biochem ch 45 [9-2
advertisement

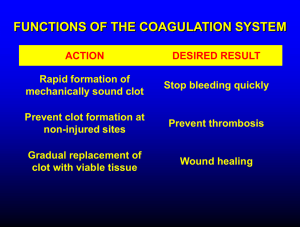
Blood Plasma Proteins, Coagulation, and Fibrinolysis Osmotic pressure exerted by plasma proteins regulates distribution of water between blood and tissues Plasma proteins in junction with platelets maintain integrity of circulatory system through clotting Primary hemostatic plug consists of aggregated platelets and a fibrin clot o Platelets attached to subendothelial layer of vessel principally thorough von Willebrand factor and are activated to bind fibrinogen o Fibrinogen binds platelets to each other to form platelet aggregate, which is rapidly covered with layers of fibrin, which are formed from fibrinogen by the proteolytic enzyme thrombin o Injury to endothelium and exposure of tissue factor on subendothelial layer to plasma proteins also activate blood coagulation cascade o Factor XIII cross-links strands of of polymerized fibrin monomers to form secondary hemostatic plug o Ca2+ and γ-carboxyglutamate residues in proteins (formed by vitamin K-dependent process in liver) attach factor complexes to phospholipids exposed on platelet membranes, causing thrombus formation to be rapidly accelerated and localized to site of injury Regulatory mechanisms within blood coagulation cascade and antifibrinolytic mechanisms prevent random coagulation within blood vessels that might obstruct blood flow; impairments here lead to thrombosis Plasma Proteins Maintain Proper Distribution of Water between Blood and Tissues 2 basic assays for measuring activity of factor VIII in blood sample o Functional (clotting) assay – sample of patient’s plasma added to factor VIII-deficient sample of plasma, and time to generate clot formation determined; clot formation is end product of the assay, but you are measuring eventual activation of factor II to IIa, which allows clot formation to initiate o Coupled (to factor X activation) enzyme system leading to cleavage of chromogenic substrate, generating colored product – chromogenic assay or automated assay – sample of unknown is mixed with purified factor IXa, Ca2+, phospholipid vesicles, chromogenic substrate, and purified factor X; if unknown sample contains factor VIII, factors VIII and IXa will synergize and activate factor X to Xa, which will cleave chromogenic substrate, forming a colored product, whose concentration can be determined spectrophotometrically; comparison to standard curve of factor VIII addition enables accurate estimate of level of active factor VIII in sample In cases of severe protein malnutrition (kwashiorkor), concentration of plasma proteins decreases as result of which osmotic pressure of blood decreases; as result, fluid not drawn back to blood and accumulates in interstitial space (edema); distended bellies of famine victims result of fluid accumulation in extravascular tissues because of severely decreased concentration of plasma proteins, particularly albumin; albumin synthesis decreases fairly early under conditions of protein malnutrition Plasma contains water, nutrients, metabolites, hormones, electrolytes, and proteins; essentially same electrolyte composition as other extracellular fluids and constitutes about 25% of body’s total extracellular fluid o Plasma proteins maintain proper distribution of water between blood and tissues, transport nutrients, metabolites, and hormones throughout body, defend against infection, and maintain integrity of circulation through clotting As arterial blood enters capillaries, fluid moves from intravascular space into interstitial space because of Starling forces (hydrostatic pressure in arteriolar end of capillaries exceeds sum of tissue pressure and osmotic pressure of plasma proteins), so water tends to leave capillaries and enter extravascular spaces At venous end of capillaries, hydrostatic pressure falls while osmotic pressure and tissue pressure remain constant, resulting in movement of fluid back from extravascular (interstitial) spaces and into blood o Most of force bringing water back from tissues into plasma is osmotic pressure mediated by presence of proteins in plasma Albumin constitutes about 60% of total plasma protein but contributes 70-80% of total osmotic pressure of plasma; albumin is glycoprotein carrier of free fatty acids, calcium, zinc, steroid hormones, copper, and bilirubin o Many drugs bind to albumin (drug does may need to be recalculated if patient’s plasma protein concentration is abnormal) o Individuals who lack albumin have only moderate edema because concentration of other plasma proteins increased to compensate for lack of albumin; rare to have no albumin Plasma Contains Proteins that Aid in Immune Defense Two different types of proteins aid in immune response: immunoglobulins and complement proteins o Immunoglobulins secreted by plasma cells and bind antigens at binding sites formed by hypervariable regions of proteins; once antibody-antigen complex formed, it must be cleared from circulation Complement system proteins become activated by interaction with antigen-antibody complexes or (specific to