Improving Outcomes: Standardizing a Process for Pediatric IV
advertisement

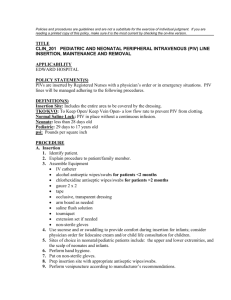
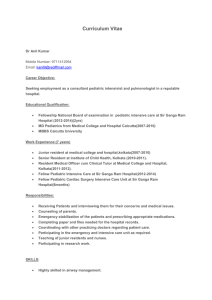
Abstract 17 Roger W. Meece, BSN, RN, CPN; Michelle Rhoads, RN, MSN, APRN-BC Nemours/A. I .duPont Hospital for Children rmeece@nemours.org Title: Improving Outcomes: Standardizing a Process for Pediatric IV Insertion on a Sedation/Infusion Unit Objectives: The aim of this evidence-based initiative is to improve outcomes related to peripheral intravenous (PIV) insertion in pediatric patients on a sedation/infusion unit by developing a standard process for PIV insertion. Introduction: Even in the most skilled hands, pediatric IV placement offers many challenges. The literature states that IV placement, even when successful on the first attempt, may be very stressful for the patient and family. A review of relevant literature related to outcomes of IV placement success rates on the first attempt range from less than 50% to greater than 90%. A myriad of factors, ranging from body habitus, dehydration, and staff variables, such as feeling rushed or a lack of experience influences whether an IV will require one attempt or more. Every aspect of our nursing practice related to PIV insertion, including the significance of proper hydration, the synergistic process of pairing the ideal nurse and patient, and providing optimal pain management strategies were evaluated. Methods: 1. Reviewed relevant literature related to outcomes of pediatric IV insertion; 2. Retrospectively and prospectively collected data from post sedation phone calls and medical records regarding PIV placement; and 3. Queried staff regarding all barriers to successful PIV insertion. Results OR Practice Implications: Utilizing an evidence-based approach to improve patient outcomes has become an integral part of our nursing practice. Although this initiative is not yet complete, the authors are already documenting evidence of improved outcomes related to PIV insertions. Conclusions: Our post-sedation/infusion calls have consistently identified the most frequent concern of our families as related to PIV placement. This initiative evaluated every aspect of our practice related to PIV placement with the goal of improving patient outcomes. References: 1. Larsen et al., Journal of Infusion Nursing. 2010: 226-234. 2. Lininger, Ann., Pediatric Nursing. 2003: 29(5). 3. Spanos, Stephanie et al., Pediatric Emergency Care. Volume 24(8): 511-515. Funding Source: None