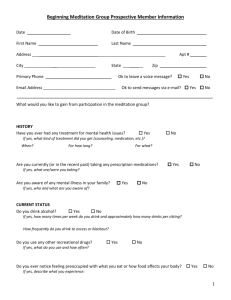
Intake - Zen Life
advertisement

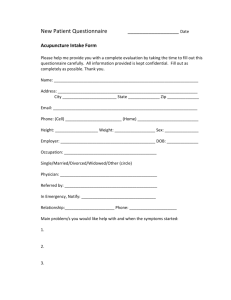
Kristen Barritt, RN L.Ac New Patient Intake Name: _____________________________________________________________________________________________________________ Date of Birth: _____________________ Age: _____________ Sex: ____________ Address: ________________________________________________________ Phone: ___________________________________ Marital Status: __________________ City/State/Zip: _____________________________ Email: ______________________________________________________________ Occupation: ___________________________________________ Employer: ____________________________________________ Emergency Contact (name/relation/phone) __________________________________________________________________ Referred by: _____________________________________________ Physician Name: _________________________________________________ Address:________________________________________________________ Date of last physical exam:_____________ Phone: ____________________________________ City/State/Zip: _____________________________ Date of most recent blood work (attach if possible):___________ Any Western Diagnoses:________________________________________________________________________________________ What would you like to be treated for?__________________________________________________________________________________ __________________________________________________________________________________ __________________________________________________________________________________ Please describe your current medical problem. Please include how and when it began, any treatment you’ve had thus far, any testing (labs, imaging, etc), any relieving or aggravating factors, and any other information you feel would be helpful. ________________________________________________________________________________________________________________________________ _________________________________________________________________________________________________________________________________ _________________________________________________________________________________________________________________________________ _________________________________________________________________________________________________________________________________ _________________________________________________________________________________________________________________________________ _________________________________________________________________________________________________________________________________ _________________________________________________________________________________________________________________________________ Medical History Previous Surgeries/Hospitalizations Reason Date ________________________________________________________________________________________________________________________________ ________________________________________________________________________________________________________________________________ ________________________________________________________________________________________________________________________________ Current Medications (including over the counter) Reason Dosage ________________________________________________________________________________________________________________________________ ________________________________________________________________________________________________________________________________ ________________________________________________________________________________________________________________________________ ________________________________________________________________________________________________________________________________ ________________________________________________________________________________________________________________________________ How many courses of antibiotics have you had in the last 5 years? _____________________________________________________ Current Supplements Reason Dosage ________________________________________________________________________________________________________________________________ ________________________________________________________________________________________________________________________________ ________________________________________________________________________________________________________________________________ Allergies (drugs, seasonal, environmental, etc) ________________________________________________________________________________________________________________________________ ________________________________________________________________________________________________________________________________ ________________________________________________________________________________________________________________________________ Family Medical History Father: Age ____________ Please circle: Good health Poor health Deceased (cause ________________) Mother: Age ____________ Please circle: Good health Poor health Deceased (cause ________________) (Please indicate if you or an immediate family member has/has any of the following conditions) Cancer ______________ Heart disease ______________ High blood pressure _______________ Diabetes ______________ Kidney disease ______________ Bleeding disorders _______________ Epilepsy ______________ Tuberculosis ______________ Alcoholism/Addictions ____________ Arthritis ______________ Mental Illness ______________ Depression/Anxiety _______________ Asthma _______________ Stroke/TIA Osteoporosis _________________ Birth defects _________________ _______________ Alzheimer’s/ Parkinson’s Disease _____________________ Autoimmune disorders (which disorder?) _______________________________________________________________________ Other (please specify) ______________________________________________________________________________________________ Lifestyle History Current Weight: ______________ Do you exercise? Y N Height: ______________ Max Weight: _____________ When? _______________ If yes, what do you do, for how long and how often? _____________________ ______________________________________________________________________________________________________________________ Do you smoke? Y N If yes, how much and for how long? ________________________________________ Previously smoked? Y N If yes, how much and for how long? ________________________________________ Do you drink alcohol? Y N If yes, how much and how often? ___________________________________________ Recreational drug use? Y N Have you been treated for drug/ alcohol addiction? Sleep __________ hours/night Enjoy your work? Y N Y N Easy to get to sleep and stay asleep? Y N Awake rested? Y N Have a good support system? N History of abuse? Y N Y Average stress level (circle): (low) 1 2 3 4 5 6 7 8 9 10 (high) Average energy level (circle): (low) 1 2 3 4 5 6 7 8 9 10 (high) What time of day is your energy highest? ________________________ lowest? ___________________________ What’s your predominant emotion? ____________________________________________________________________________ Circle any that apply: Easily irritated Depressed Worry a lot