bacterial infections) through interaction of bacterial cell polysaccharides with complement protein C3b o Activation of complement system results in proteolytic activation cascade of proteins of complement system, resulting in release of biologically active peptides or polypeptide fragments that mediate the inflammatory response, attract phagocytic cells to the area, initiate degranulation of granulocytes, and promote clearance of antigen-antibody complexes Protease inhibitors in plasma serve to control inflammatory response o Activated neutrophils release lysosomal proteases from granules that attack elastin, various types of collagen, and other ECM proteins o Plasma proteins α1-antiproteinase (α1-antitrypsin) and α2-macroglobulin limit proteolytic damage by forming noncovalent complexes with proteases, thereby inactivating them o Product of neutrophil myeloperoxidase (HOCl) inactivates protease inhibitors, ensuring proteases are active at site of infection α1-antiproteinase (AAP) is main serine protease inhibitor of plasma; individeuals with point mutation in exon 5 of AAP gene, which results in single AA substitution in protein, have diminished secretion of AAP from liver and are at increased risk for developing emphysema o When neutrophils degranulate in lungs as part of body’s defense against microorganisms, insufficient levels of AAP present to neutralize elastase and other proteases released o Excess proteolytic activity damages lung tissue, leading to loss of alveolar elasticity and emphysema o Methionine 358 of AAP necessary for AAP binding to proteases; oxidation of this methionine destroys AAP’s protease-binding capacity; cigarette smoke oxidizes Met-358, increasing risk of emphysema Plasma Proteins Maintain Integrity of Circulatory System When blood vessel wall damaged, subendothelial cell layer exposed, consisting of basement membrane of endothelial cells and smooth muscle cells In response to above damage, barrier (hemostatic plug, fibrin clot) initiated by platelet binding to damaged area Regulatory mechanisms limit clot formation to site of injury and control size and stability As vessel heals, clot is degraded (fibrinolysis) Plasma proteins required for above to occur Idiopathic thrombocytopenic purpura (ITP) – autoimmune disease in which antibodies to platelet glycoproteins produced; antibody binding to platelets results in clearance bhy spleen o Early symptom is appearance of small red spots on skin (petechial hemorrhages) caused by blood leakage from capillaries o Minor damage to vascular endothelial cells constantly being caused by mechanical forces related to blood flow o Patients have few platelets available to repair damage Formation of Hemostatic Plug Platelets major role is to form mechanical plugs at site of vessel injury and secrete regulators of clotting process and vascular repair; in absence of platelets, leakage of blood from rents in small vessels common o Derived from megakaryocytes in bone marrow o Megakaryocytes differentiate from hematopoietic stem cell; as megakaryote matures, it undergoes synchronous nuclear replication without cellular division to form cell with multilobed nucleus and enlarged cytoplasm; at 8 nucleus stage, cytoplasm becomes granular and platelets budded off cytoplasm; single megakaryote gives rise to about 4,000 platelets In nonactivated platelet, PM invaginates extensively into interior of cell, forming open membrane (canalicular) system; because PM contains receptors and phospholipids that accelerate clotting process, canalicular structure substantially increases membrane SA that is potentially available for clotting reactions Platelet interior contains microfilaments and extensive actin/myosin system – platelet activation in response to endothelial injury causes Ca2+-dependent changes in contractile elements, which substantially change architecture of PM; long pseudopodia generated, increasing SA of membrane as clot formation initiated Platelets contain 3 types of granules: electron-dense granules (contain Ca, ADP, ATP, and serotonin), α-granules (contain heparin antagonist, platelet-derived growth factor, β-thromboglobulin, fibrinogen, von Willebrand factor, and other clotting factors), and lysosomal granule (contains hydrolytic enzymes) o During activation, contents of granules secreted and modulate platelet aggregation and clotting vWF – large multimeric glycoprotein; role is to stabilize factor VIII and protect it from degradation o High-molecular-weight (HMW) forms concentrated in endothelium of blood vessels and released in response to stress hormones and endothelial damage o HMW vWF released by endothelium and cleaved by specific metalloprotease in serum, reducing size of circulating vWF o Large vWF multimers more effective at forming complexes with platelets than are small vWF multimers o vWF deficiency most common cause of inherited bleeding disorders; both platelet adherence and clotting cascade affected because levels of factor VIII low In absence of vWF, factor VIII rapidly cleared from system Multiple mutations of vWF gene known with