O43 A Prognostic Model for Risk of Encapsulating Peritoneal
advertisement
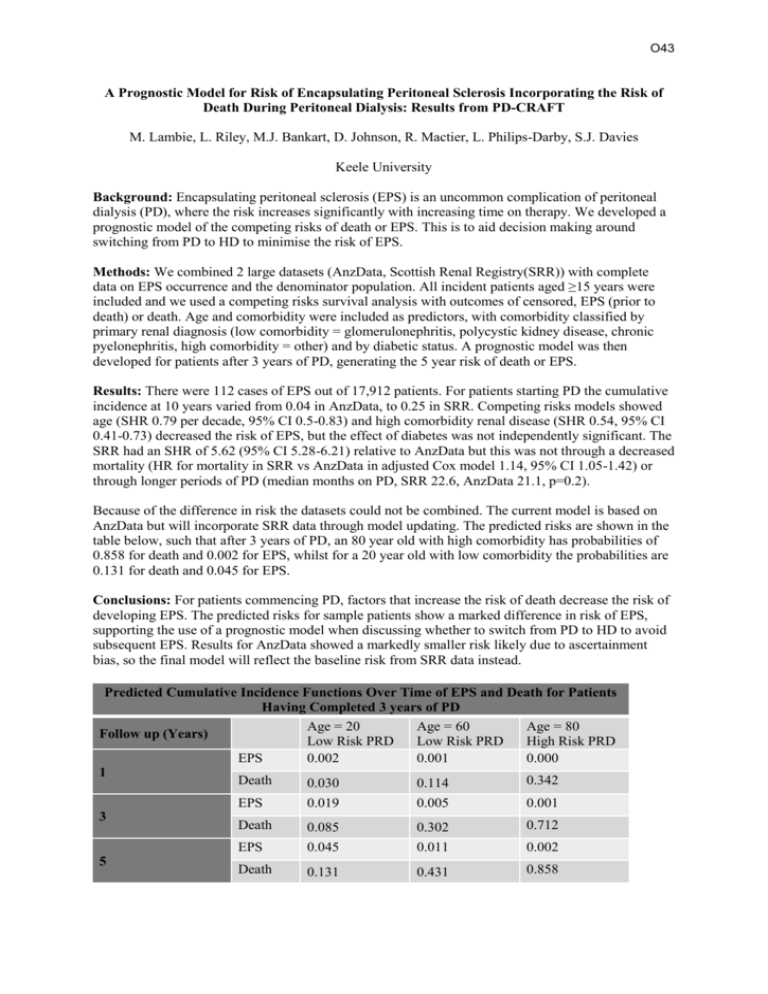
O43 A Prognostic Model for Risk of Encapsulating Peritoneal Sclerosis Incorporating the Risk of Death During Peritoneal Dialysis: Results from PD-CRAFT M. Lambie, L. Riley, M.J. Bankart, D. Johnson, R. Mactier, L. Philips-Darby, S.J. Davies Keele University Background: Encapsulating peritoneal sclerosis (EPS) is an uncommon complication of peritoneal dialysis (PD), where the risk increases significantly with increasing time on therapy. We developed a prognostic model of the competing risks of death or EPS. This is to aid decision making around switching from PD to HD to minimise the risk of EPS. Methods: We combined 2 large datasets (AnzData, Scottish Renal Registry(SRR)) with complete data on EPS occurrence and the denominator population. All incident patients aged ≥15 years were included and we used a competing risks survival analysis with outcomes of censored, EPS (prior to death) or death. Age and comorbidity were included as predictors, with comorbidity classified by primary renal diagnosis (low comorbidity = glomerulonephritis, polycystic kidney disease, chronic pyelonephritis, high comorbidity = other) and by diabetic status. A prognostic model was then developed for patients after 3 years of PD, generating the 5 year risk of death or EPS. Results: There were 112 cases of EPS out of 17,912 patients. For patients starting PD the cumulative incidence at 10 years varied from 0.04 in AnzData, to 0.25 in SRR. Competing risks models showed age (SHR 0.79 per decade, 95% CI 0.5-0.83) and high comorbidity renal disease (SHR 0.54, 95% CI 0.41-0.73) decreased the risk of EPS, but the effect of diabetes was not independently significant. The SRR had an SHR of 5.62 (95% CI 5.28-6.21) relative to AnzData but this was not through a decreased mortality (HR for mortality in SRR vs AnzData in adjusted Cox model 1.14, 95% CI 1.05-1.42) or through longer periods of PD (median months on PD, SRR 22.6, AnzData 21.1, p=0.2). Because of the difference in risk the datasets could not be combined. The current model is based on AnzData but will incorporate SRR data through model updating. The predicted risks are shown in the table below, such that after 3 years of PD, an 80 year old with high comorbidity has probabilities of 0.858 for death and 0.002 for EPS, whilst for a 20 year old with low comorbidity the probabilities are 0.131 for death and 0.045 for EPS. Conclusions: For patients commencing PD, factors that increase the risk of death decrease the risk of developing EPS. The predicted risks for sample patients show a marked difference in risk of EPS, supporting the use of a prognostic model when discussing whether to switch from PD to HD to avoid subsequent EPS. Results for AnzData showed a markedly smaller risk likely due to ascertainment bias, so the final model will reflect the baseline risk from SRR data instead. Predicted Cumulative Incidence Functions Over Time of EPS and Death for Patients Having Completed 3 years of PD Age = 20 Age = 60 Age = 80 Follow up (Years) Low Risk PRD Low Risk PRD High Risk PRD EPS 0.002 0.001 0.000 1 Death 0.342 0.030 0.114 3 5 EPS 0.019 0.005 0.001 Death 0.085 0.302 0.712 EPS 0.045 0.011 0.002 Death 0.131 0.431 0.858