 45-59 Moderate ↓GFR +/- evidence of renal damage 3B 30-44 4 15-29 Severe ↓GFR +/- evidence of renal damage 5 <15 Established renal failure. *renal damage: proteinuria, haematuria, evidence of disease Common causes: Sub-Saharan Africa = malaria = glomerulonephritis Middle east = urinary tract obstruction 4x more common in black Africans than whites in UK and USA CKD due to atherosclerotic renal disease more common in elderly >70% of all CKD cases are due to DM, atherosclerosis and hypertension Early CKD = often asymptomatic Serum urea and creatinine measured as easy to measure and rough correlation exists with symptoms (though they do not directly cause the symptoms) Possible cause of symptoms: breakdown products of protein (as protein restriction helps relieve symptoms) Symptoms common when [urea] > 40mmol/L: malaise, loss of energy loss of appetite/anorexia insomnia nocturia and polyuria due to impaired concentrating ability itching/pruritis nausea, vomiting and diarrhoea; metallic taste paraesthesiae due to polyneuropathy 'restless legs' syndrome (overwhelming need to frequently alter position of lower limbs) bone pain due to metabolic bone disease paraesthesiae and tetany due to hypocalcaemia symptoms due to salt and water retention - peripheral or pulmonary oedema (SOB, ankle swelling) symptoms due to anaemia amenorrhoea in women; erectile dysfunction in men. Oliguria [urea] > 60mmol/L = more severe uraemic symptoms and CNS involvement eg mental slowing, confusion, clouding of consciousness, seizures, myoclonic twitching, encephalopathy, coma Urine output is not a useful guide to kidney function as though GFR decreases => oliguria; tubular resorption is also less so high vols of urine may still result Few signs of uraemia; may include: Short stature (if CKD in childhood) Pallor due to anaemia or yellow pigmentation (uraemic syndrome) Bruising or purpura Increased photosensitive pigmentation Brown discolouration of the nails Scratch marks due to uraemic pruritis Signs of fluid overload eg pleural effusion Pericardial friction rub Mitral regurgitation due to overload or annular calcification Glove and stocking peripheral sensory loss (rare) High BP Impalpable kidneys unless enlarged due to PCKD, tumour or obstruction Screening questions to ask Biological causes/risk factors Investigations e.g. to confirm diagnosis, exclude physical causes etc Signs of an underlying condition that has lead to CKD: cutaneous vasculitic lesions in systemic vasculitides retinopathy in diabetes evidence of peripheral vascular disease evidence of spina bifida or other causes of neurogenic bladder. Should assess hydration status (JVP and skin turgor, BP lying and standing) duration of symptoms drug ingestion, including non-steroidal anti-inflammatory agents, analgesic and other medications, and unorthodox treatments such as herbal remedies previous medical and surgical history, e.g. previous chemotherapy, multisystem diseases such as SLE, malaria previous occasions on which urinalysis or measurement of urea and creatinine might have been performed, e.g. pre-employment or insurance medical examinations, new patient checks family history of renal disease. Congenital and inherited disease: PCKD (adult and infantile forms); Medullary cystic disease; Tuberous sclerosis; Oxalosis; Cystinosis; Congenital obstructive uropathy Glomerular disease: Primary glomerulonephritides including focal glomerulosclerosis Secondary glomerular disease (systemic lupus, polyangiitis, Wegener’s granulomatosis, amyloidosis, diabetic glomerulosclerosis, accelerated hypertension, haemolytic uraemic syndrome, thrombotic thrombocytopenic purpura, systemic sclerosis, sickle cell disease) Vascular disease: Hypertensive nephrosclerosis = ↑BP; Reno-vascular disease; Small and medium-sized vessel vasculitis; DM Tubulointerstitial disease: Tubulointerstitial nephritis – idiopathic, due to drugs (especially nephrotoxic analgesics), immunologically mediated; Reflux nephropathy; Tuberculosis; Schistosomiasis; Nephrocalcinosis; Multiple myeloma (myeloma kidney); Balkan nephropathy; Renal papillary necrosis (diabetes, sickle cell disease and trait, analgesic nephropathy); Chinese herb nephropathy Urinary tract obstruction: Calculus disease; Prostatic disease; Pelvic tumours; Retroperitoneal fibrosis; Schistosomiasis RF: DM, age >60, recurrent UTIs, urinary obstruction, systemic illness that effects the kidneys Bloods: o FBC: Hb ↓ (normocytic, normochromic), eosinophilia (vasculitis, allergic tubulointerstitial nephritis); fragmented RBC +/- thrombocytopenia (accelerated HTN, haemolytic uraemic syndrome) o ESR ↑ (myeloma, vasculitis) o U and E: ↑ urea and creatinine, eGFR, glucose, ↓ Ca2+, ↑ PO43-, ↑ ALP (renal osetoadenopathy), ↑ PTH (hyperparathyroidism) o Immunology: autoantibody screening (SLE), antibodies to HBV, HCV, HIV Urinalysis: o haematuria: ?glomerulonephritis though other causes need to be excluded o proteinuria: glomerular disease though infection may also cause it o glycosuria with normal blood glucose is common in CKD Urine microscopy, culture and sensitivity (MCS): o WCC = active bacterial infection though this is uncommonly a cause of CKD o Eosinophiluria allergic tubulointerstitial nephritis or cholesterol embolization. o Casts. Granular casts formed from abnormal cells within the tubular lumen, and indicate active Complications (summary) Management e.g. overall plans, referrals to other services Treatment Biological e.g. specific drugs renal disease. Red-cell casts are highly suggestive of glomerulonephritis. o Red cells in the urine may be from anywhere between the glomerulus and the urethral meatus Urine biochem: o 24hr creatinine clearance for severity of renal disease o Urine osmolality is a measure of concentrating ability; low osmolality is normal if ↑ fluid intake but otherwise indicates renal damage Radiology: o US: exclude obstruction (and hydronephrosis) and look at renal size (usually small <9cm) but may be large if CKD in DM, PCKD, amyloidosis, myeloma o AXR: exclude renal stones which may be missed on US o CT: useful to diagnose retroperitoneal fibrosis and may demonstrate cortical scarring o MRI and IV urography: seldom necessary Renal biopsy: if cause unclear and normal size kidneys Bone scan and CXR: osteodystrophy; signs of pleural effusion, cardiomegaly 1. Anaemia: due to EPO deficiency and less so to retention of bone marrow toxins, bone marrow fibrosis, ↑ RBC destruction, blood loss (GI bleed, blood sampling, haemodialysis, platelet dysfunction), ACE-I (interfere with normal EPO control) 2. Bone disease: renal osteodystrophy: due to ↓ production of 1α-hydroxylase => ↓ activation of vit D; includes osteomalacia, osteoporosis, osteosclerosis, hyperparathyroid bone disease 3. Skin disease: pruritis due to retention of nitrogenous waste products 4. Nephrogenic systemic fibrosis (NSF): 5. GI problems: decreased gastric emptying and ↑ risk of reflux, PUD, pancreatitis, constipation 6. Metabolic: gout due to retention of urate; insulin requirements in DM pts ↓ (as kidneys to some extent break it down and excrete it) 7. Endocrine: hyperprolactinaemia, ↑ LH, ↓ testosterone (erectile dysfunction and ↓ spermatogenesis), absence of normal cyclical hormones in females so ilogomenorrhoea, impaired growth in uraemic children; abnormal thyroid problems 8. Muscles: due to uraemia but unsure how; also ↓ physical fitness = cardiovascular conditioning 9. Nervous system: seizures, dialysis dementia, overactivity of SNS, carpal tunnel syndrome, restless legs syndrome due to uraemia 10. CV: ↑ risk of MI, HF, sudden death, stroke 11. Malignancy: ↑ in pts with CKD and dialysis Contact nephrologist! Relieve obstruction, stop nephrotoxic drugs, deal with ↑ Ca 2+, HTN: even a small ↓ in HTN may save kidney function Oedema: furosemide and limit fluid intake Anaemia: exclude iron deficiency and chronic infection; consider EPO injections Osteodystrophy: treat if ↑ PTH (PO4 ↑ which causes ↑ PTH further) so give Calcichew (binders); vit D analogues (alfacalcidol) or calcitrol and Ca supplements ↓ bone disease and hyperparathyroidism Diet: Na restriction to control BP; moderate protein diet; K+ restriction if hyperkalaemia; HCO3- if acidotic Restless legs: clonazepam or gabapentin Prepare for dialysis (renal replacement therapy) or transplant: o Haemodialysis: blood flows on 1 side of a semi-permeable membrane whilst dialysis fluid flows in the opposite direction on the other; solute transfer by diffusion o Haemofiltration: used for critically ill pts as better; blood is filtered continuously across a highly selective permeable synthetic membrane so waste removal by convection; ultrafiltrate is then substituted with an equal volume of replacement fluid o Peritoneal dialysis: useful for elderly, children, at home, pts with CV disease; PD fluid introduced into peritoneal cavity and uraemic solutes diffuse into it across the peritoneal membrane Monitoring: some lose function at a constant rate → reciprocal plot of plasma creatinine (plasma Cr on y axis, years on x axis, 295 OHCM) gives a straight line parallel to the decline in GFR →predict need for dialysis. Drugs: ↓dose of following drugs that are renally excreted: aminoglycosides (gent); heparin, Lithium; Digoxin; Ethambutol; Cephalosporins; Sulfmethoxazole; Procainamide; Tetracycline, opiates. Urinary tract infection (UTI) The presence of pure growth of >105 organisms/mL of fresh MSU. Bacteria = bacteria in the urine but patient may be symptomatic or asymptomatic. Can affect bladder (cystitis), urethra (urethritis), prostate (prostatitis) or renal pelvis (pyelonephritis). Disorder– core They may be uncomplicated (normal renal tract and function) or complicated (abnormal renal/GU tract, decreasing function, impaired host defences, virulent organisms eg Staph A, diabetes mellitus, ). Assume UTI in men w/o RF is complicated. How common is it Who does it affect Core symptoms Biological causes/risk factors 50,000/1mn/year; 1-2% presentations to GP; recurrent infections can cause considerable morbidity and renal failure. Up to a 1/3 of women with symptoms have bacteruria (= abacterial cystitis or urethral syndrome) Newborn males: due to higher GU abnormalities Teenage women: due to beginning of sexual activity Men when older: mostly due to prostate problems Women post-menopause: low oestrogen makes it easier for bacteria to adhere Women more so than men due to a short and straight urethra. If men or children have a UTI, then investigate further for abnormalities => complicated cystitis Symptomatic infection related to bacteria virulence but inflammation and injury determined by host response not bacteria. Cystitis = lower UTI: Frequency, urgency, nocturia, dysuria (painful void), haematuria, suprapubic pain Acute pyelonephrtis: fevers, rigors, vomiting, loin pain, tenderness, oliguria if renal failure Prostatitis: flu-like symptoms, backache, swollen/tender prostate on PR, few urinary symptoms Old patients: UTIs may cause confusion too (and low Na+; unknown reason!) Reflux nephropathy: (ie chronic pyelonephritis) results from a combination of vesicouretric reflux and an infection acquired in infancy/childhood Bacteria from person’s own bowel flora (gut); transfer via ascending transurethral route but may be via blood stream, lymphatics or direct extension (egvesicocolic fistula). See bacteria list after table. Dipstick +ve for leucocytes and nitrites is 95% indicative of infection on microscopy. Virulence determined by ability to adhere to epithelial cells. flagellae (for motility) aerobactin (for iron acquisition in the iron-poor environment of the urinary tract) haemolysin (for pore forming) presence of adhesins on the bacterial fimbriae and on the cell surface. E. coli with type 1 fimbriae associated with cystitis; E. coli with type P fimbriae are associated with pyelonephritis Risk Factors: Female, sexual intercourse, exposure to spermicide in females (by diaphragms or condoms), pregnancy, menopause, immunosuppression, urinary tract obstruction/ stones/ malformation (=urinary stasis ↑ bacteria), long-term catheter (post >30days = ~100% catheters are infected) Relapse is diagnosed by recurrence of bacteriuria with the same organism within 7 days of completion of antibacterial treatment and implies failure to eradicate infection usually in conditions such as stones, scarred kidneys, polycystic disease or bacterial prostatitis. Investigations e.g. to confirm diagnosis, exclude physical causes etc Reinfection is when bacteriuria is absent after treatment for at least 14 days, usually longer, followed by recurrence of infection with the same or different organisms. This is not due to failure to eradicate infection, but is the result of reinvasion of a susceptible tract with new organisms. Approximately 80% of recurrent infections are due to reinfection. 