varying clinical presentations 3 fundamental mechanisms involved in platelet function during blood coagulation: adhesion (sets off series of reactions called platelet activation, which leads to adhesion and secretion of platelet granule contents), aggregation, and secretion o Adhesion step is primarily platelet-subendothelial interaction that occurs when platelets initially adhere to sites of blood vessel injury Blood vessel injury exposes collagen, subendothelial matrix-bound vWF, and other matrix components vWF synthesized in endothelial cells and megakaryocytes and is located in subendothelial matrix, in specific platelet granules, and in circulation bound to factor VIII Platelet PM contains glycoproteins (Gps) that bind to collagen and vWF, causing platelet to adhere to subendothelium; binding to collagen by GpIa (integrin α2β1) causes platelet to change shape from flat disc to spherical cell, extruding long pseudopods that promote platelet/platelet interactions Binding of subendothelial vWF by GpIb causes changes in platelet membrane that expose GpIIbIIIa (integrin αIIbβ3)-binding sites to fibrinogen and vWF o Initial adherence of platelets sets off series of reactions (platelet activation) that result in more platelets being recruited and aggregated at site of injury Some platelets release contents of dense granules and α-granules, with ADP release (ADP is potent platelet activator) ADP released from platelets and from damaged RBCs binds to receptor on platelet PM, which leads to further unmasking of GpIIb-IIIa-binding sites Aggregation of platelets cannot take place without ADP stimulation because ADP induces swelling of activated platelets, promoting platelet/platelet contact and adherence o Fibrinogen – protein that circulates in blood and also found in platelet granules that consists of 2 triple helices held together with disulfide bonds Binding of fibrinogen to activated platelets necessary for aggregation, in part providing mechanism by which platelets adhere to one another Cleavage of fibrinogen by thrombin (protease activated by coagulation cascade) produces fibrin monomers that polymerize and form soft clot with platelets o Thrombin – potent activator of platelets through binding to specific receptor on platelet surface Bernard-Soulier syndrome – bleeding disorder caused by defects in GpIb; platelet aggregation affected because of inability of GpIb to adhere to subendothelial vWF Thrombotic thrombocytopenic purpura (TTP) – disease characterized by formation in circulation of microclots (microthrombi) consisting of aggregated platelets; microthrombi collect in microvasculature and damage RBCs, resulting in hemolytic anemia; microthrombi also damage vascular endothelium, exposing collagen and releasing HMW vWF promoting more platelet aggregation o Subsequent depletion of platelets renders patient susceptible to internal hemorrhage o Familial TTP associated with mutations in vWF-specific metalloprotease, although not all individuals with defective protease develop TTP o Sporadic cases of TTP associated with development of antibody to metalloprotease Thrombus formation enhanced by thrombin activation (mediated by complex blood coagulation cascade) o Cascade consists primarily of proteins that serve as enzymes or cofactors, which function to accelerate thrombin formation and localize it at site of injury o All proteins present in plasma as proproteins (zymogens), which are activated by cleavage of polypeptide chain at one or more sites o Key to successful and appropriate thrombus formation is regulation of proteases that activate zymogens Proenzymes (factors VII, IX, X, XI, and prothrombin) are serine proteases that, when activated by cleavage, cleave next proenzymes in cascade o Because of sequential activation, great acceleration and amplification of response achieved o Cleavage and activation occurrence indicated by addition of “a” to name of proenzymes Cofactor proteins (tissue factor, factor V, and factor VIII) serve as binding sites of other factors o Tissue factor – not related structurally to other blood coagulation cofactors and is integral membrane protein that does not require cleavage for active function o Factors V and VIII serve as procofactors that are activated by cleavage to function as binding sites for other factors Protein S and protein C – regulatory proteins that are part of blood coagulation cascade o Protein C regulated by proteolytic cleavage and, when activated, is serine protease In response to collagen and thrombin, platelets release vasoconstrictors o Serotonin released from dense granules of platelets and synthesis of thromboxane A2 stimulated, reducing blood flow to damaged area o Platelet-derived growth factor (stimulates proliferation of vascular cells) released into damaged area Process of Blood Coagulation Activation of blood coagulation cascade triggered by reaction of plasma proteins with subendothelium at same time that platelets are adhering to subendothelial layer 2 different pathways – both require access to PM and calcium (platelet membrane that adhered