paediatric respiratory medicine: assessment guidance
advertisement

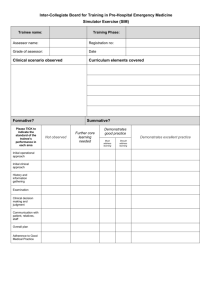
PAEDIATRIC RESPIRATORY MEDICINE: ASSESSMENT GUIDANCE AIM OF THE ASSESSMENTS Reassuring the individual, the profession and the public, as well as employers and regulatory bodies that a trainee is fit to practise. THE EDUCATIONAL PURPOSES FOR THE ASSESSMENT SYSTEM ARE: 1. To support learning and progression across the curriculum. 2. To assess the level of competence achieved at different stages of the training. 3. To produce level 3 competency Paediatric Respiratory Consultant. The assessment system is to be used to reassure the trainee and provide the trainee with feedback about their own knowledge, skills and attitudes and the opportunity to show progression and development through their training programme. In order to achieve this, all areas of the training curriculum need to be sampled and assessed in the most appropriate ways, according to the nature of the knowledge or skill being assessed. The aim at level 3 the trainee is learning to work independently within team and developing further many of the non-technical competences which will be assessed through Portfolio and the range of workplace based assessments. Trainees will be developing expert clinical reasoning, which makes CbD particularly valuable at this stage. The core assessment instruments for level 3 trainees are: 1. Portfolio 2. Workplace based assessment 3. Trainer Report The purpose of the individual assessment instruments within the system will therefore vary. 1. PORTFOLIO The portfolio will underpin learning from the curriculum and act as a platform for trainers and trainees to manage various elements of professional development and assessment required. It will be compiled by the trainees throughout the three years of training period. The portfolio will contain: Professional development plan (after discussion with the trainers) Skills log Record of training events Trainer reports Reflective events Teaching and presentation Audit/research Clinical ethic and safety/quality issues (QA project, clinical audit etc) 2. ASSESSMENT OF PERFORMANCE a. MSF (multisource feedback) The Sheffield Peer Review Assessment Tool, originally validated for use in paediatrics (Archer 2005), has been adapted to each level of training in Paediatric Respiratory. This instrument is invaluable for assessing a trainee’s performance over time, in everyday practice. It provides multi-source feedback, also known as 360° assessment (MSF). The reliability and validity of MSF has been evaluated in its development and implementation stage, and it has proved to be a robust assessment tool. MSF generates structured feedback which can be used as part of personal development planning. A minimum of 2 assessments are required per year. If during the first year training, the trainee did not obtain a single satisfactory assessment, it should be brought up to the Paediatric Respiratory Sub-Speciality Committee to decide on further action. b. MiniCex (Mini Clinical Evaluation Exercise) (Holmboe 2003,2004 & Norcini 2005). The instrument has been modified to map to paediatric respiratory assessment standards. MiniCeX is a workplace based assessment tool designed to provide feedback on skills essential to the provision of good clinical care. The instrument enables us to assess trainees in real patient encounters. In keeping with a quality improvement assessment model, strengths, areas for development and agreed action points will be identified following each Mini -CEX encounter. It samples a range of areas within the assessment standards and can be mapped to Good Medical Practice. Mini-CEX is suitable for use in an out-patient, in-patient or acute care setting. The assessor must have actually OBSERVED the part of the encounter they are rating. It is not designed to assess a reported encounter. Example of suitable encounters could include: Examination of a patient and explanation of the findings on the ward round Initial history taking for a patient who is newly admitted Review of a patient with a chronic illness such as CF A trainee demonstrate a variety of inhaler devices to parents and children and select appropriate devices for clinical situation Interpret CXR and CT chest Immediate feedback will be provided after each encounter by the assessor rating the trainee focusing on aspects of the discussion of the encounter where the trainee did especially well (anything especially good), suggestions for development and any agreed action should be provided and documented. A minimum of 4 assessments are required per year. If the assessment is not satisfactory, it has to be repeated within that 3 months posting. c. CbD (Case-Based Discussion) (Davies 2005 & Davies 2005). The instrument developed has been modified to map to paediatric respiratory assessment standards. CbD is a workplace based assessment tool for paediatric respiratory trainees that have been designed to assess clinical reasoning skills and the ability to bring an analytical approach to diagnosis and management of paediatric respiratory conditions. It allows trainees to discuss why they acted as they did. Ideally half the cases should be selected by the trainee and half by the assessor. The cases selected should cover a range of clinical problem areas and should be cases that reflect their stage of training. Discussion should be based on the entry made in the notes and exploring the thought processes that underpinned the entry. It should not be seen as an opportunity to conduct a viva but should be seen as an opportunity to explore their clinical reasoning and decision making. A few possible questions are set out below to provide an example of the sort of style of questioning that is effective: What was going through your mind when you wrote that management plan, just talk me through your thought process? I see that you have written down a number of different investigations – how did you think the results would help you work out what was going on and what you needed to do? You have referred to the ward guidelines in your notes – tell me a bit about how you used the guidelines to help plan management and whether there were any aspects that didn’t fit in this case? I see that you have decided to treat child with xx – talk me through how you decided to prescribe that regime and what the alternatives you considered were? You have written down that you were going to ask Dr X for their advice – what specifically did you want to discuss with them, why was it important in this case, how did their advice help and what did you learn from it? The discussion must start from and be centred on the trainee’s own record in the notes. Following discussion of the case the assessment record should then be filled out. Immediate feedback focusing on aspects of the discussion of the case where you felt the trainee did especially well (anything especially good), suggestions for development and any agreed action should be provided and documented. A minimum of 4 assessments are required per year. If the assessment is not satisfactory, it has to be repeated within that 3 months posting. d. SAIL (Sheffield Assessment Instrument for Letters) Sheffield Assessment Instrument for Letters (SAIL) has been developed and validated for use in paediatrics (Crossley 2001 Fox 2004). SAIL is a workplace based assessment tool designed to assess clinic letters and other written communication. The instrument assesses a trainee’s competence in written communications in everyday practice, over time A feedback will be provided based on the written letter or other written communication by the assessor rating the trainee focusing on where the trainee did especially well (anything especially good), suggestions for development and any agreed action should be provided and documented. A minimum of 4 assessments are required per year. If the assessment is not satisfactory, it has to be repeated within that 3 months posting. e. DOPs (Directly Observed Procedural Skills) DOPS is a workplace-based assessment tool designed for the assessment of practical skills. It is considered appropriate to assess most practical procedures and a range of practical procedures have been identified for assessment. Following discussion the assessment record should then be filled out by the assessor. Immediate feedback focusing on aspects of the discussion where you felt the trainee did especially well (anything especially good), suggestions for development and any agreed action should be provided and documented Minimum of one satisfactory DOPs assessment for each procedure listed in the log book. 3. TRAINER’S OVERALL ASSESSMENT REPORT The report should be based on the trainee’s portfolio (including log book) and the tools used for work-based assessment performance. MSF: MiniCEX: CbD: SAIL: DOPs: minimum 2/year minimum 4/year minimum 4/year minimum 4/year One for each procedure required in the log book The trainee will be assessed every 6 months and during the first year of training, if there is no satisfactory MSF/trainer’s report, the trainee should be assessed by a different Paediatric Respiratory Consultant. If the assessment by second consultant remained unsatisfactory the discussion should be made by the Paediatric Respiratory Sub-Speciality Committee to decide whether the trainee is fit to continue in the training programme. Adapted from Royal College of Physician and Child Health 2010. Prepared on 190513