1. Urine sample: White bottle Red bottle: contains bolic acid which stops contaminate overgrowth that could affect results 2. Dipstick MSU (1st bit of urine discarded as bacteria from glans penis/labia minora may contaminate the test (note that CSU = catheter specimen) If infection present: ↑ leucocytes: due to inflammatory reaction (causing release of esterase from leucocytes); but DD = pyuria, stones, cancer, catheter urine ↑ nitrites: bacteria have an enzyme that metabalises nitrates to nitrites If symptomatic, dipstick urine and treat empirically if nitrites or leucocytes positive. Note that dipstick haematuria (microscopic) = 4% cancer risk; frank haematuria = 30% cancer risk Note that if dipstick haematuria present and proteins too, indicates podocyte malfunction (leaky glomeruli) and ?glomerulonephritis 3. MC+S Microscopy: WBC: >3/field = pyuria RBC: >2? = microscopic haematuria General comments: hyaline casts? Red cell casts? => almost 100% glomerulonephritis Culture and sensitivity: Grow bacteria on Agar plates. Takes 1-2 days Treatment Biological e.g. specific drugs Special investigations: evaluate males/ children/ recurrent infection/ very severe symptoms/ DM Ultrasound: assess suspected pyelonephritis that requires drainage; detects calculi, obstruction and incomplete emptying CT: follow-up of complicated renal tract infection. MRI: useful in pts with iodinated contrast allergies Single isolated attack:pretreatment urine culture is desirable. Antibiotics for 3–5 days with amoxicillin, nitrofurantoin, trimethoprim (40% resistance rate) or an oral cephalosporin. Modify in light of MC and S, or clinical response If resistance:coamoxiclavor ciprofloxacin If no previous Hx of UTI and within 36hrs of bladder symptoms: amoxicillin or co-trimoxazole Drink plenty of fluids (2L) during and after treatment for a few weeks; repeat urine culture after 5 days If suspect acute pyelonephritis: give antibiotics by IV (aztreonam, cefuroxime, ciprofloxacin or gentamicin), then switch to oral Ab for a further 7days. IV fluids may be required to achieve a good urine output Recurrent infection: Relapse: search for a cause (stoned or scarred kidneys) and eradicate Reinfection: suggests predisposition to periurethral colonisation or poor bladder defence mechanisms; all pts must take prophylactic measurements: a 2 L daily fluid intake; voiding every 2- to 3hrs; voiding before bedtime and after intercourse; avoidance of spermicidal jellies and bubble baths and; avoidance of constipation, which may impair bladder emptying Urinary Tract Obstruction...hydronephrosis Description Epidemiology Cause Common and should be considered in any pt with impaired renal function. Damage can be permanent. Prevalence: common Age groups: Can occur anywhere from renal calyces to urethral meatus. Obstruction lesions are, luminal: stones, clots, sloughed papilla, tumour (renal, ureteric, bladder); mural: congenital or acquired stricture, schistosomiasis; extra-mural: abdo/pelvic mass/tumour. Risk Factors Symptoms Signs Differential diagnosis Complications Investigations Treatments Drugs Presentation Unilateral obstruction may be clinically silent if other kidney is functioning. Acute upper tract obstruction: loin pain radiating to the groin. May be superimposed infection +/- tenderness or enlarged kidney Chronic upper tract obstruction: flank pain, renal failure, superimposed infection. Polyuria may occur owing to impaired urinary conc. Acute lower tract obstruction: acute urinary retention, severe suprapubic pain, preceeded by sx of bladder outflow obstruction, distended, palpable bladder, dull to percussion. Chronic lower tract obstruction: urinary frequency, hesitancy, poor stream, terminal dribbling, overflow incontinence. Distended palpable bladder +/- large prostate on PR. Complications: UTI, retention. Hydronephrosis dilation distension of the renal pelvis calyces. Management US: hydronephrosis or hydroureter → antegrade or retrograde ureterogram- drainage Upper: nephrostomy or ureteric stent. Pyeloplasty to widen PUJ Lower: urethral or suprapubic catheter. Rx underlying cause. Disorder– core How common is it Who does it affect Core symptoms Signs Biological causes/risk factors Benign prostatic hypertrophy (BPH) 80% of 80yo Men over 60yo, less common in Asians Enlargement of the gland stretches and distorts the urethra as it passes through, obstructing bladder outflow. Frequency of urination, nocturia is earliest symptom usually, difficulty starting, poor flow, terminal dribbling, double voiding, acute retention of urine or retention with overflow incontinence may occur. Occassionaly rupture of prostatic veins, bacteriuria or stones cause haematuria Abdo exam for bladder enlargements; rectal exam. Prostate feels smooth. ↓ urine flow (<15mL/s) Aetiology unknown Investigations MSU; U and E; US (↑ residual volume, hydronephrosis) Rule out cancer: PSA; transrectal US +/- biopsy; nb do venepuncture for PSA before PR as PR can ↑ PSA Management Watchful waiting if mild-moderate symptoms as symptoms following therapy are often greater than those with no therapy at all. If acute retention, then relieve pain and insert catheter. Then consider prostatectomy (transurethral resection of the prostate TURP) or permanent indwelling catheter. Transurethal resection of the prostate (TURP): <14% become impotent after; 20% need redoing in 10y Transurethal incision of the prostate (TUIP): less destruction than TURP and ↓ risk to sexual function but gives similar benefit; achieves this by relieving pressure on the urethra Retropubic prostatectomy: open operation Transurethral laser-induced prostatectomy (TULIP): ?as good as a TURP Drugs: 1. Tamsulosin: α-blockers; ↓ smooth muscle tone of prostate and bladder but cause drowsiness, dizziness, depression, ↓ BP, dry mouth, ejaculatory failure, extra-pyramidal signs, nasal congestion, ↑ weight BUT drug of choice 2. Finasteride: competitive 5α-reductase inhibitor, which converts testosterone to dihydrotestosterone, thought to be the cause of BPH; it is excreted in semen so need to wear condoms and females shoul avoid handling crushed pills; may cause impotence and ↓ libido; effects are slow and limited so many try tamsulosin and skip to surgery Wait and see: risks incontinence, retention and renal failure Treatment Biological e.g. specific drugs Disorder– core How common is it Who does it affect Core symptoms Signs Investigations e.g. to confirm diagnosis, exclude physical causes etc Treatment Biological e.g. specific drugs Prognosis Prostatic carcinoma 7% of all cancers affecting men; 2nd most common cancer in men; 6th commonest in the world 80% of 80yo have malignant changes but most lie dormant; histologically = adenocarcinoma As for BPH, but may also have metastatic spread = back pain, weight loss, anaemia Hard, irregular gland on rectal exam PSA screening programmes in USA, not in the UK. PSA >4ng/mL is abnormal but could be due to BPH or prostate Ca; Problems with SA screening: test is not v accurate and no evidence that those with the test live longer; if false +ve result then may unduly have extra tests; only 30% of those with ↑ PSA have cancer Transrecal US of prostate and prostatic biopsy to confirm diagnosis histologically; bone scan Spread may be local )seminal glands etc) or haematogenously to bone (sclerotic bony lesions) RCT between radical prostatectomy and active surveillance (watchful waiting) = radical prostatectomy ↓ disease-specific mortality but no signif difference in terms of overall survival. But carries high morbidity of urinary incontinence and sexual dysfunction Local cancer: radiotherapy +/- androgen ablation therapy; goserelin if lymph node +ve Metastatic disease: orchidectomy (though most men refuse), LHRH analogues (goserelin, buserelin) may benefit for 1-2years 10% die within 6months, but 10% live >10years; most people die with the cancer not from it Staged using TNM system; graded using Gleason grade system (1-5). 5 carries worse prognosis. Two specimens are examined and score added up so total is 2-10. 8-10 = aggressive; 5-7 = intermediate; 2-4 = indolent Disorder– core How common is it Who does it affect Core symptoms Signs Biological causes/risk factors Investigations Management e.g. overall plans, referrals to other services Prognosis Renal cell carcinoma (RCC) 1-2% of all tumours; most common renal tumour in adults Male: female 2:1; rarely present <40yo; average age of presentation is 55yo Often asymptomatic; though possible haematuria, loin pain and mass in the flank Malaise, anorexia and weight loss (30%) Common: polycythaemia (5%); HTN (30%) due to secretion of renin by the tumour; anaemia due to depression of EPO production; may be pyrexical too Rare: left-sided varicocele due to invasion of renal vein and obstruction of left testicular vein into renal vein Arise from proximal tubular epithelium Von Hippel-Lindau disease: AD disorder, bilateral RCC, haemangioblastomas, phaeochromocytomas, renal cysts common US: demonstrates a solid lesion, examines patency of renal vein and IVC (?invasion) MRI: for staging Urine cytology for malignant cells and renal arteriography = no value nowadays Nephrectomy unless bilateral RCC or contralateral kidney functions poorly (partial nephrectomy may be done instead as conservative Mx); nephrectomy may still be done even if mets are present as these may reduce after a nephrectomy Medroxyprogesterone acetate: helps control metastatic disease IL-2 therapy: remission in ~20% cases Temsirolimus: new therapy, inhibits rapamycin kinase, improves overall survival in those with metastatic RCC Depends on stage and grade as usual; 60-70% 5-year survival rate if confined to renal parenchyma; 1535% if local lymph node involvement but only 5% if distant mets Nephroblastoma = Wilm’s tumour Found in <3yo; bilateral common; presents as abdominal mass; rarely haematuria; 90% 5-year survival Disorder– core How common is it Urothelial tumours eg bladder tumours/ transitional cell carcinomas (TCC) 3% of deaths from all cancers; bladder tumours are 50x more common than those of ureter or renal pelvis Male: female 4:1; uncommon <40yo Painless haematuria; although pain may occur if clot retention; Symptoms similar to UTI develop in the absence of bacteriuria Presenting symptoms may be due to local metastases TCC of kidney and ureter may also present with haematuria Smoking Exposure to industrial carcinogens (β-naphthylamine and benzidine – chemical, cable and rubber factories) Exposure to some drugs(phenacetin, cyclophosphamide) Chronic inflammation (schistosomiasis) Urine cytology: malignant cells present Renal imagaing: US, CT, MRI Cystoscopy: necessary unless pathology found in upper urinary tract (may be omitted if <20yo in men and 30yo in women if bacteriuria as well as haematuria, and both clear up on treatment and normal renal imaging too) Depends on stage and grade (has it invaded the bladder muscle?) Superficial bladder tumours: transurethral resection with follow up cystoscopies; or bladder instillation (injection): doxorubicin, mitomycin, thiotepa, BCG (bacilli Calmette-Guerin, same as BCG jab!) Invasive tumours: radical cystectomy if <70yo or radical radiotherapy if >70yo (a new bladder is then made out of small bowel) 90% 5-year survival if superficial 5% 5-year survival if presenting with mets Who does it affect Core symptoms Biological causes/risk factors Investigations e.g. to confirm diagnosis, exclude physical causes etc Management e.g. overall plans, referrals to other services Prognosis Cancers that spread to bone: lung, breast, prostate, kidney, thyroid