Cry easily Angry Indecisive Hurry to do things Typical Food Intake Breakfast: _________________________________________________________________________________________________________ Lunch: _____________________________________________________________________________________________________________ Dinner: ____________________________________________________________________________________________________________ Snacks: ____________________________________________________________________________________________________________ Beverages: ________________________________________________________________________________________________________ How much water do you drink in a day? (Iced, room temp, warm, hot?) ___________________________________ Do you eat 3 meals a day? Y N Eat out often? Y N Do you drink coffee/ black tea? Y N If yes, how much? ____________________________ Do you drink soda pop? Y N If yes, how much? ____________________________ Men’s Health (men only please) Please circle below as pertains to you Hernia Testicular masses Testicular pain Penile discharge/sores Sexual difficulties Impaired fertility Are you sexually active? STI/STD’s Y N Y N Prostate problems (Date of last exam? _______________________) (If yes, what type?_____________________________________) Women’s Health (women only please) Age of first menstruation ____________________ Age of menopause _____________________ Date of last pap smear ____________________ Number of pregnancies _____________________ Number of live births ____________________ Number of miscarriages ____________________ Birth control Y N If yes, what type? ____________________________________________________________ Hysterectomy Y N If yes, when? _________________________ Full or partial? ____________________ Abnormal pap smear? Y N If yes, when? _________________________ Please circle below as pertains to you Self breast exams Breast lumps Breast pain Nipple discharge Endometriosis Ovarian cysts Fibroid tumors Frequent yeast infections Impaired fertility Sexual difficulties Are you sexually active? Y N STI/STD’s? Y N (If yes, what type?_______________________________________) If you are still menstruating Length of cycle _____________ Irregular cycles PMS Y N Length of flow (days) _____________ Painful menses Spotting Heavy flow If yes, what are your symptoms? ________________________________________________________________________ _______________________________________________________________________________________________________________________________ If you are in menopause please circle below as pertains to you Hot flashes Vaginal dryness Changes in memory Dry skin Spotting Decreased libido Mood changes Hair loss Urinary incontinence Urinary tract infections Hormone replacement Y N If yes, what type? _______________________________________________ Review of Systems Body temperature: Normal Warm natured Flushed face Warm palms Warm soles Cold hands / feet Alternate chills and fever Other Perspiration: Normal Without exertion Very little Palms Digestion: Normal Bitter taste in mouth Nausea/vomiting Abdominal pain or cramps Easily Strong odor Night sweats Spontaneous without exertion Indigestion Belch or burp Bloating Bad breath Stomach noises Gas Difficulty digesting fatty / oily foods Bowels: How many times per day? _______________________ Normal Loose stool Undigested food in stool Pain or cramps Stool with bad smell Use laxatives Small amount of stool Intestinal worms Black stool Other Thirst: Normal Less than normal Thirsty but do not drink Excessive Other Headaches – Dizziness: Headaches Vertigo Bend down and get up / get dizzy Migraines Poor balance Other Heartburn Gallstones Full feeling or distention Weight problems Nervous stomach Other Profuse Cloudy Strong smell Clear/yellow Kidney stones or infections Prefer cold drinks Awake easily Sleep too much Restless Lots of dreams Other Profuse Other Blood in stool Diarrhea Hemorrhoids Hard stool Constipation Difficult to pass stool Mucous in stool Burning Anus Urination: (three to four times a day is normal) Normal Frequent Burning Urgency Painful Scanty Nighttime Blood Not normal color Bladder infections Sleep: Normal Difficulty falling asleep Tired when waking up Cold natured Feel warmer late afternoon/evening Incontinence Other Prefer hot drinks Difficulty getting back to sleep Nightmares Motion sickness Dizziness Poor memory Faint easily Skin: Normal Cuts heal slowly Bruise easily Dry Pimples Body odor Hives Rashes Yellow skin Clammy Moles Other Ulcers Itching Warts Eczema Boils Oily Hair: Normal Dry Oily Dandruff Falling out Early grey Other Nails: Normal Ridges and lines Soft Purple Grow fast Break easily Grow slowly Other Spots Pale Eyes: Normal Color blindness Sensitive to light Inflammation Tear easily Wear glasses or contacts Eyelids swollen Poor night vision Spots or lines in vision Pale under eyelids Cataracts Dry Sty history Strain Yellow sclera Glaucoma Itch Failing vision Twitch Red Blurry vision Blink frequently Pain Other Ears: Normal Itching Nose: Normal Blow nose a lot Other Mouth and Throat: Normal Feel lump in throat Drool a lot Sores mouth/tongue Discharge Hayfever Sinusitis Difficulty hearing Sneeze a lot Loss of smell Teeth problems Grind teeth Hoarseness Frequent sore throats Mucous Bleeding Pain: Low back Hands or wrists Foot or ankle Damp weather Chest pain Murmur Palpitations Bleed easily Varicose veins Shoulder Sciatica Nerve Other Rhinitis Stuffy nose Environmental sensitivity Dry Frequent colds TMJ Swollen glands Frequent sinus infections Difficulty swallowing Respiratory: Normal Chest pain Dry cough Difficulty inhaling Sighs Bronchitis Difficulty breathing w/lying down Cardiovascular / Circulaion: Normal High blood pressure History of anemia Slow beating heart High cholesterol Broken blood vessels/capillaries Ring (low/high pitched) Other Mid back Hips Arthritis Cough a lot Difficulty exhaling Cough w/blood Tightness in chest Hiccups Thyroid problems Gum problems Other Shortness of breath Cough with phlegm Asthma Other Facial swelling Low blood pressure Ankle swelling Diagnosed heart problems Hand swelling Irregular heart beat Bruise easily Purple palms/fingers Numbness in extremities Other Upper back Neck Foot/ankle Knees Spine Muscle weakness Flank area Muscle twitching Any other problems you would like to discuss? ______________________________________________________________________ Thank you for taking the time to answer the questions above. I certify that the information I have given above is correct and accurate to the best of my knowledge. ____________________________________________________________________________ Patient or Guardian signature ____________________________________________________________________________ Printed patient name ______________________________ Date Practitioner Notes: Tongue: __________________________________________________________________________ Pulse: R: ______________________________________________ L: ______________________________________________________________ TCM DX: _______________________________________________________________________________________________________________ Points: Gua Sha Moxa Cupping Tui Na Auricular: