Training Reguirements for the specialty of Infectious - UEMS-ID
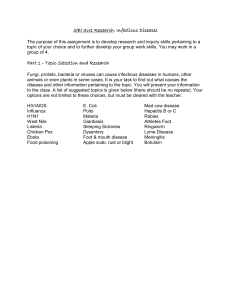
advertisement

UNION EUROPÉENNE DES MÉDECINS SPÉCIALISTES EUROPEAN UNION OF MEDICAL SPECIALISTS Association internationale sans but lucratif AVENUE DE LA COURONNE, 20 BE- 1050 BRUSSELS www.uems.net International non-profit organization T +32 2 649 51 64 F +32 2 640 37 30 info@uems.net Training Requirements for the Specialty of Infectious diseases, European Standards of Postgraduate Medical Specialist Training (old chapter 6) Preamble The UEMS is a non-governmental organization representing national associations of medical specialists at the European Level. With a current membership of 34 national associations and operating through 39 Specialist Sections and European Boards, the UEMS is committed to promote the free movement of medical specialists across Europe while ensuring the highest level of training which will pave the way to the improvement of quality of care for the benefit of all European citizens. The UEMS areas of expertise notably encompass Continuing Medical Education, Post Graduate Training and Quality Assurance. It is the UEMS' conviction that the quality of medical care and expertise is directly linked to the quality of training provided to the medical professionals. Therefore the UEMS committed itself to contribute to the improvement of medical training at the European level through the development of European Standards in the different medical disciplines. No matter where doctors are trained, they should have at least the same core competencies. In 1994, the UEMS adopted its Charter on Post Graduate Training aiming at providing the recommendations at the European level for good medical training. Made up of six chapters, this Charter set the basis for the European approach in the field of Post Graduate Training. With five chapters being common to all specialties, this Charter provided a sixth chapter, known as “Chapter 6”, that each Specialist Section was to complete according to the specific needs of their discipline. More than a decade after the introduction of this Charter, the UEMS Specialist Sections and European Boards have continued working on developing these European Standards in Medical training that reflects modern medical practice and current scientific findings. In doing so, the UEMS Specialist Sections and European Boards did not aimed to supersede the National Authorities' competence in defining the content of postgraduate training in their own State but rather to complement these and ensure that high quality training is provided across Europe. At the European level, the legal mechanism ensuring the free movement of doctors through the recognition of their qualifications was established back in the 1970s by the European Union. Sectorial Directives were adopted and one Directive addressed specifically the issue of medical Training at the European level. However, in 2005, the European Commission proposed to the European Parliament 1 and Council to have a unique legal framework for the recognition of the Professional Qualifications to facilitate and improve the mobility of all workers throughout Europe. This Directive 2005/36/EC established the mechanism of automatic mutual recognition of qualifications for medical doctors according to training requirements within all Member States; this is based on the length of training in the Specialty and the title of qualification. Given the long-standing experience of UEMS Specialist Sections and European Boards on the one hand and the European legal framework enabling Medical Specialists and Trainees to move from one country to another on the other hand, the UEMS is uniquely in position to provide specialty-based recommendations. The UEMS values professional competence as “the habitual and judicious use of communication, knowledge, technical skills, clinical reasoning, emotions, values, and reflection in daily practice for the benefit of the individual and community being served”1. While professional activity is regulated by national law in EU Member States, it is the UEMS understanding that it has to comply with International treaties and UN declarations on Human Rights as well as the WMA International Code of Medical Ethics. This document derives from the previous Chapter 6 of the Training Charter and provides definitions of specialist competencies and procedures as well as how to document and assess them. For the sake of transparency and coherence, it has been renamed as “Training Requirements for the Specialty of Infectious diseases”. This document aims to provide the basic Training Requirements for the specialty and should be regularly updated by UEMS Specialist Section and Boards to reflect scientific and medical progress. The three-part structure of this documents reflects the UEMS approach to have a coherent pragmatic document not only for medical specialists but also for decision-makers at the National and European level interested in knowing more about medical specialist training. 