Bladder Bladder cancer tends to stay in the same area (the pelvis) and grow into nearby tissues such as the pelvic wall. It can also spread to the lungs, liver, and bone. Brain Brain cancer rarely spreads outside the brain. It mainly grows throughout the brain and sometimes into the spinal cord. Breast Breast cancer most commonly spreads to the bone, but also can spread to the liver, lung, and brain. As the cancer progresses, it may affect any organ, even the eye. It can also spread to the skin of the chest (near where the cancer started). Colon and rectum The most common site for colon cancer to spread is to the liver. It may also spread to the bone and lungs. Spread to the brain is uncommon. Rectal cancer commonly spreads to the lung, brain, and bone. But its major site of spread is in the pelvis, where the rectal cancer started. This can be painful because it often grows into nerves and bones in this area. Esophagus Esophageal cancer mostly grows near where it started. As it progresses, it may make it hard to swallow. This can happen very fast or slowly over many months. Kidney Kidney (renal) cancer can grow where it started and invade nearby tissues. When it spreads, the lungs and bones are the most common sites. Leukemia Because they are already in the blood, leukemias can be considered to have spread to all parts of the body when they are diagnosed. They can progress by filling the bone marrow with leukemia cells. The normal bone marrow is replaced and cannot make new blood cells, such as oxygen-carrying red cells, infection-fighting white cells, or platelets that stop bleeding. Tumors made up of leukemia cells can occur in the skin or in other parts of the body. Liver Liver cancer doesn't often spread outside the liver; rather, it grows throughout the liver as it becomes advanced. Lung Lung cancer can spread to any organ of the body, but most often it will spread to the adrenal glands, liver, bones, and brain. It will grow in the lung and spread to other parts of the lung, too. It can also grow into the sac around the heart (the pericardium). Lymphoma Most lymphomas tend to stay in the lymph nodes, spleen, and bone marrow. Some start in other organs, such as the brain or stomach. Others only spread to other organs when they are very advanced. Some lymphomas spread to the fluid around the brain and spinal cord (the cerebrospinal fluid or CSF). This is called lymphomatous meningitis. Melanoma Melanoma can spread anywhere in the body. It first tends to go to lymph nodes near where it started, but then can spread through the blood to the brain, lungs, liver, and bone. Mouth and throat Cancers of the mouth, throat, or nasal passages tend to stay in the same area. When they spread, it is usually to the lungs. Multiple myeloma Multiple myeloma can cause tumors called plasmacytomas. These tumors can spread to the bones anywhere in the body, but they rarely spread to other organs. Ovary Ovarian cancer most often spreads to the lining and organs of the belly (abdomen) and can cause a build-up of fluid and swelling in the abdomen. It can also spread to the outer lining of the lungs and cause fluid to build up there. As it becomes more advanced, it may spread to the lung and liver, or, rarely, to the brain or skin. Pancreas Pancreatic cancer mainly stays in the belly (abdomen). It grows into nearby tissues and may spread to the liver. It can also spread to the lungs, bones, and brain. Prostate Advanced prostate cancer most often goes to the bones. Much less often, it will spread to other organs, including the brain. Stomach Stomach (gastric) cancer tends to spread to nearby tissues and stay within the belly (abdomen). The next areas it goes to are the liver and lungs. Spread to bone and brain is less common. Disorder– core How common is it Who does it affect Biological causes/risk factors Investigations e.g. to confirm diagnosis, exclude physical causes etc Management e.g. overall plans, referrals to other services Incontinence: a condition defined by inappropriate and involuntary loss of urine that is objectively demonstrable that has effects on health or social interaction. Common referral to gynaecology clinics; >2x each month 8.5% in women aged 15-64 and 11.6% in women aged >65yo; underestimates possibly? 25% women and 15% men >65yo (K and C) 3million women in UK Elderly mainly but all age ranges possible Stress: UI due to ↑ abdo effects on bladder and weak pelvic floor or sphincter eg exercise, sneezing, coughing, jumping, damage to bladder neck or pelvic floor muscles during childbirth Urge: UI preceeded by urge eg bladder spasms, hyperactive detrussor muscle, UTIs; motor problem (MS) or sensory problem (irritation). Bladder is perceived to be full so empties. Mixed: urgency and link to sneezing or coughing… Overflow: dry during day but wet at night; leakage of urine from a full distended bladder; common in men with prostatic obstruction, following spinal injury or women with cytoceles or after gynae surgery Functional: inability to get to the toilet because of a disability eg stroke, trauma, dementia Overactive bladder syndrome (OAB) is defined as urgency that occurs with or without urge UI and usually with frequency and nocturia. OAB that occurs with urge UI is known as 'OAB wet'. OAB that occurs without urge UI is known as 'OAB dry'. 1. Physical examination for local problems: a. Prostate in men b. Gynaecological disorders in women c. Central problems: neurological disorders or dementia 2. Urinalysis: glycosuria (DM) or luecocytes/nitrites for UTIs 3. If not responding to management, try urodynamics a. Invasive tests, necessitating insertion of bladder and rectal catheters to measure total bladder pressure and abdominal pressure and to allow bladder filling b. Filling studies determine detrusor activity and compliance i. Low detrusor pressures with low urine flow suggest detrusor function problems ii. High detrusor pressures with a low flow suggest bladder outlet obstruction Treat contributing causes eg constipation, drug therapy, other co-existing disease Urge: bladder training, antimuscarinics, (oxybutynin, tolterodine, solifenacin) Stress: pelvic floor exercises, transurethral injection of autologous myoblasts to build the muscle sphincters, injection of collagen or botox around sphincter to close it off Overflow: remove the obstruction Functional: improve facilities, regular urine voiding, absorbent padding, ensure commodes available, catheterisation should be avoided Respiratory Disorder– core How common is it Who does it affect Core symptoms Signs Features/ symptoms of presentation in a primary care setting Biological causes/risk factors Chronic obstructive pulmonary disease (COPD) Airflow limitation/obstruction (defined as FEV1/FVC ratio <0.7) that is not fully reversible; usually progressive (over months) and associated with an abnormal inflammatory response of the lungs to noxious or noxious particles or gases. The impairment of lung function is not fully reversed by bronchodilator or other therapy. Nb. It is no longer necessary to have a FEV1 <80% predicted for definition of airflow obstruction; if >80% diagnosis of COPD should only be made in presence of resp symptoms (SOB and cough) Predicted to become 3rd most common cause of death and 5th most common disability worldwide by 2020 Combines a number of clinical syndromes ass with a destruction of the lung and airflow obstruction (symptoms: chronic bronchitis, chronic asthma; pathological: emphysema; physiological states: pink puffers and blue bloaters). As these conditions overlap, led to term COPD. 1999: 900,000 people with COPD in England and Wales; 30,000 death/year = 20x ↑ than asthma Smokers (90% cases); ↑ age-related decline in lung function by long-term exposure to toxic particles and gases. Only 10-20% smokers develop COPD, indicating susceptibility varies. Development of COPD proportional to number of cigarettes smoked/day (smoking 30/day = 20x more likely to develop COPD than a non-smoker). Early cessation allows rate of decline to return to normal. Pts pass through mild-moderate-severe stages in turn; they do not jump to severe. Consider in pts >35yo with chronic symptoms of SOB, wheeze, ‘smoker’s’ cough, white/ clear sputum normally but purulent when infective exacerbation, recurrent chest infections (colds ‘settle on the chest’). Symptoms made worse by cold, foggy weather, atmospheric pollution. Severe diseases = SOB with mild exercise or getting dressed. Systemic effects = hypertension, osteoporosis, depression, metabolic problems causing weight loss and loss of muscle mass. Diagnosis is made by spirometry. Note that peak flow meters are excellent in asthma but not COPD as underestimate level of lung damage If mild, possibly no signs or a quiet wheeze. Severe disease = tachypnoeic, prolonged expiration, used of accessory muscles, intercostals drawing on inspiration and pursing of lips on expiration. Chest expansion poor, lungs are hyperiniflated, loss of normal cardiac and liver dullness. If responsive to CO2 = breathless but rarely cyanosed, HF and oedema rare terminal events If not responsive to CO2 = cyanosed but not breathless, oedematous. Late disease = ?respiratory failure (which is defined as PaO2 <8KPa or a PaCO2 >7KPa. May also develop cor pulmonale (heart disease 2° to lung disease) Most pts do not present until moderate to severe stages of disease 3 mechanisms have been suggested for this limitation of airflow in small airways (<2 mm in diameter). 1. Loss of elasticity and alveolar attachments of airways due to emphysema. This reduces the elastic recoil and the airways collapse during expiration. 2. Inflammation and scarring cause the small airways to narrow. 3. Mucus secretion which blocks the airways. Each mechanism narrows the small airways and causes air trapping leading to hyperinflation of the lungs and breathlessness. Pathological basis: Increased number of mucus-secreting goblet cells in bronchial mucosa; bronchi may become inflamed and covered in pus. Microscopically: infiltration with acute and chronic inflammatory cells. Epithelial layer may become ulcerated, with squamous cells replacing the columnar cells on healing of the ulcer Inflammation leads to scarring and thickening of the walls => narrowing of the small airways Small airways especially affected in early disease (w/o any breathlessness); accounts for improvement in lung function if smoking is stopped early enough. Inflammation continues in later stages so smoking cessation not as effective. If airflow limitation is combined with emphysema (causing loss of the elastic recoil of the lung with collapse of small airways during expiration) the resulting airflow limitation is even more severe. n.b. emphysema is defined pathologically as dilatation and destruction of the lung tissue distal to the terminal bronchiole. It is classified according to the site of damage: o centri-acinar: commonest; distension and damage is around resp bronchioles whilst distal alveolar ducts are preserved o pan-acinar: less common; destruction involves whole acinus o irregular: patchy scarring and damage; no regard for acinar damage o emphysema leads to expiratory airflow limitation and air trapping. The loss of lung elastic recoil = ↑ TLC and premature closure of airways limits expiratory flow, and loss of alveoli = decreased surface area for gas exchange Pathogenesis: Cigarette smoking: ↑ number of neutrophil granulocytes that release elastases and proteases, causing damage. Also inhibits α1-antitrypsin which is a major anti-protease, further upsetting the balance. Infections: often the precipitating cause of an acute exacerbation of COPD α1-antitrypsin deficiency: produced in the liver, secreted into blood and diffuses into the lung; MZ heterozygous deficiency), ZZ (homozygous deficiency); hereditary deficiency accounts for 2% emphysema cases Spirometry: measures volume of air that the pt is able to expel after full inspiration; can differentiate between obstructive (COPD, asthma) and restrictive (size of lungs reduced eg fibrosis). Severity cannot be predicted based on signs and symptoms alone. Five measures: 1. FEV1: the volume of air that the patient is able to exhale in the first second of forced expiration 2. FVC: the total volume of air that the patient can forcibly exhale in one breath 3. FEV1/FVC: the ratio of FEV1 to FVC expressed as a percentage 4. VC: slow vital capacity 5. FEV1/VC: the ratio of FEV1 to the slow vital capacity FEV1/FVC FEV1 % predict NICE 2004 ATS/ERS 2004 GOLD 2008 NICE 2010 Investigations e.g. to confirm diagnosis, exclude physical causes etc 80 Mild Stage 1 (mild) * 50-79 Mild Moderate Stage 2 (moderate) <0.7 or 70% 30-49 Moderate Severe Stage 3 (severe) <30 Severe Very severe Stage 4 (very severe) ** All post-bronchodilator now; * symptoms should be present to diagnose mild COPD **or FEV 1 <50% with resp failure; values of FEV1 and FVC are expressed as a percentage of the predicted normal for a person of the same sex, age and height Condition Normal Obstruction Restriction Combined Asthma may show the same abnormalities on spirometry as COPD – if there is diagnostic doubt spirometry following reversibility testing may be used to identify asthma Technique: Patient must be sat down (to avoid fainting). Record their sex, age and height (predicts FEV 1). Demonstrate how to use it, let them have a go before recording. Attach a clean, disposable one-way mouthpiece to spirometer. Breathe in fully. Seal lips around mouthpiece. Breathe out as fast and hard as poss until nothing left (may take 15s; athletes = 3s). Repeat twice more. Should have 3 readings within 100mL or 5% of each other. Diagnosis: FEV1/FVC ratio = <0.7 = obstructive FEV1 = 55% = moderate COPD Flow-volume loops: Normal: 3 consistent loops needed Normal: rapid rise to max expiratory flow followed by steady, uniform decline until all air exhaled Obstructive: peak expiratory flow (PEF) ↓and decline in airflow to complete exhalation follows a distinctive dipping (concave) curve Severe obstruction: esp with emphysema; ‘steeple’ pattern Restrictive: normal in shape but absolute ↓ in volume Coughing during exhalation: abrupt drop in flow and a short intake of air with the start of the cough Slow start to forced exhalation Extra breath: abrupt, short plateau Early stoppage: normal pattern but reaches a plateau abruptly Management e.g. overall plans, referrals to other services Treatment Biological e.g. specific drugs Treatment - Social Differential diagnosis FVC: total vol of air expelled during forced maximal expiration following maximal inspiration (breathing as hard and fast as poss) VC: the same as FVC except exhaled naturally and slowly; not forced. FVC = VC in healthy people PEF: the greatest flow that can be sustained for 10ms on forced expiration starting from maximal inspiration (monitors conditions of upper/large airways) CXR: looks normal but overinflation of lungs (big black fields), flattened diaphragms, ?large bullae, blood vessels may be ‘pruned’ with large proximal blood vessels but small vessels in the periphery Hb level may be raised due to prolonged hypozaemia (ie secondary polycythaemia) Sputum examination not useful normally as Strep. pneumonia and H. influenzae produce acute exacerbation ECG: in advanced cor pulmonale, p waves taller and ?right bundle branch block Smoking cessation (slows rate of progression and prolong time before disability and death occur) and drug therapy (shortterm for acute exacerbations, long-term for symptom relief) Green inhaler is salmeterol = long acting version of the blue inhaler Brown is steroid Blue is salbutamol Bronchodilators, corticosteroids, Abx, antimucolytics (carbocisteine) for 4 weeks, diuretics, oxygen therapy at 2L/min via nasal cannulate to achieve O2 sats >90% 18 million lost work days for men, and 2 million for women; 7% of total lost work days each year. Clinical feature COPD Asthma Smoker/ex-smoker Nearly all Possibly Symptoms <35yo Rare Often Chronic productive cough Common Uncommon Breathlessness Persistent and progressive Variable Night time waking with SOB Uncommon Common Significant diurnal/day-to-day variation Uncommon Common Serial peak flow monitoring, looking for diurnal variation of greater than 20%, may help to differentiate these conditions The NICE guidelines suggest that bronchodilator reversibility testing is not routinely used where the clinical features and spirometry strongly indicate COPD. If there is any doubt, reversibility testing can be performed at a clinic visit (>400mL response to bronchodilator) or after a 2 week trial of prednisolone 30mg daily. Alternatively, spirometric and clinical response to a month’s trial of bronchodilator therapy can be assessed. Reversibility testing is not a ‘gold standard’ and the results must be interpreted alongside the clinical history. Disorder– core Who does it affect Core symptoms Signs Biological causes/risk factors Pneumothorax ‘air in the pleural space’; tension pneumothorax = MEDICAL EMERGENCY Young males, M:F = 6:1; caused by rupture of a pleural bleb (usually apical), ?due to congenital defects in alveolar connective tissue, pts are tall and thin, if pt >40yo then usually due to COPD Sudden onset of unilateral pleuritic pain or progressive breathlessness; as pneumothorax develops, pt becomes more SOB, tachycardic and pale If small, ?none; otherwise; hyperresonant chest on percussion and diminished breath sounds on affected side, reduced expansion on affected side; if tension pneumothorax, trachea will be deviated away from the affected side; tachycardic, hypotensive, resp distress, distended neck veins, 1. Spontaneous: young thin men due to rupture of a subdural bulla 2. Result of trauma to chest: 3. Rarer: asthma, COPD, TB, pneumonia, lung abscess, Ca, CF, fibrosis, sarcoidosis, connective tissue disorders (Marfan’s, Ehlers-Danlos syndromes) 4. Iatrogenic: insertion of a CVP line, pleural aspiration, biopsy, percutaneous liver biopsy, positive pressure ventilation 1. Localised: if visceral pleura has previously become adhered to parietal pleura 2. Generalised: if no pleural adhesions Usually the pressure in the pleural space is –ve; this is lost once there’s a communication with atmospheric pressure. The elastic recoil of the lungs causes the partial deflation. Once this communication is obliterated, then air will be reabsorbed at a rate of 1.25% of the total radiographic volume of the hemithorax/day (a 50% collapse of lung will take ~40days to reabsorb completely) Investigations e.g. to confirm diagnosis, Management Tension pneumothorax: valvular mechanism = air is sucked into pleural space during inspiration but can’t leave during expiration. This causes a continual +ve intrapleural pressure, the lung deflates further, and mediastinum shift results; compression of great vessels and cardiorespiratory arrest will occur CXR: should not be performed if suspect a tension pneumothorax otherwise request an expiratory film (CXR are usually on inspiration) ABG: Pneumothorax due to trauma or mechanical ventilation requires a chest drain OHCM: 1. Primary: SOB and/or rim of air >2cm on CXR: a. No = discharge b. Yes = aspirate, if successful then discharge and if not then put in a chest drain 2. Secondary: SOB and age >50yo and rim of air >2cm a. No: aspirate and if successful admit for 24hrs b. Yes: chest drain Disorder– core How common is it Who does it affect Core symptoms Signs Biological causes/risk factors Pneumonia = an acute LRTI associated with fever, symptoms and signs in chest, and abnormal CXR; due to inflammation of the substance of the lungs; Incidence = 1-3/1000/year; mortality = 10% (pts admitted to hospital) Dangerous condition among >70yo Acute cough, purulent sputum, fever, rigors, malaise, anorexia, dyspnoea, haemoptysis, ?pleuritic pain Signs of consolidation of the lung eg reduced expansion, dull to percuss, increased tactile vocal fremitus, bronchial breathing, pleural rub, bibasal crackles if pleural effusion; evident signs on a CXR; fever; cyanosis, confusion (in elderly), tachypnoea, tachycardia, hypotension, Site: Localised – whole of one or more lobes = lobar pneumonia Diffuse – primarily affects the lobules of the lung, often in association with bronchi and bronchioles = bronchopneumonia Aetiology: can be found in 75% of pts Community-acquired pneumonia (CAP): may be primary or secondary to underlying disease Streptococcus pneumoniae is commonest cause; then H influenzae, Mycopasma pneumonia; Staph A, Legionella speciies, Moraxella catarrhalis and Chlamydia = rest of bacteria; G-ve and anaerobes are rare; viruses only 15% Hospital-acquired pneumonia (HAP): acquired >48hrs after hospital admission; most commonly due to G-ve bacteria or Staph A; anaerobes; also Pseudomonas, Klebsiella, Bacteriodes, Clostridia Aspiration of vomit (=chemical cause): occurs in those with stroke, myasthenia, bulbar palsies, decreased consciousness (drunk), oesophageal disease (achalasia, reflux), poor dental hygiene; Staph pneumoniae and anaerobes Immunocompromised pt: Strep pneumoniae, H influenza, Staph A, M catarrhalis, M pneumoniae, G-ve bacilli, Pneumoncystic jiroveci (used to be named P carinii); fungi; viruses Radiotherapy Allergic mechanisms Usually caused by bacteria Pathogen Information Pneumococcal Ie Streptococcal pneumoniae; commonest; affects all ages esp elderly, alcoholics, post-splenectomy, immunosupprssed, pts with HF or pre-existing lung disease; CXR shows lobar consolidation Staphylococcal Rarer cause; may complicate influenza infection or occur in young, IVDU, pts with underlying disease (CF, leukaemia); CXR shows bilateral cavitating bronchopneumonia Klebsiella Rare; occurs in elderly pts with heart or lung disease, diabetes, alcoholics, malignancy. The onset is often sudden, with severe systemic upset. The sputum is purulent, gelatinous or bloodstained. CXR shows cavitating pneumonia of upper lobes and bulging of fissures. Pseudomonas Common in bronchiectasis, CF pts and HAP pts. Isolation of bacteria may just be an artefact as it grows well on agar gels. M pneumoniae Occurs in epidemics every 4 years; present with flu-like symptoms (headaches, arthralgia, myalgia) followed by a dry cough; frequent in teens and twenties; CXR shows usually one 1 lobe but sometimes bilateral, patchy consolidation. Legionella Colonises water tanks kept at <60°C eg air-conditioning and hot water systems => pneumophilla Legionnaire’s disease; flu-like symptoms then a dry cough and dyspnoea Three epidemiological patterns of Legionnaires’ disease are recognized: 1. outbreaks among previously fit individuals staying in hotels, institutions or hospitals where the shower facilities or cooling systems have been contaminated with the organism 2. sporadic cases where the source of the infection is unknown; most cases involve middle-aged and elderly men who are smokers, but it is also seen in children 3. outbreaks occurring in immunocompromised patients, e.g. on corticosteroid therapy. Half of the patients have gastrointestinal symptoms, with nausea, vomiting, diarrhoea and abdominal pain. Patients may be acutely ill, with mental confusion and other neurological signs. Haematuria occurs and occasionally renal failure. The patient is tachypnoeic with an initially dry cough that later may become productive and purulent. The chest X-ray usually shows lobar and then multilobar shadowing, sometimes with a small pleural effusion. Cavitation is rare. Chlamydia pneumoniae Chlamydia psittaci Viral pneumonia Pneumocystis pneumonia (PCP) H influenzae Moraxella Investigations e.g. to confirm diagnosis, exclude physical causes etc Management e.g. overall plans, referrals to other services Treatment Biological e.g. specific drugs Commonest chlamydial infection; person-to-person spread via biphasic illness: pharyngitis, hoarse voice, ottitis then pneumonia Causes psittacosis, an ornithosis acquired from infected birds (parrots); headache, fever, dry cough, lethargy, athralgia. The incubation period is 1–2 weeks and the disease may pursue a very low-grade course over several months. The liver and spleen are occasionally enlarged, and scanty ‘rose spots’ rash may be seen on the abdomen. CXR shows patchy consolidation Rare. More often, viral infection predisposes patients to bacterial pneumonia by damaging the respiratory epithelium and facilitating bacterial infection. Avian influenza (influenza A; H5N1): normally does not affect humans