to damaged site used as scaffold for activation reactions to occur o Extrinsic pathway – dependent on external stimuli such as blunt trauma Damaged tissues present tissue factor to blood at injured site, triggering extrinsic phase of blood coagulation Circulating factor VII binds to tissue factor, which autocatalyzes itself to factor VIIa, which then activates factor X in extrinsic pathway and factor IX in intrinsic pathway o Intrinsic pathway – dependent on internal stimuli Factor IXa activates factor X (hemophilia B is X-linked bleeding disorder caused by mutations in gene for factor IX; lack of factor IX activity leads to inability to convert prothrombin to thrombin and impaired clotting) Sustains coagulation response initiated by extrinsic pathway γ-carboxylated clotting proteins chelated to membrane surfaces via electrostatic interactions with calcium and negatively charged phospholipids of platelet membrane o Protein cofactors VIIIa and Va serve as sites for assembling enzyme-cofactor complexes on platelet surface, thereby accelerating and localizing reaction, resulting in thrombin formation, which augments its own formation by converting factors V, VIII, and XI into activated cofactors and stimulating platelet degranulation o Initial activation of prothrombin slow because activator cofactors VIIIa and Va present in only small amounts, but once small amount of thrombin activated, it accelerates its own production by cleaving factors V and VIII to their active forms (intrinsic pathway) Major substrate of thrombin is fibrinogen (hydrolyzed to form fibrin monomers that undergo spontaneous polymerization to form fibrin clot) – soft clot because fibrin monomers not cross-linked (cross-linking requires factor XIIIa, which is activated by thrombin cleavage of factor XIII) Use of active-site serine to cleave peptide bond common to variety of enzymes referred to as serine proteases o Serine proteases essential for activating formation of blood clot from fibrin o Thrombin – serine protease that converts fibrinogen to fibrin; also cleaves aspartate-histidine-serine catalytic triad found in chymotrypsin and trypsin Activated by proteolytic cleavage of its precursor protein (prothrombin) Sequence of proteolytic cleavages leading to thrombin activation requires factor VIII, blood clotting protein that can be deficient in those with hemophilia A Factor XIIIa catalyzes transamidation reaction between glutamine and lysine side chains on adjacent fibrin monomers – covalent cross-linking takes place in 3D, creating strong network of fibers that are resistant to mechanical and proteolytic damage o Network of fibrin fibers traps aggregated platelets and other cells, forming clot that plugs vent in vascular wall o Factor XIIIa is only enzyme in blood coagulation cascade that is not a serine protease In several essential steps in blood coagulation cascade, activated protease bound in complex attached to surfaces of platelets that have aggregated at site of injury o Factors VII, IX, X, and prothrombin contain domain in which one or more glutamate residues are carboxylated to γ-carboxyglutamate residues that bind Ca2+, which forms a coordination complex with negatively charged platelet membrane phospholipids and γ-carboxyglutamates, thereby localizing complex assembly and thrombin formation to platelet surface o Cofactor Va contains binding site for both factor Xa and prothrombin (zymogen substrate of factor Xa) Upon binding to factor Va-platelet complex, prothrombin undergoes conformation change, rendering it more susceptible to enzymatic cleavage Binding of factor Xa to factor Va-prothrombin-platelet complex allows prothrombin-to-thrombin conversion (complex assembly accelerates rate of conversion 10,000-15,000x o Factor VIIIa forms complex on surface of activated platelets and binds factor IXa and its zymogen substrate (factor X) o Tissue factor is integral membrane protein – once exposed by injury, binds factor VIIa and initiates complex formation Complex assembly enhances rate of thrombin formation by as much as several 100,000x, enabling clot to form rapidly enough to preserve hemostasis; also explosive thrombin formation localized to site of vascular injury at which negatively charged phospholipids exposed o Surface-binding sites only exposed at injury site in which cell rupture exposes internal membrane surface Formation of γ-carboxyglutamate residues on blood coagulation factors takes place in hepatocyte before release of protein; in hepatocyte, vitamin K (present in quinone form) reduced to form vitamin KH2 by microsomal quinone reductase o Vitamin KH2 is cofactor for carboxylases that add carboxyl group to appropriate glutamate residues in proenzymes to form carboxylated proenzyme o To recover active vitamin KH2, vitamin K reduced to quinone form by vitamin K epoxide reductase and then to active hydroquinone form Warfarin (Coumadin) – slow-acting, long-acting blood anticoagulant with structure resembling that of vitamin K, allowing it to compete with vitamin K and prevent γ-carboxylation of glutamate residues