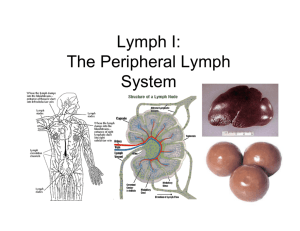
Microanatomy- lymphatics
advertisement

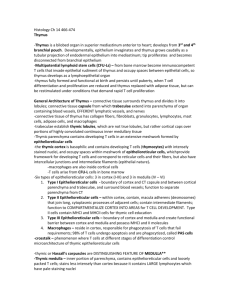
blue/black cells are Von Kuppfer’s cells (macrophages of the liver) – liver cells form plates that are separated by spaces- space of Diess, drainage that opens to lymphatic system, tissue specific macrophages are here Von Kuppfer’s cells space of Disse von Kuppfer’s Cell Space of Disse Recall some of these are antigen presenting- can initiate an immune response early on Trachea (cartilaginous rings evident) esophagus Tracheal epithelium lymphocytes (not encapsulated so not a nodule) lamina propria MALT= mucoid associated lymphoid tissue Lymphocytes are identifiable by very large nucleus- very densely packed, thin surrounding cytoplasm, cell is not associated w/ underlying tissue (usually found in the CT underlying the epithelium) Mammary Glands Glands plasma cell surrounding CT Glands are full of plasma cells that secrete IgA- main source of a neonatal immune system Plasma cell nuclei have DISTINCTIVE wheel spoke nucleus- Plasma cells have an oval shape with an eccentrically located nucleus. The chromatin of the nucleus is arranged in a pattern similar to the spokes of a wagon wheel with a central nucleolus. The cytoplasm is rich in ribosomes and proteins, which usually produce a dark uniform purple stain Plasma cells are activated forms of B cells- create antibodies specific for the antigen that activated them Peyer’s Patches epithelium lumen smooth muscle CT of the LP Peyer’s patches are unilateral in the GI tract- opposite the side of the mesentery Note the patches are located deep to the epithelium w/in the lamina propria (LP is obscured by the density of the patches) All pictured are activated as evidenced by the lighter core (B cells that have undergone blast transformation)- fewer cells filling a larger space Recall patches have a T cell domain and a B cell domain T cell domain faces epithelium of the luminal border (region where M cells are- not distinguished in this stain) T Cell cap Germinal Center- B cell region under active division Epithelium lumen of the SI Palatine Tonsils Stratified squamous mucousal epithelium crypts stimulated follicles non-stimulated B cells from the activated follicles form plasma cells that travel to the lymph vessels of the crypts then into the adjacent lymph nodes where they mature. Once mature the plasma cells return (homing) to the tonsil and are active against the antigen that activated them. Smooth muscle glands palatine tonsil tissue Pharyngeal tonsil tissue Seromucus glands Seromucus glands are diagnostic of pharyngeal tonsil tissue as opposed to palatine tonsil tissue which have purely mucus glands Other key diagnostic feature is PCCE (respiratory epithelium) instead of the squamous epithelium of the palatine tonsil Follicles and are other structures are equivalent Lymph nodes: Cortex Medullary sinus paracortex medulla secondary nodule primary nodule medullary cord (cellular islands) Medullary sinuses are lined with macrophages, B cells, T cells and serve as major sites of immune function on the lymph fluid Medullary sinus medullary cord germinal centers paracortex trabecula T cell domain = paracortex in a lymph node (region between germinal centers and the medulla) Medulla – region for collection of lymph fluid, filtration, and return to body 2 functions of lymph nodes- cleaning of lymph, immunological surveillance Lymphocytes enter the cortex through high endothelial venules (difficult to find on posted board) Correct lymph flow path: vein (in the hilus) Lymph Vessel subcapsular sinus to trabecular sinus to medullary sinus to lymphatic lymph vessel valve Issues with edema, varicose veins, DVT, etc. have direct effect on lymph clearance Lymph vessels are driven exclusively by skeletal muscle pump action- valve is composed of endothelium w/ a very thin layer of CT between 2 layers- valves are necessary to prevent backflow in this system Splee An encapsulated structure w/ trabecula Capsule red pulp white pulp T cell domain- form a sheath around the central arteries of the white pulp- periarteriolar sheath (PALS) Red pulp white pulp central arteriole PALS marginal sinus (contains B cells) These vessels are branches of the splenic artery and vein that enter and leave (respectively) the spleen through the hilum. The rest of the organ is taken up by splenic pulp which can be classified as either red or white pulp. White pulp consists of masses of lymphatic tissue, which in stained tissue sections appear as round masses of darkly staining lymphocytes. Germinal centers may or may not be present. The white pulp contains an artery, the central artery. At low magnification, the central artery in cross section appears as a small round, red staining mass in the white pulp. This is diagnostic for the spleen. When the central artery originates from the trabecular artery and leaves the trabecula, it is immediately surrounded by lymphoid tissue (white pulp). This lymphoid tissue is called PALS, periarterial lymphoid sheath. Look for radial branches of the central arteries. Identify the marginal zone region at the periphery of the white pulp. This region is a shell of large but ill-defined vascular tissue called the marginal zone, in which most of the white pulp capillaries are found. This zone is extremely variable in size and content and is completely devoid of sinusoids. In this section, the marginal zone is looser in texture than the white pulp and contains blood cells, lymphocytes, macrophages and reticular cells. The red pulp makes up the bulk of the splenic pulp and is the remaining lighter (red) staining tissue surrounding the white pulp. It contains large numbers of RBCs as well as lymphocytes. Look for the splenic sinuses and splenic cords (Billroth’s cords). At high magnification, the splenic sinuses are endothelial lined spaces. They may be difficult to visualize. They may be packed with RBCs or completely empty. Look for a cross section of a red pulp sinus where the gaps between the endothelial cells are visible. sinusoid- lined by endothelial cells & macrophages (large dark cells = macrophages) Macrophages phagocytose old/damaged RBCs from the sinusoids Thymus- bilobate structure Individual lobules cortex medulla T cells all mature in the cortex Hassell’s Corpuscles – DIAGNOSTIC, derived from type 6 tissue- These are red staining spheres of concentrically layered cells found in the medulla. The lymphocytes in the medulla are not as densely packed as those in the cortex. T-lymphocytes proliferate in the periphery of the cortex and then migrate towards the medulla Cortex medulla blood vessel CT of trabecula hassell’s corpuscles