but can be transmitted from poultry (where it causes avian flu), when there has been unusually close contact. Patients present with fever, breathlessness, cough and diarrhoea. Lymphopenia and thrombocytopenia are present and pulmonary infiltrates are seen on chest X-ray. There is a >50% mortality. Tamiflu (oseltamivir) reduces morbifity by 1-2 days. Severe acute respiratory syndrome (SARS): Caused by SARS-COV virus – a coronavirus. The incubation period is approximately 5 days with spread between humans occurring mainly by droplet infection. Fever, malaise, headache and rigors were followed in the second week by dry cough, breathlessness and diarrhoea. Mortality is 1-50% depending on age; mechanism of transmission is only by close contact of infected pt. supportive management. Causes pneumonia in immunosuppressed eg HIV; caused by penumocystis jiroveci (formerly carinii); dry cough, SOBOE, fever, bilateral creps, CXR normal of perihilar shadowing Frequent cause of exacerbation in pts with COPD of chronic bronchitis; pneumonia may be diffuse or localised; no special features to separate it from other bacterial infections. Treat with amoxicillin Also exacerbations of COPD Precipitating factors: Strep. pneumoniae – often follows viral infection with influenza or parainfluenza. Hospitalized ‘ill’ patients – often infected with G-ve organisms. Cigarette smoking (the strongest independent risk factor for invasive pneumococcal disease). Alcohol excess. Bronchiectasis (e.g. in cystic fibrosis). Bronchial obstruction (e.g. carcinoma) – occasionally associated with infection with ‘nonpathogenic’ organisms. Immunosuppression (e.g. AIDS or treatment with cytotoxic agents) – organisms include Pneumocystis jiroveci, Mycobacterium avium-intracellulare, cytomegalovirus. Intravenous drug users – frequently associated with Staph. aureus infection. Strep. pneumoniae – often follows viral infection with influenza or parainfluenza. CXR: will show area of consolidation; though radiology often lags behind so may be no signs early on and will take ~6wks to resolve; if it doesn’t resolve after 6wks it suggests there may be something else (eg bronchial carcinoma with persisting secondary pneumonia) Bloods: FBC for raised WCC, U and E, LFT, raised CRP ESR, blood cultures Sputum: for MCS, esp if severe case and not clearing Bronchoscopy/bronchoalveolar lavage: if pts is immunocompromised or on ITU Establish diagnosis, identify pathogen, assess severity Severity testing: use CURB-65 score for CAP Confusion Urea: >7mmol/L Respiratory rate: >30/min BP: <90 systolic and/or <60 diastolic >65yo 0-1 = treat at home 2 = treat in hospital 3 or more = severe pneumonia (ABG/O2 sats of <8KPa/92%; co-morbidity; multilobar/bilateral involvement also indicate severe disease) Abx; oral if not severe O2 if low sats IV fluids if anorexia, shock or dehydration Complication Analgesia if pleurisy ITU if shock, hypercapnia, uncorrected hypoxia; if CRP remains high or failure to improve then look for progression/complications. Pneumoccocal vaccine: Offer to at risk groups: >65yo; chronic heart, liver, kidney or lung failure/conditions; DM; immunosurpressed (small spleen (splenectomy, asplenia, sickle cell, celiac); AIDS, chemotherapy Respiratory failure: type 1 respiratory failure (PaO2 <8kPa) is relatively common; treat with highflow O2 (60%); transfer the pt to ITU if they do not improve or PaCO2 rises to >6kPa Hypotension: due to vasodilation and dehydration because of sepsis; if <90mmHg systolic then give a 250mL colloid/crystalloid fluid challenge over 15min; give Adr if BP does not rise Atrial fibrillation: quite common and resolve often with treatment of AF Pleural effusion: inflammation of the pleura by adjacent pneumonia may cause fluid exudation into the pleural space; if it accumulates faster than it is resorbed then an effusion develops; if it is large enough it may require draining; it could become infected (empyema) Empyema: pus in the pleural space; suspect if a pt with a resolving pneumonia keeps spiking a fever; clinical signs and CXR show an effusion; aspirated fluid is yellow; insert a chest drain Lung abscess: is a cavitating area of localised suppurative infection within the lung; caused by: aspiration (commonest) eg heavy alcohol users following aspiration pneumonia; bronchial obstruction eg tumour, foreign body; pulmonary infarction; septic emboli eg septicaemia, IVDU, right heart endocarditis; clinical presentation: swinging fever, cough, purulent foul-smelling sputum, pleuritic chest pain, haemoptysis, malaise, weight loss, clubbing, anaemia, crepitations Septicaemia: due to bacterial spread from lung parenchyma into the bloodstream and may cause ‘metastatic infection’ (meningitis, infective endocarditis) Pericarditis/myocarditis: may complicate pneumonia Cholestatic jaundice: due to sepsis or secondary to Abx therapy (fluoxacilin or co-amoxiclav) Disorder– core How common is it Core symptoms Signs Screening questions to ask Biological causes/risk factors Asthma ‘chronic inflammatory condition of lung airways; classically has 3 characteristics: Reversible airflow lmititation (spontaneously or with treatment) Airway hyperresponsiveness Inflammation of the bronchi with T cells, mast cells, eosinophils and smooth muscle hypertrophy, mucus plugging and epithelial damage’ Prevalence is increasing especially amongst children and young adults where = 15%; asthma more common in developed countries; 300million people have asthma worldwide Wheezing attacks and episodic SOB often worse at night (diurnal variation); ‘chest tightness’; cough or nocturnal cough may be the main feature in children; great variation in frequency and duration of episodes Tachypnoea, audible polyphonic wheeze, hyperinflated chest, hyperresonant percussion, diminished air entry; severe attack = inability to complete sentences, pulse >110bpm, RR >25/min, PEFR 33-55% predicted; life-threatening attack = silent chest, cyanosis, bradycardia, exhaustion, confusion, feeble respiratory effort, PEFR <33% Precipitants: cold air, exercise, emotion, allergens (house dust mite, pollen, animal fur) Diurnal variation: in symptoms or peak flow; marked morning dipping Exercise: quatify exercise tolerance Disturbed sleep: quantify as nights/week (sign of severe asthma) Acid reflux: known association with asthma Other atopy: hayfever, eczema, allergy, Fx The home esp bedroom: pets, carpet, feather pillows, soft furnishings (floor pillows) Occupation: if symptoms resolve at the weekends or on holiday then may be something at work Days off week/school: Classified as: Intrinsic: definite external cause; oftens arts in middle-age (late onset) though these pts often have a Hx of respiratory problems indicative of asthma Extrinsic: no causative agent found; frequent in atopic individuals who are skin prick +ve for dustmite, aimal dander, pollen; +ve skin prick in 90% children and 70% adults with persistent adults; late onset in adults causes may be via sensitization of chemicals at work Atopy and allergy Atopy = hayfever (allergic rhinitis), eczema and asthma; tend to run in families Genetic: Control production of cytokines – IL-3, 4, 5, 9, 13 and GM-CSF; affect mast cell and eosinophil development ADAM 33 (a disintegrin and metalloproteinase) – airway hyperesponsiveness and tissue remodelling Environment: Early childhood exposure to allergens and maternal smoking influences IgE production Hygiene hypothesis: growing up in clean environments predisposes us to a IgE response to allergens and a TH2 response Pathogenesis: Complex, not fully understood; severity and chronicity of asthma dependent on airway inflammation and remodelling; driven by Th2-type T lymphocytes which facilitate IgE synthesis through production of IL-4 and eosinophilic inflammation through IL-5. However, as the disease becomes more severe and chronic and loses its sensitivity to corticosteroids, there is greater evidence of a Th1 response with release of mediators such as TNF-α and associated tissue damage, mucous metaplasia and aberrant epithelial and mesenchymal repair. Inflammation: Mast cells: increased numbers, release preformed mediators eg histamine that act on smooth muscle, blood vessels and sensory nerves; inhibited by sodium cromoglycate and β2-agonists which helps to prevent bronchoconstriction. Mast cells also release cytokines and chemokines that act in late response and more chronic aspects of asthma. Eosinophils: increased numbers in bronchial wall and secretions of asthmatics; drawn there by IL-3, 5 and GM-CSF; decreased numbers and activation by steroids Dendritic cells and lymphocytes: increased numbers in mucous membranes of airways and alveoli; CD4+ T helper cells release cytokines that help mast cells migrate and activate. IL-4 and 13 also help maintain proallergic response (Th2) which favours switch of AB production to IgE. Remodelling: alteration of structure and function of airways Epithelium: loss of ciliated cells; metaplasia with an increased number of mucus-secreting goblet cells; damage to epithelium makes it more susceptible to viral infection (rhinovirus, coronavirus) and to effects of pollutants; also increased production of nitric oxide due to increased expression of NO synthase in epithelia Basement membrane: deposition of repair collagens I, III and V by myofibroblasts and proteoglycans in lamina reticularis beneath BM => thickened BM; Smooth muscle: hyperplasia of smooth muscle alters in function so it contracts easier and stays contracted because of changes in crosslinking; smooth muscle also secretes cytokines and chemokines that sustain chronic inflammatory response; ADAM33 involved in driving smooth muscle responses Nerves: contribute to irritability of asthmatic airways o central reflexes via stimulation of nerve endings in the epithelium and submucosa => release of ACh from nerve endings to stimulate M3 receptors on smooth muscle to cause contraction o local/peripheral reflexes and effect on smooth muscle via release of neuropeptides (substance P: contraction; CGRP: vasoconstrictors; neuropeptide Y and VIP: vasodilation) Investigations e.g. to confirm diagnosis, exclude No single test to confirm asthma in all pts. physical causes etc Lung function tests: PEFR on waking prior to bronchodilator and before bed after bronchodilator; demonstrates variable airflow limitation (diurnal variation is a good measure of activity and helps in long term assessment and response to treatment); to assess occupational asthma, PEFR needs to be measured for 2wks during work and 2wks off work. Spirometry: good for assessing reversibility = diagnosis if >15% improvement in FEV1 or PEFR following inhalation of a bronchodilator (nb reversibility may not be present asthma is in remission or chronic asthma with little reversibility present. Exercise tests: Widely used for diagnosis in children; run for 6mins on a treadmill so HR >160bpm; or cold air challenge but a –ve result doesn’t rule out asthma. Management e.g. overall plans, referrals to other services Treatment Biological e.g. specific drugs Histamine/methacholine bronchial provocation test: indicates presence of airway hyperreesponsiveness and should be used if main symptom remains cough. Exercise testing is easier. Trial of corticosteroids: prednisolone 30mg daily for 2wks with lung function measured before and immediately after the course. >15% improvement diagnostic Blood and sputum: increased eosinophils; not so useful CXR: no diagnostic features, though overinflation is characteristic during an acute episode; good to exclude a pneumothorax which can be a complication Skin prick tests: performed in all cases to help identify allergic causes Allergen provocation tests: not required unless ?occupational asthma (+ ?food; in the absence of any obvious allergy eg peanut or milk, if the pt has asthma w/o any other systemic features then it is unlikely to be caused by food); open food challeneges are unreliable (should be blind) Aims: Abolish symptoms Restore normal/ best possible lung function Reduce risk of severe attacks Enable normal growth in children Minimise absence from school or work => education about asthma and treatment, avoidance of identified causes, use of lowest effective and convenient medications Control of extrinsic factors: Avoidance of household dust mite is difficult – no evidence that physical or chemical measures benefit; use of covers for bedding and changes to accommodationalso has no benefit; smoking should be stopped; β-blockers should be stopped; avoid all NSAIDs if intolerant of aspirin Delivered as aerosols or powders into the lungs – drugs delivered direct, avoid first pass metabolism, lower doses needed, fewer systemic effects 3 key points: 1. Asthma involves self-management with treatment and PEFR 2. Asthma is an inflammatory condition so anti-inflammatory meds needed even if mild case 3. Short acting bronchodilators only relieve breakthrough symptoms; increased use of them indicates worsening disease Use of a metered-dose inhaler 1. The canister is shaken. 