Finished Xcredit
advertisement
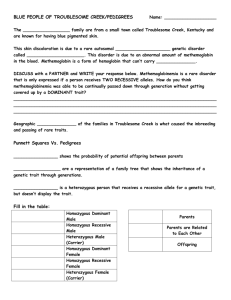
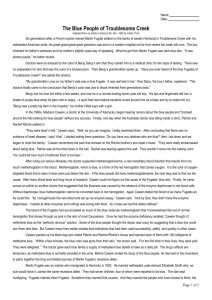
Review of: THE BLUE PEOPLE OF TROUBLESOME CREEK The story of an Appalachian malady, an inquisitive doctor, and a paradoxical cure. By: Kale Hintz 4/9/2014 The family of Martin Fugate and his American bride had a genetic disease that was passed down six generations to their great-great-great-great grandson, Benjy Stacy’s. When Benjy was born, his skin had a blue tint. The doctors were perplexed by his appearance and were attempting to figure out how to fix his bluish appearance. The medical team decided they were going to give him a transfusion to try to help him, until Benjy’s grandmother asked the doctors if they had ever heard of the blue Fugates of Troublesome Creek. Martin Fugate was a French orphan who settled on the banks of eastern Kentucky’s Troublesome Creek. His family had an unexplainable disease that caused their skin to appear as a “bruised plum”. The doctors came to the conclusion that Benjy had inherited the disease from Benjy’s grandmother’s grandma, who was a Fugate from the troublesome creek. Within a few weeks the blue tint dissipated and the boy grew up normally. The only sign of the disease is when he would get cold or angry his lips and fingernails would turn a blue-purple shade. Benjy had inherited piece of the Fugate family that he would carry for the rest of his life and would possibly pass on to his children. This disease hadn’t created any serious complications for this family, most of the effected people lived well into their 80’s and 90’s. In the early generations the family wasn’t visited by doctors to discover the cause of the deformity, the “blue people” kept to themselves because they were the only of their kind, most people were either white or black and being blue made them stick out. By the time that a hematologist decided to try to help cure the blue people, the recessive gene had been passed on through several generations all over the area. In 1960, a hematologist named Madison Cawein, from the University of Kentucky’s Lexington medical clinic, and a nurse from Hazard Kentucky, named Ruth Pendergrass, began to search the hills to find the blue people. Cawein was interested in this suspicious case because he had been an Army medical technician in WWII, and he had always liked the way that blood look. Pendergrass was introduced to the disease on a cold day when a woman came in from a very cold day to the clinic asking 1 for a blood test, the woman appeared blue and her fingernails were almost purple. Pendergrass thought that the woman was having a heart attack, and expected the woman to die right in the clinic, but the woman explained that she was from the family of the blue Combses from Ball Creek. After many times of running up and down the hills trying to find some of the blue people, Cawein had some luck when another blue person came into the clinic. The patients name was Rachel Ritchie; she was very embarrassed of being blue and would not wait in the waiting room with the other patients. Cawein conducted some tests and came to the conclusion that the blue was not caused from heart or lung disease. After these tests he began charting out the family history. Cawein drew lots of blood to conduct tests and to figure out what exactly was causing the blue tint. He tested for abnormal hemoglobin, but the test came back negative. Cawein then turned to medical journals to try to find cases that were similar to this one. He found a very similar case from E. M. Scott's 1960 report in the Journal of Clinical Investigation (vol. 39, 1960). In this case, “Scott, at the Arctic Health Research Center in Anchorage had discovered hereditary methemoglobinemia among Alaskan Eskimos and Indians. Scott speculated, by an absence of the enzyme diaphorase from their red blood cells. Normally, hemoglobin is converted to methemoglobin at a very slow rate. If this conversion continued, all the body's hemoglobin would eventually be rendered useless. Normally diaphorase converts methemoglobin back to hemoglobin. Scott also concluded that the condition was inherited as a simple recessive trait. In other words, to get the disorder, a person would have to inherit two genes for it, one from each parent. Somebody with only one gene would not have the condition but could pass the gene to a child.” (Trost, 1982) To better understand what this disease truly is a simple medical breakdown of the word will help explain the disease for those who don’t understand medical termenology. The breakdown of the disease known as Methemoglobinemia is: Methem- (Methylamine) is the organic compound. This colorless gas is a derivative of ammonia, but with one H atom replaced by a methyl group. Globin- (protein) Emia- (blood condition). 