1 Defining and Assessing Professional Competence, Dr Ronald M. Epstein and Dr Edward M. Houndert, Journal of American Medical Association, January 9, 2002, Vol 287 No 2 2 I. TRAINING REQUIREMENTS FOR TRAINEES 1. Content of training and learning outcome Competencies required of the trainee Definition of competency: knowledge, skills and professionalism A medical trainee is a doctor who has completed his/her general professional training as a physician and is in an accredited training program to become a recognized medical specialist. Variably known in different countries as an intern, fellow or registrar. ‘Learning Outcomes’ means statements of what a learner knows, understands and is able to do on completion of a learning process, which are defined in terms of knowledge, skills and competence. Theoretical and practical training will follow an established programme approved by the National Authorities in accordance with national rules and EU/EFTA legislation as well as with UEMS/EMID recommendations. At EU/EFTA levels the UEMS Section and the EBID recommend that general description of Higher Medical Training for Infectious Diseases should have a training programme that will include agreed periods undertaken in the management of unselected community acquired infection(s) and the management of imported infection, both as in patient and out-patient, and hospital acquired infection. Attachment to a Medical Microbiology/Clinical Virology department is also necessary during the training to enable the trainee to acquire the ability to use the laboratory appropriately and to interpret data originating from the Clinical Microbiology laboratory. Involvement in the management of compromised patients (for example HIV infection, transplant patients, patients with infected prostheses) and a period of involvement in an Intensive Care Unit will be obligatory. Research will be regarded as an integral component within the training programme. It is recognised that in some countries infectious diseases is practised with clinical responsibility for patients in a ward and in others it may be more on a consultation basis but the underlying principles included in this training programme should be relevant to both styles of training. REQUIREMENTS for TRAINEES 1. EXPERIENCE To build up his/her experience the trainee should be involved in the management and treatment of a sufficient number of in-patients and out-patients and perform a sufficient number of the practical procedures indicated in section b. It is recognised that this may sometimes require secondment to an additional accredited training department/hospital. 2. LANGUAGE The trainee should have sufficient linguistic ability to communicate with patients and to study international literature and to communicate with foreign colleagues. In some countries this may be subject to a formal test. 3 3. RESPONSIBILITY The trainee has the responsibility to keep his/her log book up to date in accordance with national guidelines and EC Directives. a. Theoretical knowledge Should include the main domains covered by the specialty with a short description of domains that trainee should master in the specialty Theoretical and practical training will follow an established programme approved by the National Authorities in accordance with national rules and EU/EFTA legislation as well as with UEMS/EMID recommendations. At EU/EFTA levels the UEMS Section and the EBID recommend that: b. Practical and clinical skills Key skills to possess in this specialty Number of procedures required Practical Skills to be acquired by completion of infectious diseases training: The underlying objective is to produce an individual who can function independently at consultant/specialist level by the end of training. Requirements can be summarised as follows: i. Appropriate management of an emergency admission suffering from severe infection. ii. Competence in acute assessment of patients suffering from infections and the day-to-day care of patients suffering from severe infections and its sequelae. iii. Management of severe infection in an ICU setting. iv. Management of patients with imported infections - e.g. malaria. v. Care of compromised patients - including neutropenic and those with HIV infection/AIDS. It is essential that the trainee must develop the skill to effectively use and monitor combination antiviral regimes. vi. Management of nosocomial infections, with knowledge of infection control, and appropriate liaison with laboratory services. vii. Practical knowledge of common clinical diagnostic procedures. It is also essential that the trainee be: a. Regularly involved in under-graduate and post-graduate teaching. b. Involved in audit and quality control relating to the speciality. c. Conversant with clinical pharmacological aspects of and appropriate use of antimicrobial chemotherapy (where possible with involvement with the Antibiotic Sub-Committee). d. Conversant with aspects of infection control (where possible by being co-opted onto the Infection Control Committee). e. Aware of resource management implications related to practice in the speciality. f. Able to lead a multidisciplinary team in the clinical setting. 