2. The patient exhales to functional residual capacity (not residual volume), i.e. normal expiration. 3. The aerosol nozzle is placed to the open mouth. 4. The patient simultaneously inhales rapidly and activates the aerosol. 5. Inhalation is completed. 6. The breath is held for 10 seconds if possible. Even with good technique only 15% of the contents is inhaled and 85% is deposited on the wall of the pharynx and ultimately swallowed. NB Chlorofluorocarbon (CFC) propellants have been/are being replaced by hydrofluoralkane (HFA) propellants. The new aerosols may feel and taste different and patients need reassurance of their efficacy. Spacers These are plastic conical spheres inserted between the patient’s mouth and the inhaler. They are designed to reduce particle velocity so that less drug is deposited in the mouth. Spacers also diminish the need for coordination between aerosol activation and inhalation. They are useful in children and in the elderly and they reduce the risk of candidiasis. Short-acting relievers Inhaled β2 agonists (e.g. salbutamol (albuterol in USA), terbutaline) Long-acting relief/disease controllers Inhaled long-acting β2 agonists (e.g. salmeterol, formoterol) Inhaled corticosteroids (e.g. beclometasone, budesonide, fluticasone) Compound inhaled salmeterol and fluticasone Sodium cromoglicate Leukotriene modifiers (e.g. montelukast, zafirlukast, zileuton) Other agents with bronchodilator activity Inhaled antimuscarinic agents (e.g. ipratropium, oxitropium) Theophylline preparations Oral corticosteroids (e.g. prednisolone 40 mg daily) Steroid-sparing agents Methotrexate Ciclosporin Intravenous immunoglobulin Anti-IgE monoclonal antibody – omalizumab Etanercept (p. 76) Β2 agonists (not antagonists!) are selective for the lungs (β1 are found in the heart) DD Prognosis The sites of action of NSAIDs (e.g. aspirin, ibuprofen) are shown. The enzyme cyclo-oxygenase occurs in three isoforms, COX-1 (constitutive), COX-2 (inducible) and COX-3 (in brain). PG, prostaglandin; BLT, B leukotriene receptor; cysLT, cysteinyl leukotriene receptor. Pulmonary oedema (‘cardiac asthma’), COPD, large airway obstruction, SVC obstruction (wheeze/dyspnoea not episodic), pneumothorax, PE, bronchiectasis Most childhood asthmatics grow out of it in adolescence or suffer much less as adults Disorder– core Core symptoms Signs Biological causes/risk factors Investigations e.g. to confirm diagnosis, exclude physical causes etc Management Pleural effusion = fluid in the pleural space Divided by their protein concentration: transudates (<25g/L) and exudates (>35g/L) Asymptomatic, or dyspnoea and pleuritic chest pain Decreased chest expansion Sony dull percussion note Diminished breath sounds on the affected side Tactile vocal fremitus and vocal resonance are decreased Large effusions may cause tracheal deviation away from effusion Lung above effusion may be compressed so bronchial breathing 1. Transudates: May be due to increased venous pressure (HF, constrictive pericarditis, fluid overload) or hypoproteinaemia (liver failure, cirrhosis, malabsorption, nephrotic syndrome) and Meig’s syndrome (right pleural effusion and ovarian fibroma) 2. Exudates: mostly due to increased ‘leakiness’ of pleural capillaries secondary to infection, inflammation, malignancy (pneumonia, TB, pulmonary infarction, RA, SLE, lymphoma, lung Ca) CXR: Small effusions blunt the costophrenic and costocardiac angles Larger effusions are seen as water-dense shadows with concave upper borders (a meniscus); a completely horizontal upper border = pneumothorax as well! US: useful in guiding diagnostic or therapeutic aspiration Drainage: if effusion is symptomatic then drain it; best remove fluid slowly (<2L/24hrs) Pleurodesis: if recurrent effusions Disorder– core How common is it Who does it affect Core symptoms and signs Biological causes/risk factors Pulmonary embolism Post-mortem studies show microemboli are present in up to 60% of people, but not usually diagnosed that frequently. 10% of clinical PE are fatal. Depend on number, size and location of emboli Sudden onset of dyspnoea commonest and ?only symptom; many occur silently! Pleuritic chest pain and haemoptysis are only present in lung tissue is infracted Three main scenarios: 1. Small/medium PE: embolus has impacted at a terminal pulmonary vessel; haemoptysis occurs in 30% 3 or more days after initial event; pt is tachypnoeic with localised pleural rub and often coarse crackles over area involved; exudative pleural effusion may develop; pt may have a fever; CV exam normal 2. Massive PE: much rarer; sudden collapse occurs due to obstruction of RV outflow tract; central chest pain, shocked, pale, sweaty, syncope, death; pt is tacypnoeic, tachycardic with hypotension and peripherally shutdown; raised JVP with prominent ‘a’ wave; right ventricular heave present, gallop rhythm, a split 2nd heart sound; usually no abnormal chest signs. 3. Multiple recurrent PEs: increased SOB over several weeks/months; weakness, syncope on exertion and occasionally angina; physical signs are due to pulmonary hypertension; signs of right ventricular overload with right ventricular heave and loud pulmonary second sound. Look for signs of a cause – DVT? Scars? Thrombus formed in the systemic veins esp of pelvis, abdomen or legs (DVT), or sometimes the right heart (<10% cases, post-MI or septic emboli due to RHS endocarditis); clots can sometimes break off, flow back to the, through RHS of heart to lungs and cause a PE. Other thrombi can arise from: fat (from long bone #), air, amniotic fluid, malignancy, parasites/ foreign material (IVDU) Clots form due to change in Virchow’s triad: Modern Notes Altered blood flow These include turbulence, stasis, mitral stenosis, and varicose veins. Altered vessel Injuries and/or trauma to endothelium includes damage to the veins arising from shear stress or hypertension. Hyperviscosity, deficiency of antithrombin III, nephrotic syndrome, Altered blood constituents changes after severe trauma or burn, disseminated cancer, late = hypercoagulability pregnancy and delivery, race, age, smoking, and obesity. Risk factors: same as for DVT and general thrombosis formation Patient Factors Disease or surgical procedure Increasing age Trauma/ surgery to lower limb, pelvis, hip BMI >30Kg/m2 (obese) Malignancy Varicose veins Cardiac/ respiratory failure Continuous travel for >3hrs in preceeding 4 wks Recent MI or stroke Immobility/ bedrest >4days Acute medical illness/ infection Pregnancy IBD Previous DVT or PE Nephrotic syndrome Thrombophilia Myeloproliferative disorders Antithrombin deficiency Sickle cell anaemia Protein C or S deficiency Central venous catheter Factor V Leiden Paraproteinaemia Prothrombin gene variant Antiphospholipid antibody/ lupus anticoagulant Paroxysmal nocturnal haemoglobinuria Oestrogen therapy inc the pill and HRT Plasminogen deficiency DVT occur in 50% pts after a prostatectomy (w/o prophylactic heparin) of following a CVA; 10% of pts following an MI The problems? 1. Lung tissue is ventilated but not perfused = increased intrapulmonary dead space and decreased gas exchange. After a few hours, the lung tissue then stops producing surfactant => lung collapse => increased hypoxaemia. 2. Decreased cross-sectional area of pulmonary arterial bed => increased pulmonary arterial pressure (pulmonary hypertension) and a decreased cardiac output Zone of lung no longer perfused => can infarct but often doesn’t because lungs are still supplied with O2 by bronchial circulation and the airways Bloods: FBC (polymorphonuclear leucocytosis, elevated ESR), U and E (increased LDH), clotting, D-dimers (only do in pts without a high probability of a PE; -ve result excludes PE and imaging not required) ABG: may show low PaO2 and normal/ low PaCO2 (type 1 respiratory failure) CXR: may be normal or show oligaemia of affected segment, dilated pulmonary artery, linear atelectasis, small plural effusion, wedge-shaped opacities (pul infarct) or cavitation (rare) ECG: may be normal, tachycardic, AF, RBBB, right ventricular strain (inverted T wave in V1-4) with subsequent right-axis deviation, right atrial dilatation (tall, peaked P waves); classical S wave in lead I and a Q wave and inverted T wave in lead III (S1Q3T3) is rare. Can also do: Radionuclide V/Q scanning: Pulmonary 99mTc scintigraphy demonstrates underperfused areas which, if not accompanied by a ventilation defect on a ventilation scintigram performed after inhalation of radioactive xenon gas (see p. 824), is highly suggestive of a PE. (though if PE has caused an infarct, then this will be ‘matched‘ = normal result = false -ve) US: detect pelvic or iliofemoral veins for clots CT angiography/ MRI: good predictive value Echo: shows a vigorously contracting left ventricle and occasionally a dilated right ventricle Treatment: High-flow O2 (60-100%) unless they have lung disease (COPD) If infarct, then bed rest and analgesia ?severe: IV fluids and inotropic drugs to improve pumping of right heart Fibrinolytics: streptokinase IV over 30mins; confer greater survival in massive PE Surgical embolectomy rarely necessary but may be if haemodynamic circumstances are severe 3. Investigations e.g. to confirm diagnosis, exclude physical causes etc Treatment Biological e.g. specific drugs Prevention: Anticoagulate: LMWH and warfarin 10mg; stop LMWH when INR >2-3 and continue warfarin for 3months If high-risk where anticoagulation contraindicated or where multiple emboli still occur, insert a filter in the inferior vena cava via femoral vein above the level of the renal veins (but keep pt on anticoagulation) Disorder– core How common is it Who does it affect Core symptoms Signs of advance disease Bronchial carcinoma: divided into small-cell (SCC) and non-small cell carcinoma (NSCC) Bronchial carcinoma = 95% of all primary tumours of lung; alveolar = 2% and others = 3% Most common malignant tumour world-wide with 1.3 million death/year; 3rd most common death after heart disease and pneumonia in UK; highest mortality in Scotland; in UK 32,000 die/year M 3x> F; levelled off in men but causes more deaths from malignant disease in women than any other, even breast cancer Cough (41%); chest pain (22%); cough and pain (15%); haemoptysis (7%); dyspnoea; chest infection, malaise, anorexia and weight loss, SOB, hoarseness, distant spread, no symptoms (each <5%); chest pain is described as a ‘fullness’ and ‘pressure within the chest’ 1. Chest signs; none or consolidation; collapse (Ca=commonest cause of collapse in adult); pleural effusion 2. Extrapulmonary manisfestations: rare, except for clubbing; supraclavicular lymph nodes Metabolic (universal at some stage) Loss of weight = cachexia Lassitude Anorexia Endocrine (10%) (usually small-cell carcinoma) Ectopic adrenocorticotrophin syndrome Syndrome of inappropriate secretion of antidiuretic hormone (SIADH) = ↓Na+ and ↑ADH Hypercalcaemia (usually squamous cell carcinoma) due to bony mets Rarer: hypoglycaemia, thyrotoxicosis, gynaecomastia Neurological (2–16%); confusion, fits, focal CNS signs, cerebellar syndrome Encephalopathies – including subacute cerebellar degeneration Myelopathies – motor neurone disease Neuropathies – peripheral sensorimotor neuropathy Muscular disorders – proximal polymyopathy, myasthenic syndrome (Eaton–Lambert syndrome) Biological causes/risk factors Investigations e.g. to confirm Vascular and