in factors II, VII, IX, X, and proteins C and S; noncarboxylated blood clotting protein precursors increase in both blood and plasma, but unable to promote blood coagulation because they cannot bind calcium and thus cannot bind to their phospholipid membrane sites of activation; used for rat poison Deficiency in amount or functionality of protein C or protein S increases risk of venous thromboembolism; individuals homozygous for mutations do not survive neonatal period unless given replacement therapy Regulation through Feedback Amplification and Inhibition Feedback amplification – processes that accelerate clot formation once formation of clot begins Thrombin – involved in both prothrombic regulation (feedback amplification) and antithrombotic regulation (feedback inhibition) o Prothrombic action – initiated when thrombin stimulates its own formation by activating factors V, VIII, and XI, thereby accelerating rate of clot formation; thrombin promotes clot formation by activating platelet aggregation, stimulating release of factor VIII from vWF and cleaving factor XIII to factor XIIIa o Antithrombotic effects – result from binding to endothelial cell receptor (thrombomodulin), which abolishes clotting function of thrombin and allows thrombin to activate protein C, which has anticoagulant effects Protein C and its cofactor protein S serve to suppress activity of coagulation cascade o After activation, protein C forms complex with protein S, which anchors activated protein C (APC) complex to clot through Ca2+/γ-carboxyglutamate binding to platelet phospholipids o APC destroys active blood coagulation cofactors (factor VIIIa and Va) by proteolytic cleavage, decreasing production of thrombin o APC stimulates endothelial cells to increase secretion of prostaglandin I2 (PGI2), which reduces platelet aggregation In European populations, point mutation in factor V gene (factor V Leiden) causes replacement of an arginine with glutamine in preferred site for cleavage by APC, rendering factor Va Leiden resistant to APC o Heterozygous individuals have 6-8x increased risk of DVT, and homozygotes have 30-140x risk o Factor V Leiden mutation not associated with increased risk of arterial thrombosis (such as MI) except in young women who smoke o In developed world, inherited APC resistance is most prevalent risk factor for familial thrombotic disease Serine protease inhibitors (serpins) – group of inhibitory proteins present in plasma at high concentrations (10% of all plasma proteins); inhibit proteases involved in coagulation and clot dissolution (fibrinolysis) o Each inhibitor possesses reactive site that is ideal substrate for specific serine protease and thus acts as trap for that protease; bound serine protease attacks peptide bond located at critical AA residue within serpin and forms tight enzyme-inhibitor complex o Activity of thrombin controlled by serpin antithrombin III (ATIII); regulation of thrombin important because it affects pathways of both coagulation and fibrinolysis One molecule of ATIII irreversibly inactivates one molecule of thrombin through reaction of arginine residue in ATIII with active-site serine residue of thrombin ATIII-thrombin complex formation markedly enhanced in presence of heparin o Heparin – glycosaminoglycan found in secretory granules of mast cells and in LCT around small vascular beds; binds to lysyl residues on ATIII and dramatically accelerates rate of binding to thrombin because of allosteric alteration in ATIII such that position of critical arginine residue of ATIII more readily available for interaction with thrombin Formation of ATIII-thrombin complex releases heparin molecule so it can be reused and therefore function of heparin is catalytic ATIII-heparin complex can inactivate serine protease factors XIIIa, Xia, IXa, and Xa, but has no effect on factor VIIa or APC o Thrombin attached to a surface (i.e., thrombomodulin on endothelial cell membrane) no longer participating in clot formation and is not readily attacked by ATIII or ATIII-heparin complex Thromboresistance of Vascular Endothelium Endothelial cells of blood vessels provide selectively permeable barrier between circulating blood and tissues; normal endothelial cell lining neither activates coagulation nor supports platelet adhesion (nonthrombogenic surface) – reason for that is endothelial cells highly negatively charged (repels negatively charged platelets), endothelial cells synthesize PGI2 and NO (vasodilators and powerful inhibitors of platelet aggregation) o PGI2 synthesis stimulated by thrombin, epinephrine, and local vascular injury Endothelial cells synthesize 2 cofactors that inhibit action of thrombin, thrombomodulin, and heparan sulfate (GAG similar to heparin that potentiates ATIII but not as efficiently) Inactivation of thrombin accelerated by heparan sulfate present on endothelial cell surface Fibrinolysis Fibrinolysis involves degradation of fibrin in clot by plasmin (serine protease formed from zymogen plasminogen); plasminogen is circulating serum protein with high affinity for fibrin, promoting