Sarah_Holmes_AAC_SDA Presentation
advertisement

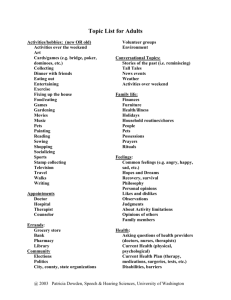
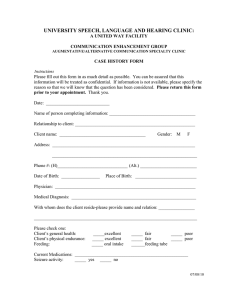
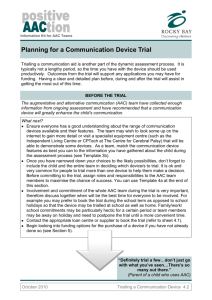
Sarah Holmes RERC on Telerehabilitation holmes.sarah79@gmail.com UPMC Center for Assistive Technology University of Pittsburgh Remote Evaluation and AAC Use: A Case Study Background Augmentative and Alternative Communication (AAC) for adults with cognitivecommunication disorders has expanded rapidly with the influx of high-tech devices that has occurred in recent years, and acceptance and use for adults with traumatic brain injury (TBI) has increased accordingly (Baxter, Enderby, Evans and Judge, 2012a; Beukelman, Fager, Ball and Dietz, 2007). While these communication devices can be highly beneficial resources, the American Speech-Language-Hearing Association (ASHA)’s 2004 AAC Technical Report provides clinicians with an important reminder: An AAC program neither begins nor terminates with the prescription of a communication aid. Instead it involves an ongoing program of decision-making that considers individuals, their methods of communicating, and the effectiveness of that communication with a variety of listeners, as well as environmental variables that foster or impede communication. Methods The client is a 40-year-old female with a bachelor’s degree in Equestrian Science with a minor in English, who also completed several courses in a Master’s in Business Administration program. Her educational career came to an abrupt halt, however, when she sustained a closed head injury in October 1995. Despite persistent weakness on her right side, she has also been able to return to her first love, horseback riding. Her speech is also significantly impaired, with features characteristic of severe flaccid dysarthria. These include breathiness, short phrases, imprecise consonants, hoarse vocal quality, monopitch and monoloudness. Her speech intelligibility is less than 50%; communication via spoken output is belabored and typically requires numerous requests for repetition from communication partners. Device selection for this client was completed via telepractice by an SLP specializing in augmentative communication technology with an on-site graduate clinician acting as a remote assistant. The remote assistant traveled to the client’s home in rural Pennsylvania (three hours from the clinic) and set up a videoconference using a laptop, orbital camera, and a camera positioned over the client’s shoulder on a tripod, which allowed for viewing of the communication device screen. The Versatile and Integrated System for Telerehabilitation, also known as VISYTER (Parmanto, Pramana, Schein and McCue, 2010), was the interface used for teleconferencing. This system allowed the SLP to view and record audio and video from the three cameras on site and his own camera simultaneously, and provided an interface through which he could communicate with the client and remote assistant online. Results Follow-up assessments were administered in the form of the Proficiency Probe for Competence Levels of AAC Users, or PPC (Jinks, 2010), and the Psychosocial Impact of Assistive Devices Scale (PIADS) three months after device acquisition, and again at the nine month mark. In this time, the client became proficient at an expert level in social, linguistic, operational, and strategic competence, showing increases in all realms of proficiency on her PPC scores (data table to be included). One expert-level skill demonstrated by this user was page creation, which required creation, naming, and formatting (choosing font size, appropriate icons for each button, etc.) of new buttons. Pages were for categories such as “horse breeds,” “family,” “medical,” “feelings,” and “jokes,” along with a number of others. The client also uses her device for peripheral purposes, such as email, which she uses regularly to send detailed and lengthy updates to her physicians and therapists. Moreover, she expanded her use of the device by employing it to produce a thank-you speech for volunteers from her non-profit therapeutic horseback riding organization. Based on scores reported by this client on the PIADS, which was administered nine months after device acquisition, she experienced significant changes in her happiness, independence, self-esteem, productivity, self-confidence and quality of life. Furthermore, regarding feeling more “in charge,” she responded that, “I think for years I have depended on my Mom to do things for me. Now, I can, and do, speak for myself.” These findings are consistent with others who found that AAC use increased feelings of overall self-worth and independence in highly motivated users (Dattilo, Estrella, Estrella, Light, McNaughton and Seabury, 2008; Lund and Light, 2006). By providing telerehabilitation services through an SLP-AAC specialist and a remote assistant, a high-tech speech-generating device was obtained for this client. With ongoing training and follow-up assessments, significant progress in user proficiency and quality of life were documented. After nine months, the client had created numerous pages for speech output, used email and a drawing application regularly, and had used the device to give a speech in front of a large audience. Her success with the Nova Chat7 increased her self-esteem, happiness, and overall quality of life, and has motivated her to become more independent. This client’s success is attributable to her high level of motivation and willingness to incorporate the device into her daily life. These intrinsic factors are notable in that they may predict the likelihood of success for other users of high-tech AAC devices. Future studies should assess the role of motivation and personality in the generalization and maintenance of skills related to AAC device use in order to gain a more complete understanding of why certain users are more successful than others. References American Speech-Language-Hearing Association. (2004). Roles and responsibilities of speechlanguage pathologists with respect to augmentative and alternative communication: technical report [Technical Report]. Retrieved from www.asha.org/policy. Baxter, S., Enderby, P., Evans, P., & Judge, S. (2012a) Barriers and facilitators to the use of high-technology augmentative and alternative communication devices: a systematic review and qualitative synthesis. International Journal of Language and Communication Disorders, 47 (2), 115-129. Baxter, S. Enderby, P., Evans, P., Judge, S. (2012b). Interventions using high-technology communication devices: A state of the art review. Folia Phoniatrica et Logopaedica, 64, 137-144. Beukelman, D. R., Fager, S., Ball, L., & Dietz, A. (2007). AAC for adults with acquired neurological conditions: A review. Augmentative and Alternative Communication, 23(3), 230-242. Dattilo, J., Estrella, G., Estrella, L. J., Light, J., McNaughton, D., & Seabury, M. (2008). “I have chosen to live life abundantly”: Perceptions of leisure by adults who use augmentative and alternative communication. Augmentative and Alternative Communication, 24(1), 1628. Jinks, A. (2010). Proficiency Probe for Competence Levels of AAC Users (unpublished paper). Lund, S. K., & Light, J. (2006). Long-term outcomes for individuals who use augmentative and alternative communication: Part I-What is a “good” outcome?. Augmentative and Alternative Communication, 22(4), 284-299. Parmanto, B., Saptono, A., Pramana, G., Pulantara, W., Schein, R. M., Schmeler, M. R., McCue, M. P. & Brienza, D. M. (2010). VISYTER: Versatile and integrated system for telerehabilitation. Telemedicine and e-Health, 16(9), 939-944. Ward, E.C., Sharma, S., Burns, C., Theodoros, D., & Russell, T. (2012). Managing patient factors in the assessment of swallowing via telerehabilitation. International Journal of Telemedicine and Applications, 2012, 1-6.