haematological (rare) Thrombophlebitis migrans Non-bacterial thrombotic endocarditis Microcytic and normocytic anaemia Disseminated intravascular coagulopathy Thrombotic thrombocytopenic purpura Haemolytic anaemia Skeletal Clubbing (30%) Hypertrophic osteoarthropathy (HPOA) (± gynaecomastia) (3%) = wrist pain Cutaneous (rare) Dermatomyositis Acanthosis nigricans Herpes zoster Development from initial malignant change to presentation takes: 15 years with adenocarcinoma 8 years with squamous carcinoma 3 years for SCC Most important distinction is between SCC and NSCC NSCC: Squamous or epidermoid carcinoma is the commonest type = 40% of all carcinomas; most present as obstructive lesion of the bronchus leading to infection; cells are well-differentiated usually; local spread common but widespread metastases occur late Adenocarcinoma= 10% of all carcinomas; arises from mucus cells in bronchial epithelium; invasion into pleura and mediastinal lymph nodes common, as are mets to the brain, adrenal glands and bone; associated with asbestos, non-smokers, women, elderly, Far East Large cell carcinoma = 25% of all lung cancers; less differentiated forms of squamous cell and adenocarcinomas; metastasize early Bronchoalveolar cell carcinoma (‘bronchiolar carcinoma’) = 1-2% of lung tumours SCC: SCC = 20-30% of tumours; arises from endocrine cells (Kulchitsky cells), which are members of the APUD system and explains why they secrete many polypeptide hormones; some of these hormones stimulate tumour growth (autocrine mechanism); metastasizes early and almost always inoperable at presentation; responds to chamo and radio but poor prognosis RF: Smoking; passive smoking increased risk by 1.5 Urban areas Occupation: asbestos, ?coal tar, coal combustion products, arsenic, petrol products, radiation (radon), iron oxides; tend to be adenocarcinomas CXR: if cancer is causing symptoms, it will be visible on CXR; asymptomatic tumour visible if >1cm diameter; lateral views used to assess hilum and behind heart; isolated haemoptysis with normal diagnosis, exclude physical causes etc Management must reflect prognosis Treatment Biological e.g. specific drugs CXR is normally –ve, though further tests should be done esp if >40yo and smoker; 70% Ca present as circular masses with fluffy or spiky/ spiculated appearance = invasive; adenocarcinomas = often at periphery; may cause 2° pneumonia = consolidation (by blocking mucociliary escalator), pleural effusions (and lymphangitis carcinomatosa = streaky shadowing through lung fields) and collapsed lobes (PET)-CT: detecting small tumours esp of the mediastinum, staging the tumour; scanning should also include liver, brain and adrenal glands for mets MRI is not useful Fibreoptic bronchoscopy: to define anatomy, obtain biopsy and cytological samples; if tumour involves first 2cm of either main bronchus then it is inoperable; widening and loss of sharp angle of carina suggests enlarged mediastinal lymph nodes Peripheral aspiration and biopsy: for peripheral lung lesions that can not be seen by bronchoscopy Bloods: FBC (anaemia), LFT (liver mets?), U and E (hypercalcaemia, hyponatraemia) 20% alive at 1 year after diagnosis; 6-8% after 5 years (nb 50% for breast and cervix) Non small cell: 50% 2yr survival without mets, with mets 10%. Small cell: median survival = 3months untreated, 1-1.5yrs treated. 1. NSS: staged according to TNM staging; excision if peripheral. Radiotherapy +/- chemo (if advanced)→platinum based with monoclonal antibodies targeting epidermal growth factor receptors (cetuximab) 2. SCC: treated as to whether it is limited or extensive as nearly always mets at presentation; chemotherapy DD Complications Other tumours Surgery: curative in NSS (T1, N0, M0) but on 10% cases suitable; 70% of which survive for 5 years; rarely appropriate for >65yo as operative mortality risk exceeds 5-year survival rate Radiotherapy for cure: in pts who have a slow growing squamous carcinoma Radiatherapy for symptoms: bone pain, haemoptysis and SVC obstruction Chemotherapy: for advanced NSCC or SCC Laser therapy, tracheobronchial stents: palliative care if breathing difficulties via tumour compression Palliative care: steroids to improve appetite, morphine for pain, laxatives, bronchodilators, codeine (cough suppressants) short courses of radiotherapy for bone pain, counselling Pneumonia, TB Direct spread: Into pleura or ribs to cause pleuritic pain From apex of lung into brachial plexus = pain in shoulder and down inner surface of the arm (Pancoast’s tumour); involvement of sympathetic ganglion = Horner’s syndrome Hilar tumours = involve left recurrent laryngeal nerve causing unilateral vocal cord paresis with hoarseness and bovine cough Invasion of phrenic nerve = paralysis of ipsilateral hemidiaphragm Invasion into oesophagus = progressive dysphagia Into pericardium = pericardial effusion and malignant dysrhythmias SVC invasion = early morning headaches, facial congestion, oedema of upper limbs, distended jugular and chest veins Endocrine = ectopic hormone secretion in 10% SCC: SIADH, Cushing’s Metastatic complications: Bony mets = severe pain and pathological fractures (↑Ca2+, anaemia, bone pain) Liver mets Adrenal gland mets (latter only found at autopsy) = Addison’s Brain mets = change in personality, epilepsy or a focal neurological lesion; spinal cord compression Tracheal Carcinoma: rare; rapid and progressive dysphagia and stridor; ↓ inspiratory flow on flowvolume loops; confirm with bronchoscopy; v poor prognosis Secondary tumours: common, 1° sites include kidney (commonest), prostate, breast, bone, GIT, cervix, ovary; may be extensive on CXR but often asmptomatic Benign tumours: Pulmonary harmatoma: most common benign lung tumour; well-defined 1-2cm round lesion on CXR; slow growth Bronchial adenoma: rare, slow-growing, 90% are carcinoid and 10% are cylindromas Cylindroma, chondroma and lipoma: rare, grow in bronchus or trachea, cause obstruction Tracheal tumours: squamous papilloma, leiomyoma, haemangiomas and tumours of neurogenic origin Others Disorder– core Alopecia (hair loss) How common is it Who does it affect Core symptoms Signs Screening questions to ask Biological causes/risk factors Investigations Management Treatment Biological Treatment Psychological Treatment - Social Can be due to disorder of: 1. hair follicle in which scalp skin looks normal (non-scarring alopecia) = exclamation mark hairs present o Androgenic alopecia = male pattern baldness; most common typel depends on genetic factors and an abnormal sensitivity to androgens; presents in young men with frontal receeding, then thinning of the crown; +ve Fx; can also be present in females but presents at a later age and is milder with little frontal recession; if acne or menstrual disturbance present ?polycystic ovary syndrome. Treatment: 5% minoxidil lotion or oral finasteride (1mg OD) can help arrest growth or slightly promote regrowth, but lifelong treatment and may not work in 1/3 pts. Do not use finasteride in women as cause congenital abnormalities; use antiandrogen therapy instead. o Telogen effluvium: occurs some 3/12 after pregnancy or severe illness due to ‘stress’ putting all the hairs into telogen phase of shedding at the same time. o Alopecia areata (seen); autoimmune, presenting in children or young adults as patches of hair loss; these may regrow to be followed by new patches of hair loss; presence of exclamation mark hairs (narrow at scalp and wider and more pigmented at the tip) at the edge of the bald area is diagnostic; regrowth may be initially with white hairs and will take months; occasionally all the hair is lost (alopecia totalis) and rarely all body hair (alopecia universalis). Nails may be pitted or rough. Treatment: no effect on long-term progressionsteroids have no effect; wigs or support groups beneficial o Trichotillomania (self-induced hair-pulling) (seen) o Tinea capitis o Traction alopecia: due to pulling hair back into a bun or tight plaiting (mechanical damage); common in black Africans. o Metabolic (iron deficiency, hypothyroidism) o Drug (e.g. heparin, isotretinoin, chemotherapy) 2. disorder within the scalp that causes permanent loss of the follicle (scarring/ cicatrical alopecia) = shiny, atrophic areas in the scalp o Discoid lupus erythematosus o Kerion (tinea capitis) o Lichen planus o Dissecting cellulitis o X-irradiation o Idiopathic (‘pseudopelade’) Disorder– core How common is it Who does it affect Core symptoms Signs Screening questions to ask Features of the mental state Features/ symptoms of presentation in a primary care setting Sore throat Sore throat is the symptom the patient presents. Some doctors feel uncomfortable that without antibiotics a few patients may risk the complications. A review concluded that (1): antibiotics are unnecessary for most patients with sore throat as it is a self-limiting condition, which resolves by one week in 85% of people, whether it is due to streptococcal infection or not serious complications are rare the Centor criteria may be useful to predict patients who are at higher risk of Group A betahaemolytic streptococcus (GABHS) and complications, who may benefit from antibiotics tonsillar exudate tender anterior cervical lymph nodes absence of cough history of fever o in patients with tonsillitis who are unwell, and have three out of four of these criteria, the risk of quinsy is 1:60 compared with 1:400 in those who are not unwell if antibiotics are clinically indicated, phenoxymethylpenicillin is an appropriate first choice (adult dose: 500mg two to four times a day for 10 days) patients given antibiotics are more likely to reattend if they have another similar infection a delayed prescription, for use after three days if symptoms are not starting to resolve or are getting significantly worse, may be more appropriate for some patients offer advice and reassurance, and recommend analgesics for symptom relief in all patients As most patients with a sore throat do not see a doctor it is worth asking why they came. At any time 12 % of the population complain of a sore throat. Consultation rates are highest between age three and nine with a peak at age five to six; on average, 50 per 1000 patients consult their GP each year. Sore throat is rare: in infancy in those older than 50 years Surgery consultation rates for sore throat are between 41.2/1000 patients/ year and 57.6/ 1000 patients/year. History: The history should include: symptom duration absence or presence of trismus symptoms of systemic upset e.g. fever, malaise symptoms of dysphagia? rash? history of previous episodes? If there is stridor then this is an ominous sign. A child may complain of abdominal pain. A cough indicates a lower likelihood of streptococcal infection. Examination: General examination - assessment of how ill patient is e.g. pulse, temperature. Examine trunk for rash scarlet fever rash generally starts on the chest and spreads to involve the neck and face; there may be sparing of the circumoral area. The rash associated with infectious mononucleosis tends to be generalized. Examine the neck for cervical lymphadenopathy. Note any trismus or dribbling. Inspect the tongue and throat. In streptococcal disease there may be a 'strawberry tongue'. In cases of infectious mononucleosis there may be petichiae on the palate. Examine the tonsils. There may be hallitosis. If there is stridor then do not examine the throat because acute airways obstruction from epiglottitis may be provoked. Trismus = inability to open mouth fully Feature/ symptoms of presentation in a general hospital setting Biological causes/risk factors Investigations e.g. to confirm diagnosis, exclude physical causes etc Management e.g. overall plans, referrals to other services Treatment Biological e.g. specific drugs Treatment Psychological Treatment - Social The causes of acute sore throat include: viral infections adenoviruses, coxsachie, rhinoviruses and parainfluenzae viruses are isolated in 10 -20% of cases (1). bacterial infections (1) o 17% had a group A beta-haemolytic streptoccocus (GABHS) o 4% had group B,C, and D streptococci o 1% had other bacteria such as H.Influenzae or staph. aureus - these percentages should be interpreted