2014 CAMC Surgical Site Infection (SSI) Hysterectomy Worksheet
advertisement

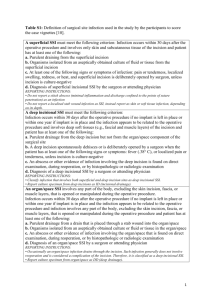
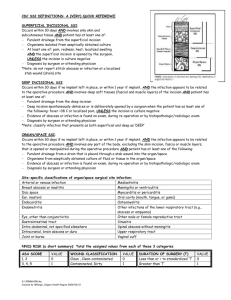
1 2014 CAMC Surgical Site Infection (SSI) Hysterectomy Worksheet Patient name Last: First: *Gender: F M *Event Type: SSI *NHSN Procedure Code: *Date of Procedure: *Date Admitted to Facility (for procedure): *Detected: □ A (During admission) MR #: Acct # Procedure: Acct # Infection: *Date of Birth: *Date of Event (last date to complete criteria): *Outpatient Procedure: Yes No Medicare ID# Hosp: □ P (Post-discharge surveillance) □ RF (Readmission to facility where procedure performed) □ RO (Readmission to facility other than where procedure was performed) **Died: Yes No Event Details SSI Contributed to Death: Yes No Surgeon: Discharge Date (for procedure): Anesthesiologist: *Specific Event: □ Superficial Incisional Primary (SIP) □ Deep Incisional Primary (DIP) □ Superficial Incisional Secondary (SIS) □ Deep Incisional Secondary (DIS) □ Organ/Space (specify site): _______________________ 30 days IAB – Intraabdominal, not specified elsewhere OREP-Other infection of the male or female reproductive tract VCUF – Vaginal cuff SSI Criteria Superficial incisional SSI Deep Incisional SSI Date Date Must meet the following criterion: Infection occurs within 30 days after any NHSN operative procedure*, including those coded as ‘OTH’* AND Involves only skin and subcutaneous tissue of the incision * (where day 1= the procedure date) * (where day 1= the procedure date) AND Patient has at least one of the following: a. Purulent drainage from the superficial incision b. Organisms isolated from an asepticallyobtained culture of fluid or tissue from the superficial incision c. Superficial incision that is deliberately opened by a surgeon , attending physician**, or other designee and is culture-positive or not cultured and Patient has at least one of the following signs or symptoms (CIRCLE): pain or tenderness; localized swelling; redness; or heat. A culture negative finding does not meet this criterion AND Patient has at least one of the following: a. Purulent drainage from the deep incision b. A deep incision that spontaneously dehisces or is deliberately opened by a surgeon, attending physician**, or other designee and is culture-positive or not cultured and Patient has at least one of the following signs or symptoms: fever (>38o); localized pain or tenderness. A culture-negative finding does not meet this criterion ** Attending physician may be interpreted as: Surgeon, infectious disease, other physician on case, emergency physician, physican assistant or nurse practitioner. c. An abscess or other evidence of infection involving the deep incision that is found on direct examination, during invasive procedure, or by histopathologic examination or imaging test. ** Attending physician may be interpreted as: Surgeon, infectious disease, other physician on case, emergency physician, physican assistant or nurse practitioner. d. Diagnosis of a superficial incisional SSI by the surgeon or attending physician. Comment: Must meet the following criterion: Infections occurs within 30 after the NHSN operative procedure* AND involves deep soft tissue of the incision (e.g., fascial and muscle layers Comment: 2 Reporting Instructions: The following do not qualify as criteria for meeting the NHSN definition of superficial SSI If the superficial incisional infection extends into the fascial and/or muscle layers, report as a deep incisional SSI only reportable under this module. A stitch abscess alone (minimal inflammation and discharge confined to the points of suture penetration) A localized stab wound or pin site infection. While it would be considered either a skin (SKIN) or soft tissue (ST) infection, depending on its depth, it is not reportable under this module. Diagnosis of “cellulites”, by itself, does not meet Criterion d for superficial incisional SSI Date Must meet the following Criteria b. c. OREP-Other infection of the male or female reproductive tract (epididymis, testes, prostate, vagina, ovaries, uterus, or other deep pelvic tissues, excluding intraabdominal or vaginal cuff infections) Other infections of the male or female reproductive tract must meet at least 1 of the following criteria: 2. 3. Patient has organisms cultured from tissue or fluid from affected site. Patient has an abscess or other evidence of infection of affected site seen during an invasive procedure or histopathologic examination. Patient has 2 of the following signs or symptoms: fever (>38°C), nausea*, vomiting*, pain*, tenderness*, or dysuria* AND at least 1 of the following: a. organisms cultured from blood b. Physician diagnosis. * With no other recognized cause VCUF-Vaginal cuff infection Vaginal cuff infections must meet at least 1 of the following criteria: 1. a.2. If a patient has an infection in the organ/space being operated on, subsequent continuation of this infection type during the remainder of the surveillance period is considered an organ/space SSI, if organ/space SSI and site-specific infection criteria are met. Occasionally an organ/space infection drains through the incision and is considered a complication of the incision. Therefore, classify it as a deep incisional SSI. Purulent drainage from a drain that is placed into the organ/space Organisms isolated from an aseptically-obtained culture of fluid or tissue in the organ/space An abscess or other evidence of infection involving the organ/space that is found on direct examination, during invasive procedure, or by histopathologic examination or imaging test. AND Meets at least one criterion for a specific organ/space infection site listed. 1. Classify infections that involve both superficial and deep incisional sites as deep incisional SSI. Classify infection that involves superficial incisional, deep incisional, and organ/space sites as deep incisional SSI. This is considered a complication of the incision. Organ/Space SSI Reporting Instructions: Infection occurs within 30 after the NHSN operative procedure and infection involves any part of the body, excluding the skin incision, fascia, or muscle layers, that is opened or manipulated during the operative procedure AND Patient has at least one of the following: a. Reporting Instructions: Post-hysterectomy patient has purulent drainage from the vaginal cuff. Post-hysterectomy patient has an abscess at the vaginal cuff. IAB-Intraabdominal infection, not specified elsewhere including gallbladder, bile ducts, liver (excluding viral hepatitis), spleen, pancreas, peritoneum, subphrenic or subdiaphragmatic space, or other 2ntraabdominal tissue or area not specified elsewhere Intraabdominal infections must meet at least 1 of the following criteria: 1. Patient has organisms cultured from abscess and /or purulent material from intraabdominal space obtained during an invasive procedure. 