4 By completion of infectious disease training the trainee must: 1. Be competent to supervise work and training of staff undergoing general professional training (common trunk general internal medicine), and to contribute to the training of those in the earlier stages of infectious diseases training. 2. Have understanding of clinical and/or laboratory research methods. 3. Have been exposed to ‘management’. This should include attendance at agreed courses and committee experience. 4. Be familiar with administrative duties relevant to modern consultant practice in the specialty. 5. Be aware of the importance of involvement in continuing medical education (CME) and utilisation of resources for this purpose. Joint Training with General Internal Medicine: This may be undertaken and will have to be in accordance with guidelines produced by the National Authorities to meet European requirements. Joint Training with Microbiology: This may be undertaken and will have to be in accordance with guidelines produced by the National Authorities to meet European requirements c. Competences Description of levels of competencies The European Specialist Curriculum must cover not only knowledge and skills, but also domains of professionalism, as detailed by the UEMS Section. Infectious Diseases includes both community Acquired Infection and hospital acquired infection: Involvement in management (clinical assessment, investigation, diagnosis, treatment and follow up) of patients suffering from unselected infections, preferably predominantly community acquired, and imported infection(s) forms a central theme within the training programme. Consult experience should be obtained during this period e.g. in other hospital-associated infections such as surgical infections, orthopaedic infection, device related infections and infection in immune compromised patients. At least 2 years should usually be spent in an approved post which meet the above requirements of the curriculum. It must include both inpatient and outpatient care. (A maximum of one year of training outside the European Community at a recognised training centre approved prior to the period of training by the specialist national authority will be acceptable). 1. HIV/AIDS: Experience in HIV/AIDS must form part of the training programme and may require rotation to a unit possessing a high component of suitable patients or to a dedicated HIV unit if it cannot be provided in the primary ID training centre. 5 2. Tuberculosis and viral hepatitis: Experience in the management tuberculosis and viral hepatitis (including B and C) must be part of the training programme. 3. Compromised Patients: The training programme must include experience in the management of opportunistic infection(s) in immunocompromised patients such as neutropenic hosts, transplant patients, congenital immune deficiencies as well as those compromised by illness such as diabetes mellitus and infected prosthetic devices. 4. Travel medicine and migrant health: The training must include aspects of prevention of travel associated diseases as well as the regular clinical assessment, diagnosis and management of travel related infections and migrant health. If this training cannot be provided at the primary training centre, the experience must be obtained elsewhere. 5. Intensive Care: A period of attachment to or a period providing consults to an Intensive Care Unit to gain experience in the management of these patients must form part of the training programme. A period spent in this environment should provide additional experience in the prevention and treatment of nosocomial infection and sepsis. 6. Medical Microbiology: Experience in Medical Microbiology is essential. It is envisaged that attachment, collaborative research, and/or direct involvement in these disciplines will be necessary. 7. Control of Infection: Experience in the prevention and control of community and healthcare related infections or hospital outbreaks e.g. MRSA, SRSV is important. 8. Epidemiology and Public Health Medicine: A period of interface with these disciplines is regarded as desirable and will enable the trainee to become familiar with the principles and practicalities of immunisation and vaccination, investigation and control of notifiable diseases and community outbreaks. A maximum combined period of 3 months in these disciplines would be acceptable. 9. Research: Training to develop a basic understanding and ability in clinical and/or laboratory research methodology is essential. A period of supervised research or further formal postgraduate training, is encouraged. No more than 12 months research will usually be acceptable as counting towards the 4 year training period. 