with some caution as some of the organisms may be commensals o asymptomatic carriage of GABHS is also common, occuring in 6-40% of people (2) tuberculosis candidiasis chemical irritation NB. immunocompromised patients are more likely to have infections which may present as a sore throat. Causes of chronic sore throat include: irritation smoking is the most common cause. poor inhaler technique dust chemicals allergy candidiasis throat swabs - in general, throat swabs are of little value in the management of sore throat as up to 20% of patients carry strep. pyogenes as a commensal; there are no criteria for distinguishing between carriage and infection full blood count and monospot may be helpful if glandular fever or blood dyscrasia is suspected Although sore throat is the most common affliction, there is little concensus on management as it is usually difficult to distinguish the precise aetiological agent. Management of sore throat can be divided into: the management of the individual patient the general management of a practice population The management of the general population Factors that may be considered include: the effect of treatment - with a few exceptions a population treated with antibiotics improve about 24 hrs sooner time management: o short term it takes less time to write a prescription o long term it takes more time to explain but less consultations will be made if there is a consensus symptoms and signs that demonstrate bacterial and viral infection indication for antibiotics non infective causes of sore throat The management of the pt establish the reason for the consultation as most patients with a sore throat do not see a doctor - the sore throat may be 'the last straw ' establish the duration of the illness - infections usually resolve within five days review other risk factors consider aetiology of sore throat - most frequently look for features suggesting: o an infective cause o an indication for antibiotics treat according to practitioners' consensus soluble paracetamol or aspirin held in the mouth and then swallowed eases the discomfort When to make a referral Most children with recurrent sore throat can be managed in primary care. NICE has given guidance concerning referral if recurrent episodes of acute sore throat in children aged up to 15 years. NICE have suggested children should, however, be referred to a specialist service if (1): ****they have, or are suspected of having, a quinsy ****the swelling is causing acute upper airways obstruction *** the swelling is interfering with swallowing, causing dehydration and marked systemic upset ** they have a history of sleep apnoea, daytime somnolence or failure to thrive * they have had 5 or more episodes of acute sore throat in the preceding 12 months documented by the parent or doctor, and which have been severe enough to disrupt the child’s normal behaviour or day-to-day activity * they have guttate psoriasis which is exacerbated by recurrent tonsillitis + there is suspicion of a serious underlying disorder such as leukaemia Key to referral times: **** immediate referral (a) *** urgent referral (b) ** soon (b) * routine (b) + times will be discretionary and depend on clinical circumstances (a) within a day (b) Health authorities, trusts and primary care groups should work to local definitions of maximum waiting times in each of these categories. The multidisciplinary groups considered that a maximum waiting time of 2 weeks is appropriate for the urgent category Other suggested reasons that a patient with a sore throat may be referred include (2): retropharyngeal abscess acute epiglotittis oropharyngeal tumour recurrent tonsillitis blood dyscrasias Differential diagnosis Features suggesting an infective cause for a sore throat include: fever - makes infection the likely cause, although lack of fever does not exclude infection pathology of the oropharynx: o quinsy is a bacterial complication o peritonsillar cellulitis particularly unilateral may have a bacterial aetiology - research evidence would be valuable o palatal petechae occur in glandular fever o Koplik's spots of measles o blisters of herpes simplex, foot and mouth cervical glands: o large cervical glands make a diagnosis of glandular fever more likely o occipital glands point to rubella skin rashes may point to viral or bacterial aetiology A no antibiotic prescribing strategy or a delayed antibiotic prescribing strategy should be agreed for patients with the following conditions: acute otitis media acute sore throat/acute pharyngitis/acute tonsillitis common cold acute rhinosinusitis acute cough/acute bronchitis Depending on clinical assessment of severity, patients in the following subgroups can also be considered for an immediate antibiotic prescribing strategy (in addition to a no antibiotic or a delayed antibiotic prescribing strategy): bilateral acute otitis media in children younger than 2 years acute otitis media in children with otorrhoea acute sore throat/acute pharyngitis/acute tonsillitis when three or more Centor criteria are present For all antibiotic prescribing strategies, patients should be given: advice about the usual natural history of the illness, including the average total length of the illness (before and after seeing the doctor): o acute otitis media: four days o acute sore throat/acute pharyngitis/acute tonsillitis: one week o common cold: one and a half weeks o acute rhinosinusitis: two and a half weeks o acute cough/acute bronchitis: three weeks When the no antibiotic prescribing strategy is adopted, patients should be offered: o reassurance that antibiotics are not needed immediately because they are likely to make little difference to symptoms and may have side effects, for example, diarrhoea, vomiting and rash o a clinical review if the condition worsens or becomes prolonged When the delayed antibiotic prescribing strategy is adopted, patients should be offered: o reassurance that antibiotics are not needed immediately because they are likely to make little difference to symptoms and may have side effects, for example, diarrhoea, vomiting and rash o advice about using the delayed prescription if symptoms are not starting to settle in accordance with the expected course of the illness or if a significant worsening of symptoms occurs o advice about re-consulting if there is a significant worsening of symptoms despite using the delayed prescription. A delayed prescription with instructions can either be given to the patient or left at an agreed location to be collected at a later date For complete details then consult the full guidance (1) Reference: (1) NICE (June 2008).Respiratory tract infections - antibiotic prescribing for self-limiting respiratory tract infections in adults and children in primary care Depending on clinical assessment of severity, patients in the following subgroups can also be considered for an immediate antibiotic prescribing strategy (in addition to a no antibiotic or a delayed antibiotic prescribing strategy): bilateral acute otitis media in children younger than 2 years acute otitis media in children with otorrhoea acute sore throat/acute pharyngitis/acute tonsillitis when three or more Centor criteria are present an immediate antibiotic prescription and/or further appropriate investigation and management should only be offered to patients (both adults and children) in the following situations: if the patient is systemically very unwell if the patient has symptoms and signs suggestive of serious illness and/or complications (particularly pneumonia, mastoiditis, peritonsillar abscess, peritonsillar cellulitis, intraorbital and intracranial complications) if the patient is at high risk of serious complications because of pre-existing comorbidity. This includes patients with significant heart, lung, renal, liver or neuromuscular disease, immunosuppression, cystic fibrosis, and young children who were born prematurely if the patient is older than 65 years with acute cough and two or more of the following criteria, or older than 80 years with acute cough and one or more of the following criteria: hospitalisation in previous year type 1 or type 2 diabetes history of congestive heart failure current use of oral glucocorticoids o For these patients, the no antibiotic prescribing strategy and the delayed antibiotic prescribing strategy should not be considered Acne Patient information leaflet on cause and treatment http://www.patient.co.uk/health/Acne.htm Treatments http://bnf.org/bnf/bnf/current/6043.htm 13.6.1 Topical preparations for acne 13.6.2 Oral preparations for acne Ankle rules http://www.bmj.com/content/339/bmj.b2901.full Chickenpox Patient information leaflet http://www.patient.co.uk/health/Chickenpox-in-Children-Under-12.htm First aid advice http://www.sja.org.uk/sja/first-aid-advice.aspx Hand foot and mouth disease Patient information leaflet http://www.patient.co.uk/health/Hand,-Foot-and-Mouth-Disease.htm Joint examination Guidebook on how to examine joints from Arthritis Research UK http://www.arthritisresearchuk.org/pdf/3231_StudentHandbook_11-1.pdf Meningococcal septicaemia and vaccination http://www.hpa.org.uk/web/HPAweb&HPAwebStandard/HPAweb_C/1296682977081 http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_079917 Oral cancer BMJ article http://www.bmj.com/content/318/7190/1051.full?sid=80c45713-00d7-460b-9fed-214df4445d68 Osgood-Schlatter's disease http://www.cks.nhs.uk/osgood_schlatters_disease/management/scenario_diagnosis#405510006 Red eye A podcast for red eye conditions that are easily treatable in Primary Care http://www.cks.nhs.uk/knowledgeplus/podcasts/red_eye acute anterior uveitis scleritis herpes simplex keratitis thalamic shingles bacterial keratitis acute angle closure glaucoma similar picture emerges due to acute inflammatory process of anterior eye, pain (not grittiness), waterying, redness, photophobia and decrease in vision are red flags. Check visual acuity. If reduced, does it improve with a pinhole? If not = significant red eye problem. Can be treated in the GP practise Bacterial (1-2 days onset, red eyes, discharge worse in mornings, lids sticking together, feeling of grittiness, ?blurring of vision but no marked loss); o/e red but not intense, mucopurulent discharge on conjunctiva, crusting of eyelids, normal acuity, treatment is to bathe the eyes, removing crusts for mild-moderate infections. Aggressive infections: chloramphenicol or fusidic acid. viral (sore, red, watery eye, other eye affected, vision ok with pinhole, partner affected, severity normally mild-mod. More severe may also have subconjunctival haemprhage, partial inflammation, may be swollen preauricular lymph nodes) treat with bathing and cold compress, use separate towels, may take 1 week to develop and 2-3 weeks to resolve, and allergic conjunctivitis (red, itcy, watery eyes, Hx of allergies, both eyes, conjunctiva inflamed to varying degrees, vision blurred normal with pinhole, seasonal allergic conjunctivitis, treatment: bathing and cold compress, topical steroid eye drops? ) Episcleritis: inflamm of the episclera, engorgement of episcleral vessels, young, red, mild discomfort, one eye, acuity normal, self-limiting and resolves in 1-2wks oral NSAIDs if recurrent or some discomfort Subconjunctival haemorrhage: acute, look in the mirror, no symptoms, vision not affected, no obv cause, check BP and warfarin INR, takes 1-2wks to settle down. Trauma: blunt and penetrating injury – pain, reduced vision, disruption of iris – refer urgently to casualty; highvelocity injuries may present a couple of days later, urgent referral Superficial corneal injury – scratch from a nail, red, watering, vision reduced, fluorscein staining, topical ABx to see if settling There is a related podcast dealing with Red Flag conditions in Primary Care Scabies This page includes links to many resources http://www.nhs.uk/conditions/Scabies/Pages/Introduction.aspx Sore throat Information on the Centor criteria http://www.gpnotebook.co.uk/simplepage.cfm?ID=x20061213134544295600 Sprains and strains Clinical advice on assessment and management http://www.cks.nhs.uk/sprains_and_strains Threadworms Patient information leaflet http://www.patient.co.uk/health/Threadworms.htm