Team Triage: Reducing the Length of Stay in the Emergency Center
advertisement
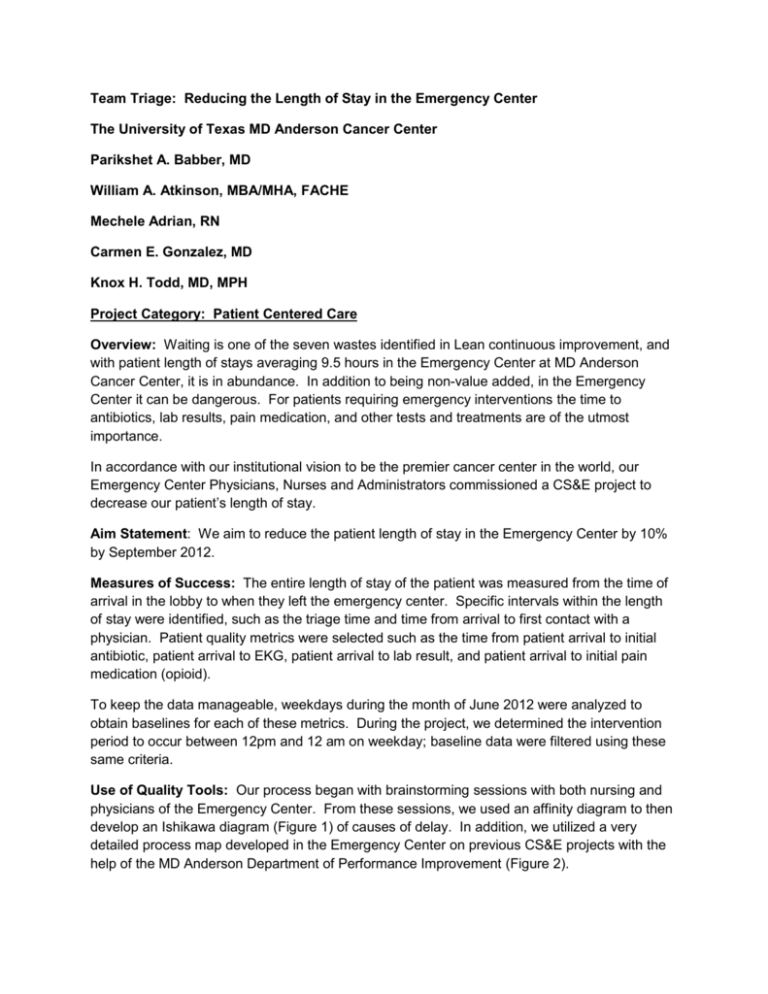
Team Triage: Reducing the Length of Stay in the Emergency Center The University of Texas MD Anderson Cancer Center Parikshet A. Babber, MD William A. Atkinson, MBA/MHA, FACHE Mechele Adrian, RN Carmen E. Gonzalez, MD Knox H. Todd, MD, MPH Project Category: Patient Centered Care Overview: Waiting is one of the seven wastes identified in Lean continuous improvement, and with patient length of stays averaging 9.5 hours in the Emergency Center at MD Anderson Cancer Center, it is in abundance. In addition to being non-value added, in the Emergency Center it can be dangerous. For patients requiring emergency interventions the time to antibiotics, lab results, pain medication, and other tests and treatments are of the utmost importance. In accordance with our institutional vision to be the premier cancer center in the world, our Emergency Center Physicians, Nurses and Administrators commissioned a CS&E project to decrease our patient’s length of stay. Aim Statement: We aim to reduce the patient length of stay in the Emergency Center by 10% by September 2012. Measures of Success: The entire length of stay of the patient was measured from the time of arrival in the lobby to when they left the emergency center. Specific intervals within the length of stay were identified, such as the triage time and time from arrival to first contact with a physician. Patient quality metrics were selected such as the time from patient arrival to initial antibiotic, patient arrival to EKG, patient arrival to lab result, and patient arrival to initial pain medication (opioid). To keep the data manageable, weekdays during the month of June 2012 were analyzed to obtain baselines for each of these metrics. During the project, we determined the intervention period to occur between 12pm and 12 am on weekday; baseline data were filtered using these same criteria. Use of Quality Tools: Our process began with brainstorming sessions with both nursing and physicians of the Emergency Center. From these sessions, we used an affinity diagram to then develop an Ishikawa diagram (Figure 1) of causes of delay. In addition, we utilized a very detailed process map developed in the Emergency Center on previous CS&E projects with the help of the MD Anderson Department of Performance Improvement (Figure 2). Fishbone Diagram Structure/Supplies Delays in Patient Disposition Documentation No notification of test result Excessive data entry Supplies are in proper location Lab draw times by nurses No cart replenishment Non-MDA patient Radiology off hours No standard room set-up Transportation for radiology Double or incomplete entry triage Layout of physician workroom and nurse pods Location of computers Excessive time for results Excessive time to MD No orders given/available Admitted patient waiting for bed Inefficient diagnosis Patient has no ride home Value add vs. time Room assignment of patients Intake/Triage Social workers not available No house staff or admission orders Discharge Barriers Excessive Length of Stay in EC Physician to nurse communication Room needs/status of test results and orders Interruptions Phone calls to/from services/clinics Communication Figure 1 – Ishikawa Diagram of Length of Stay Wait Times Figure 2 – Emergency Center Process Flow Chart - Triage We utilized Lean tools and concepts to perform our analysis and intervention. Analysis of the process maps showed that numerous external processes such as lab results, consultations, pharmacy, and radiology must occur before a patient could be diagnosed and either admitted or discharged. Thus, we attempted to implement in our intervention a quick changeover by eliminating set-up time (1.86 hours of time from arrival time to the initial orders). Finally, a key feature of our intervention was the use of visual controls. The key to success of the pilot was centered on orders getting carried out earlier by moving them up in the patient cycle time. We accomplished this by moving a physician into the triage area. This meant relaying to many individuals the fact that orders had already been ordered. To accomplish this, we used a bright orange communication sheet and clipped to the outside of the patient chart to emphasize that orders were in. We utilized run charts to measure the results of the intervention. Interventions: Process maps identified numerous causes of delay in patient cycle times through the emergency center. Patients cannot be discharged or admitted until they are effectively diagnosed and stabilized by the emergency physicians. Diagnosis and stabilization cannot occur until lab results are available, radiology tests had been performed, pain had been managed, and consulting physicians had arrived to provide assessment. Delays in any of these cycle’s times cause delays in patient length of stay, often in a cumulative fashion. During our analysis, it was identified that each of these external cycles were dependent upon initial physician orders. As the median time to physician was 1.55 hours, and the time to initial orders was 1.86 hours, we