incorporation of plasminogen in developing clot o Conversion of plasminogen to plasmin by plasminogen activators can occur both in liquid phase of blood and at clot surface, but at clot surface, process is far more efficient APC stimulates release of plasminogen activator (tPA) from tissues and simultaneously inactivates inhibitor of plasminogen activator (PAI-1) Circulating plasmin readily inactivated by binding with α2-antiplasmin (circulating protease inhibitor) o Clot-bound plasmin not readily inactivated by α2-antiplasmin, so plasminogen binding to fibrin facilitates activation to plasmin, protects it from blood serpins, and localizes it on fibrin substrate for subsequent efficient proteolytic attack – allows for dissolution of fibrin in pathologic thrombi or oversized hemostatic plugs and prevents degradation of fibrinogen in circulating blood 2 endogenous plasminogen activators most important – both synthesized in variety of cells o tPA – produced chiefly by vascular endothelial cells; has high binding affinity for fibrin and plays major role in fibrinolysis o Single-chain urokinase (U-PA) synthesized in most cells and tissues and has moderate affinity for fibrin Streptokinase – bacterial exogenous plasminogen activator from β-hemalytic streptococci; not enzyme but allosteric modifier of human plasminogen that allows autocatalytic reaction such that plasmin is formed o Physical stress, hypoxia, and large numbers of LMW organic compounds promote increased synthesis and release of tPA and U-PA from tissues into blood o Balance between release of plasminogen activators, availability of fibrin, and inhibitors of activators and plasmin determine regulation of fibrinolytic response Both streptokinase and tPA approved for treatment in MI because it will lead to clot dissolution, thereby restoring blood flow to heart; although there are more side effects associated with use of streptokinase, it is substantially cheaper than tPA Regulation of Fibrinolysis Antiactivators regulate interaction of plasminogen in blood with plasminogen activators in dynamic equilibrium o Even if minute amounts of plasmin generated (e.g., after release of vascular plasminogen activator after stress), enzyme inactivated by antiplasmin Upon activation of blood coagulation system, fibrin clot formed, which strongly binds tPA and plasminogen from blood and accelerates rate of plasmin activation Clot-bound plasmin protected from inhibitors while attached to fibrin Plasmin inactivated by α2-antiplasmin and α2-macroglobulin after proteolytic dissolution of fibrin and liberation into liquid phase of blood Drugs that Inhibit Blood Coagulation Heparin – binds to and activates ATIII, which leads to thrombin inactivation; ATIII also blocks activity of factors VIIIa, IXa, Xa, and XIa o Unfractionated (HMW) heparin – heterogenous mixture of GAGs; binds to plasma proteins and cell surfaces in addition to prime target (ATIII) Because different individuals synthesize different levels of plasma proteins, use of this form requires constant monitoring of patient to ensure correctdosage given so that spontaneous thrombi do not develop but not so much spontaneous bleeding occurs o Fractionated (LMW) heparin – fragments of HMW heparin o Heparin-induced thrombocytopenia (HIT) – major complication of heparin therapy; excessive blood clotting with reduction in number of circulating platelets Caused by heparin binding to platelet protein (platelet factor 4 or PF4), which induces conformational change in PF4 such that immune system believes complex is foreign, so antibodies developed against heparin-PF4 complex When antibodies bind to platelets, they become activated and thrombi develop Treatment consists of removing heparin and using different form of antithrombotic Warfarin – acts by blocking vitamin K reductase enzymes required to regenerate active vitamin K o Results in reduced γ-carboxylation of factors II, VII, IX, and X o In absence of γ-carboxylation, the factors cannot bind calcium nor form complexes necessary for coagulation cascade to be initiated o Blocks activity of proteins S and C, so both blood clotting and regulation of clotting impaired by warfarin administration Analysis of heparin potentiation factor Xa binding to ATIII showed unique pentasaccharide sequence required – fondaparinux formed so it would specifically enhance ATIII interactions with factor Xa; stimulates binding of ATIII to factor Xa by 300x and is specific for factor Xa inhibition o Does not affect thrombin or platelet activity and is not activating agent of platelets o Does not bind PT4, so HIT is not a complication of this therapy Direct thrombin inhibitors based on hirudin molecules initially discovered in leeches o Hirudin treatment dangerous in that formation of hirudin-thrombin complex is irreversible, and use of drug requires constant monitoring of patient Rational drug design based on hirudin structure (synthetic peptide bivalirudin) synthesized; high binding affinity and specificity for thrombin although effects on thrombin transient, making it safer than hirudin