2 Simply putting these together one can get a simple understanding of this disease which is; Methemoglobinemia is a disease that affects proteins in the blood that disrupts gas exchange. Cawein concluded that if this case was like the case that Scott had studied, there would be relatives to his patient that would have the recessive gene or even more blue people. This would be very prevalent in an inbred family line. Cawein went back to Hazard to search out some of the Richies to get some more blood samples. He was sent to a town named Hardburly, where he was introduced to Richie uncle who was also blue. From there he went to go find the patriarch of the Troublesome Creek clan and this man took Cawein farther up the hill to Aunt Bessie Fugate, who was also blue. After attaining all of these samples Cawein brought the samples back and began setting up Enzyme assay and found that the enzyme diaphorase was missing and with further testing other enzymes had nothing wrong with them. This meant that he had defined the cause of the defect, meaning that the blue disease was caused from a buildup of this blue molecule and the red hemoglobin that normally showed through the skin to give it a pink tint was overpowered, creating the blue-purple tint. Cawein was able to conclude that methylene blue would turn the blue tint back to pink because the methylene would act as an electron donor and would convert the methemoglobin back to normal. Cawein and Pendergrass headed to the Ritchie’s house and injected them with a dose of the methylene blue, and within a few minutes the blue tint has subsided and they were pink for the first times in their lives. Because methylene is excreted through urine Cawein gave the Richie’s a daily pill that would act as the injection had. Before he stopped studying the blue people, Cawein looked farther into the family ancestry. He found that: Martin Fugate immigrated to Kentucky in 1820, and lived on the wilderness banks of Troublesome Creek. Cawein found that Fugate’s family lore stated that Martin himself was blue. Although it was very unlikely that Martin would find a wife with the same recessive gene, he managed 3 to find Elizabeth Smith who also carried the recessive gene. Martin and his wife started a family at Troublesome Creek and of their seven children, four were reported to be blue. The clan had more children and their numbers increased, spreading the recessive much quicker than what it would in a normal population. Fugates married other Fugates, often first cousins marrying each other. They also married into the Combses, Smiths, Ritchies, and Stacys families. All of these families lived in isolation from the world, so it was only natural that a boy married the girl next door, even if she had the same last name. Martin and Elizabeth Fugate's blue children multiplied in this natural isolation tank. Zachariah, one of their blue boys, married his mother’s sister, which triggered the line of succession that would result in the birth, more than 100 years later, of Benjy Stacy. When Benjy was born with purple skin, his relatives told the perplexed doctors about his great grandmother Luna Fugate. Luna's father, Levy Fugate, was one of Zachariah Fugate's sons. Luna had good health common to the blue people, bearing 13 children before she died at an age of 84. The clinic doctors only saw her a few times in her life and never for anything serious. As coal mining and the railroads brought more people to Troublesome Creek and Kentucky, the blue Fugates started moving out of their isolated communities and marrying other people. This caused the disease to dissipate because it is a recessive gene, so it much less likely for two families to come together with the same recessive gene. Benjy Stacy is one of the last blue Fugates. With Fugate blood on both his mother's and his father's side, the boy could have received genes from either direction. Because the boy was only blue at birth, Benjy is assumed to have inherited only one gene for the condition. Such people tend to be very blue only at birth, probably because newborns normally have smaller amounts of diaphorase. The enzyme eventually builds to normal levels, like in Benjy’s case, because they carry only one of the genes. 