10. Tropical Infectious Diseases: For those training in infectious diseases wishing to enhance their training in tropical infectious diseases the following would be valuable: 6 i. A twelve month period in a recognised training centre in the tropics. (A maximum of one year of training outside the European Community at a recognised training centre approved prior to the period of training by the specialist national authority will be acceptable). ii. Attendance at a tropical medicine training course at one of the internationally approved centres such as those leading to the Diploma in Tropical Medicine and Hygiene or equivalent. iii. Experience in a parasitological laboratory. 11. Bioterrorism An understanding of the issues related to the clinical presentation, early recognition, epidemiology and management and control of infections which could potentially be deliberately released into a community for example, smallpox, anthrax, plague, botulism and tularaemia. 12. Sexually Transmitted Diseases An understanding of the basic principles of STD as they relate to infectious diseases is desirable. 13. Antimicrobial Chemotherapy A knowledge of the issues relating to optimal use of antimicrobial chemotherapy including an understanding of the pharmacokinetics and principles of prevention, mechanisms of resistance and management of antimicrobial resistance must be obtained during the training. 2. Organisation of training GENERAL ASPECTS of INFECTIOUS DISEASES TRAINING In addition to providing specific training for the Infectious Diseases specialist, the training in Infectious Diseases provides a generic programme for specialists who may practice in a variety of infection related disciplines for example tropical medicine, HIV medicine, infection control and aspects of public health medicine SELECTION for and ACCESS to the TRAINING Teachers and training institutions or other responsible bodies select and appoint trainees in accordance with the established selection procedure. This selection must be in open competition and on an equal opportunity basis. a. Schedule of training Minimum duration of training Include required timing 2.1. DURATION of TRAINING A minimum of 6 years postgraduate training is required, of which at least a minimum of 2 years must be in General Internal Medicine which forms the “common trunk” which should 7 be completed before embarking on the specialist training (this 2 year period is subsequent to the compulsory post qualification training internship). 2.2. STRUCTURE of TRAINING - General Internal Medicine - 2 years minimum ‘common trunk’ - as per UEMS description of training programme. - Speciality training 4 years - Infectious Diseases (with tropical medicine as required). 2.3. TRAINING PROGRAMME, TRAINING LOG-BOOK Theoretical and practical training will follow an established programme approved by the National Authorities in accordance with national rules and EU/EFTA legislation as well as with UEMS/EMID recommendations. b. Curriculum of training See section 1c “Competences” above c. Assessment and evaluation Definition of assessment, description of formative and summative assessments, Assessment: Process by which information is obtained relative to some known objective or goal. (a broad term that includes testing) Evaluation: Inherent in the idea of evaluation is "value." Process designed to provide information that will help us make a judgment about a given situation Validated systems of assessment should be used throughout the period of training (for example multisource feedback, directly observed procedures and mini CEX and review of these should form part of the annual review of the trainee. d. Governance 1. MONITORING AUTHORITY The European Board of Infectious Diseases (EBID) is composed of representatives of the European Union of Medical Specialities (UEMS) Specialist Section of Infectious Diseases. The EBID was instituted by the UEMS Specialist Section of Infectious Diseases in London on 11 September 1998. At national level the training in infectious diseases is regulated by National Authorities which set standards in accordance with national rules and European Union/European Free Trade Association (EU/EFTA) legislation as well as in accordance with the recommendation of the UEMS/European Board of Infectious Diseases. 2. RECOGNITION of TEACHERS and TRAINING INSTITUTIONS The National Authorities are responsible for selecting and approving training institutions and teachers at national levels in accordance with national rules and EU/EFTA legislation as well 8 as in accordance with UEMS/EBID recommendations. A system of accreditation of European training centres at EU/EFTA level by the EBID has not been established for infectious diseases (2008). 3 and 4. QUALITY ASSURANCE The National Authorities are responsible for setting up at national level a programme for quality assurance of training and of teachers and training institutions in accordance with national rules and EU/EFTA legislation as well as in accordance with UEMS/EBID recommendations. 