determined our greatest opportunity to reduce patient length of stay was to move orders up earlier in the process. Our intervention was to reduce set up time by moving one of our physicians to triage, the intake area of the emergency center. This would allow us to reduce the time it took for a patient to see a physician, and thus, the time to receive orders up significantly in the process. By moving orders earlier in the patient visit, each cycle has an earlier start time. In addition, it is a patient friendly approach, as the first person a patient came into contact with in an emergency situation was a doctor, which we believed would be a huge patient satisfier. Results: As of August 9th, we have completed the first week of the pilot, and have analyzed the intervention period vs. the June baseline period. During the intervention period, we observed a decrease in the median patient length of stay of 1.49 hours (Figure 3) or 16.5%, and a decrease in the median patient time to physician of 66 minutes 71% or (Figure 4). The time to initial orders, the key to reducing set up time, decreased from a median of 111.6 minutes to 27 minutes, or 75.8%. Figure 3 – Median Length of Stay Pre- and Post- Intervention Figure 4 – Median Patient time to Physician Pre- and Post- Intervention Decreases in total time to completion for the external processes were observed as well during the intervention period. The time from arrival to initial pain medication for the patient dropped 53% from 2.56 hours to 1.18 hours, and the time from arrival to initial antibiotic dropped 54% from 2.85 hours to 1.35 hours (Figure 5). We also observed a decrease in time for lab results from 2.98 hours to 2.03 hours, or 31.8%. Department of Emergency Medicine - Quality Metrics Team Triage Intervention - Hours to Initial Opiod and Antibiotic 2.85 3 2.56 2.5 2 1.35 1.18 1.5 1 0.5 0 Lobby to Opioid Lobby to Antibiotic 53% decrease (82 minutes) in TimePretoIntervention initial Pain Medication, and 54% decrease (90 Team Triage minutes) in time to Initial Antibiotic based on week one of team triage intervention. Figure 5 – Median Time to Antibiotic and Opioid Pre- and Post- Intervention We also observed a decrease in time to EKG of 28%, from 22.5 minutes to 16.2 minutes. While a smaller decrease was seen in EKG times, the percentage of patients that had their EKG performed with 20 minutes was 75% in the post -intervention vs. only 45% pre-intervention. The only increase in time we observed was that of arrival to triage, where the median time increased 6 minutes from a median of 21 minutes to 27 minutes. It was noted that triage time also became physician time and initial order time. Revenue Enhancement/Cost Avoidance/Generalizability: It is too soon to identify tangible cost savings or revenue enhancement, although it should be noted that the project was margin neutral as a physician was moved from working patient rooms to triage, and was not additional staffing. This did free up a nursing position in the triage area (there were two prior to intervention), however the triage team utilized the “extra” nurse to assist with EKG, or help with discharges upstairs. If a 1.5 hour length of stay reduction became standard, it could be assumed that significant cost savings or revenue enhancement would be recognized; extra hours equal extra capacity. Should that capacity be filled with additional patients, it would result in a net increase in revenue for the department. If the capacity remained unfilled, it could lead to a reduction in the number of physicians required to treat patients, a potential costs savings, as some shifts are filled with external contingent physicians. There is also evidence that suggest that reduced length of stays in the Emergency Center result in decreased patient length of stay in the hospital, due to more rapid access to antibiotics, etc. One could expect the healthcare system as a whole to realize reduced costs from reduced length of stay, and we aim to measure this in the near future. Conclusions and Next Steps: Physician orders drive almost every external process related to patient length of stay. Moving the physician to triage reduces set up time and thus far has shown the potential to have a large impact on length of stay, quality, patient satisfaction such as time to opioid, and time to physician. At the time of this abstract, one week of intervention has been completed, and the second week will begin Monday, August 20th. At this point, the data will be compared to the non-intervention weeks to fully evaluate the intervention. Early feedback from faculty, nurses and patients have been positive, particularly in regard to pain medications being available to patients earlier and the physician being the first provider the patient encounters. The intervention presents some challenges. Physician workload is one potential challenge. Physicians now each have to see more patients per shift since one of their colleagues is in the triage area. We are examining ways to alleviate this added patient load. We look to implement a version of this intervention full time, if the data continues to support this quality initiative.