4 Through future reviews of this case and the cases that have lead up to it, modern clinicians have concluded that, “ Methemoglobinemia may be passed down through families (inherited or congenital). Or, it may be caused by exposure to certain drugs, chemicals, or foods (acquired). Methemoglobinemia is typically passed on by both parents. The parents usually do not have the condition themselves, but they carry the gene that causes the condition.” (M. Fernadez & Bocock, 2009) This was the case of Benjy, because his parents both had the recessive gene he received the gene, but luckily he only received the gene from one of his parents, so he only had signs of the disease at birth. With a genetic breakdown of the transference of this disease there are several ways for this disease to be passed to one’s children. As stated earlier, this disease is carried on a recessive trait so in order for it to be passed on to children one of the following must happen: Mother carries (heterozygous) + Father carries (heterozygous)= child is homozygous recessive (blue) Mother carries (heterozygous) + Father carries (heterozygous)= if child receives only one recessive gene from one parent and not from the other they will be a carrier like Benjy but not be blue (heterozygous) If either of the parents is homozygous dominate than the child will be heterozygous and my be a carrier but will show no signs of the disease. (this is why the disease dissipated after more people moved to Kentucky) Or either parentis homozygous recessive or the other is heterozygous. The child will be blue at birth and show mild signs of the disease if they are heterozygous like Benjy The child will be blue if they are homozygous recessive like martin Modern medicine has also discovered that there is two different types of Methemoglobinemia; “Type 1 (also called erythrocyte reductase deficiency) occurs when red blood cells lack the enzyme. Type 2 (also called generalized reductase deficiency) occurs when the enzyme doesn't work anywhere in the body. The second form of inherited methemoglobinemia is called hemoglobin M disease. It is caused by defects in the hemoglobin molecule itself. Only one parent needs to pass on the abnormal gene for the child to inherit the disease.” (PA.Saunders, 2011) Doctors have also discovered that a large list of drugs (in high doses) causes this disease, and that Methylamine blue may not work well for everyone, especially those with certain medical conditions. “Large doses of methylene blue may result in higher levels of methylene blue rather than the 5 leukomethylene blue, which will result in hemolysis and, paradoxically, methemoglobinemia in patients with glucose-6-phosphate dehydrogenase (G6PD) deficiency. Eighteen patients with G6PD deficiency also may not produce sufficient NADPH to reduce methylene blue to leukomethylene blue; thus, methylene blue therapy may be ineffective in these patients” (Rehman & Department of Medicine Hull Royal Infirmar, 2001). When dealing with Methemoglobinemia there are a wide range of symptoms that can be expected. “Symptoms are proportional to the fraction of methemoglobin. A normal methemoglobin fraction is about 1% (range, 0-3%). Symptoms associated with higher levels of methemoglobin are as follows:” (Mary Denshaw-Burke, 1997) 3-15% - Slight discoloration (eg, pale, gray, blue) of the skin 15-20% - Cyanosis, though patients may be relatively asymptomatic 25-50% - Headache, dyspnea, lightheadedness (even syncope), weakness, confusion, palpitations, chest pain 50-70% - Abnormal cardiac rhythms; altered mental status, delirium, seizures, coma; profound acidosis >70% - Usually, death” (Mary Denshaw-Burke, 1997) Overall I found this article to be very interesting. The part that stuck out to me the most was the simple fix that this disease had, something as easy as getting a shot or taking a pill could clear the symptoms up in just a matter of minutes. Also, the facts that injecting someone with a blue dye made the blue go away. I can’t imagine the thought going through the blue hill people’s minds when the doctor showed up and explained that he was going to give them a shot of the blue injection that would make their blue tint go away. All I can say is, it’s amazing what medicine can do! 6 Works Cited M. Fernadez, F., & Bocock, C. A. (2009). Emergency Medicine Concepts and Clinical Practice (7th ed.). Philadephia, Pa: Mosby Rosen. Mary Denshaw-Burke, M. F. (1997). Methemoglobinemia. (M. Emmanuel C Besa, Ed.) Bloom J, ed. Comprehensive Toxicology., 6th(62), 62. PA.Saunders, E. (2011). Nelson Textbook of Pediatrics (19th ed., Vol. 456.7). (B. R. Kiliengman RM, Ed.) Philadelphia, PA: Stanton BF. Rehman, H. U., & Department of Medicine Hull Royal Infirmar. (2001). Methemoglobinemia (3rd ed., Vol. v.175(3); Sep 2001). (W. J. Med., Ed.) Hull, UK: BMJ Publishing Group. Trost, C. (1982). The Blue People Of Troublesome Creek. 7