5. MANPOWER PLANNING The National Authorities in co-operation with national professional and/or scientific organisations in Infectious Diseases are responsible for developing a manpower planning policy at national level which aims at balancing demand and training for infectious diseases physicians in the EU/EFTA member state concerned. The National Authority should lead manpower planning in individual member countries with the help of EBID as required. 9 II. TRAINING REQUIREMENTS FOR TRAINERS 1. Process for recognition as trainer a. Requested qualification and experience 1. QUALIFICATION of the TEACHERS The chief of training in any training institution must be a recognised specialist in Infectious Diseases and have been practising in the speciality for at least 5 years after specialist accreditation. The teachers and staff must have expertise covering a broad range of infectious diseases practice. 2. TRAINING PROGRAMME Infectious diseases training for any individual trainee must be co-ordinated by an individual person or body. There should be a training programme with a regular formal review for the trainee on a minimum of an annual basis. 3. TEACHER/TRAINEE RATIO The ratio between the number of qualified Infectious Diseases physicians in the teaching staff and the number of trainees should provide for adequate close personal monitoring of the trainee during his/her training and provide adequate exposure of the trainee to the training. This ratio should be no less than 1:1. The trainee should, at each stage of training, have a nominated educational supervisor responsible for overseeing the training and writing a report on progress to inform the annual review. b. Core competencies for trainers Special Qualifications of the trainers when required (if not covered by EU Directive on Professional Qualifications) 2. Quality management for trainers 10 III. TRAINING REQUIREMENTS FOR TRAINING INSTITUTIONS (if not covered by EU Directive on Professional Qualifications) 1. Process for recognition as training center Training institutions will be inspected and approved by national authorities. At EU/EFTA level they may be recognised as a European training centre for Infectious Diseases by the EBID. a. Requirement on staff and clinical activities Minimal number of patients cared for as inpatients and as out patients Range of clinical specialties Composition and availability of faculty, training programme defined, guidelines applies Trainee / trainer ratio Minimal scientific activity 1. SIZE of the TRAINING INSTITUTIONS The main training institution must be of sufficient size to offer the trainee practice and full range of experience of infectious diseases. Training in smaller centres will require rotations to ensure broad clinical experience. Some centres may not be able to provide experience in certain specific areas of training such as HIV, tuberculosis, hepatitis, travel medicine/tropical infectious diseases, and a period of attachment to another department will be required to ensure competencies in these areas are obtained. It is recognised that in some member countries the infectious diseases service is mainly consultation based whereas in others it is holistic with full responsibility for in-patient as well as out-patient care. The training centre must be able to provide active involvement on a daily basis in clinical assessment, investigation, diagnosis and management of in-patients and out-patients (for follow up and new patients) for at least 2 years of the training period. Training institutions must have two or more specialists in Infectious Diseases providing the trainee with an opportunity to work with different trainers. Allied specialities should be present within the institution to enable the trainee to gain experience in the multidisciplinary approach to patient care. b. Requirement on equipment, accommodation Medical-technical equipment, library, opportunities for R&D 2. Quality Management within Training institutions Accreditation Clinical Governance Manpower planning 11 Regular report External auditing Transparency of training programmes Structure for coordination of training Framework of approval – how are they approved QUALITY ASSURANCE of the TRAINING INSTITUTION The training must take place in settings which offer a high quality service. The training institution should have an internal system of medical audit or quality assurance. The training centre should have established ethical committees and pharmaceutical and therapeutics committees. Inspection visits of training institutions by the National Authorities should be conducted on a regular and structured manner. TEACHING INFRASTRUCTURE of the TRAINING INSTITUTION The trainee should have protected time and opportunity for research, practical and theoretical study. There should be opportunity to attend clinical and research courses as appropriate to their training. Access to adequate national and international professional literature should be provided as well as space and equipment for practical training, research and other clinical skills. 12