2. Patient has abscess or other evidence of intraabdominal infection seen during an invasive procedure or histopathologic examination. 3. Patient has at least 2 of the following signs or symptoms: fever (>38°C), nausea*, vomiting*, abdominal pain*, or jaundice* AND at least 1 of the following: a. organisms cultured from drainage from an aseptically-placed drain (e.g., closed suction drainage system, open drain, T-tube drain) organisms seen on Gram’s stain of drainage or tissue obtained during invasive procedure or from an aseptically-placed drain c. Organisms cultured from blood and imaging test evidence of infection (e.g., abnormal findings on ultrasound, CT scan, MRI, or radiolabel scans [gallium, technetium, etc.] or on abdominal x-ray). * With no other recognized cause b. 3 3. Post-hysterectomy patient has pathogens cultured from fluid or tissue obtained from the vaginal cuff. Laboratory – Pathogens identified – attach culture and sensitivity Culture Site: □ culture result □ Positive blood culture __________________________ _______ of _______ bottles □ Blood culture not done or no organisms detected in blood Secondary Bloodstream Infection: Yes No Culture date: Culture result: □ Not cultured □ Positive Gram stain when culture is negative or not done □ Other positive laboratory tests Additional Information: Start _____________ Stop _______________ Time ______________ ( hr & min) ASA________________ Preoperative Antibiotics (dose and time) ____________________ Class______________ Antibiotic Allergy _______________________________________ Anesthesia ______________________ Incision Closure: Primary/ Non- Primary Height (cm) _______________ Glucose: 1st Intra op: ___________________________________ Weight (kg)________________ Highest Intraop: _______________________________ Emergency: Yes No Endoscope/Robotic: Yes Diabetic : Yes Trauma Yes No No No Redose of Antibiotics: _________________________________ Highest 1st day post op: _________________________ Highest 2nd day post op: _________________________ Hair removal __________________________________________ Scrub _______________________________________________ HYST – Abdominal Hysterectomy Abdominal Hysterectomy: Includes those by laparoscope 68.31, 68.39, 68.41, 68.49, 68.61, 68.69 There are two specific Types of Superficial incisional SSIs: 1. 2. SIP – a superficial incisional SSI that is identified in the primary incision in a patient that has had an operation with one or more incisions (e.g., C—section or chest incision for CBGB) SIS – a superficial incisional SSI that is identified in the secondary incision in a patient that has had an operation with more than one incision (e.g. donor site incision for CBGB) There are two specific Types of Deep incisional SSIs: 1. DIP – a deep incisional SSI that is identified in the primary incision in a patient that has had an operation with one or more incisions (e.g., C—section or chest incision for CBGB) 2. DIS – a deep incisional SSI that is identified in the secondary incision in a patient that has had an operation with more than one incision (e.g. donor site incision for CBGB) Secondary BSI Blood and site culture match: o If the criterion met for the primary infection site requires a culture, then at least one organisms form that site must match and organisms in the blood culture (antibiograms- of isolates do not have to match). Only a blood culture – no site culture: o If the criterion met (may or may not require a positive blood culture) for the primary infection site does not require a culture and the blood isolate is a logical pathogen for the site, report as a secondary BSI. Blood and Site Culture do not match: o If the site-specific culture is an element used to meet the infection site criterion and the blood isolate is also an element used to meet another criterion at the same infection site, then the BSI is considered secondary to that site-specific infection o If the site-specific culture is an element used to meet the infection site criterion and the blood isolate is not, then the BIS is considered a primary infection Negative Site-specific culture and positive Blood culture: o If a culture from the suspected site of infection is no growth, but a blood specimen collected as part of the work-up is positive, that BSI is only considered a secondary BSI if another of the site specific criteria that includes positive blood culture as an element is met. Otherwise, the BSI is considered a primary BSI, even if another criterion for that site is met and the blood isolate is a logical pathogen for the infection. Note: Blood and site-specific specimens do not have to be collected on the same day but their collection dates must be such that they are considered part of the diagnostic work-up for the infection in question. 4 * New Incisional Closure Type Definitions: o Primary Closure: closure of all tissue levels during the original surgery, regardless of the presence of wires, wicks, drains, or other devices or objects extruding through the incision. This category includes surgeries where the skin is closed by some means, including incisions that are described as “loosely closed” at the skin level. Thus, if any portion of the incision is closed at the skin level, by any manner, a designation of primary closure should be assigned to the surgery. o Non-Primary Closure: closure that is other than primary and includes surgeries in which the superficial layers are left completely open during the original surgery and therefore cannot be classified as having primary closure. For surgeries with non-primary closure, the deep tissue layers may be closed by some means (with the superficial layers left open) or the deep and superficial layers may both be left completely open. The NHSN protocol includes numerous examples; but in short, anything not meeting the definition of primary closure is by default non-primary closure. 2/4/14