Network HASU capacity - St George`s Hospital
advertisement
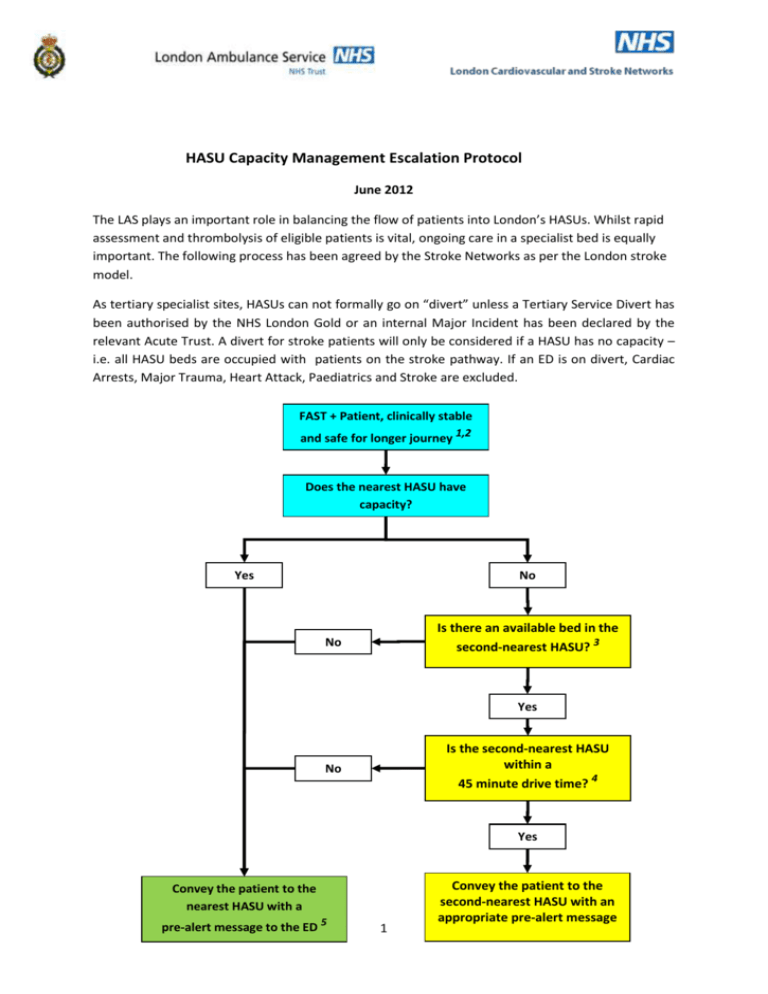
HASU Capacity Management Escalation Protocol June 2012 The LAS plays an important role in balancing the flow of patients into London’s HASUs. Whilst rapid assessment and thrombolysis of eligible patients is vital, ongoing care in a specialist bed is equally important. The following process has been agreed by the Stroke Networks as per the London stroke model. As tertiary specialist sites, HASUs can not formally go on “divert” unless a Tertiary Service Divert has been authorised by the NHS London Gold or an internal Major Incident has been declared by the relevant Acute Trust. A divert for stroke patients will only be considered if a HASU has no capacity – i.e. all HASU beds are occupied with patients on the stroke pathway. If an ED is on divert, Cardiac Arrests, Major Trauma, Heart Attack, Paediatrics and Stroke are excluded. FAST + Patient, clinically stable and safe for longer journey 1,2 Does the nearest HASU have capacity? Yes No Is there an available bed in the second-nearest HASU? 3 No Yes Is the second-nearest HASU within a 45 minute drive time? 4 No Yes Convey the patient to the nearest HASU with a pre-alert message to the ED 5 1 Convey the patient to the second-nearest HASU with an appropriate pre-alert message The default position is that a HASU should accept new onset FAST+ patients from within its catchment area. Clinical Coordination Desk (CCD) has limited capacity and opportunity to influence patient flow. Only those patients who have symptoms within the thrombolysis window are prealerted – other patients are taken in under normal driving conditions, with no routine communication with CCD. Notes: 1. This only applies to patients who are stable, and deemed safe enough to transfer to a more distant HASU. Unstable patients should be taken to the nearest HASU; patients with critical airway compromise or respiratory failure should be taken to the nearest Emergency Department 2. Patients with chronic neurological signs, or where the history is unclear and the diagnosis of acute stroke is unlikely should be taken to the nearest Emergency Department 3. The ‘next nearest’ HASU refers to geographical location, and not ‘nearest available bed’. If there is no bed available in the next nearest HASU, the patient is conveyed to the nearest HASU (i.e. the one where the patient would normally be taken to). Conveying patients beyond the next nearest HASU is not appropriate, as this potentially delays thrombolysis and could become very inconvenient for the patient and his / her relatives 4. “Reasonable Journey Time” is subjective. For example, a patient who is in Romford should be conveyed to Queens Hospital, Romford regardless of their capacity; a patient in Newham could be conveyed to either Queen’s Romford or the Royal London. Journey time should be less than 30 minutes under normal circumstances, and certainly not exceed 45 minutes at times of stress 5. Pre-alert calls should be placed for all patients within the thrombolysis window (4 ½ hours from onset of symptoms), or where the crews have clinical concerns Daily Procedure 1. HASU bed-state only takes into account patients on the Stroke pathway. Outliers from other wards or units should not be counted. 2 2. EBS team will call the HASU clinical coordinators at least twice per 24 hour period, and record the bed status in the database; this should include a prediction of available beds. This is accessible to CCD. 3. CCD will track patient movement, and monitor HASU bed capacity, so that patient flow can be balanced. 4. CCD must keep a record of patients who have been subject to a ‘redirection’, or where a redirection has been considered / discussed. 5. HASUs may call CCD and advise them of capacity at any time. This should be logged and used to guide decision-making. 6. A HASU cannot declare itself “closed” without authority from NHS London Mimics It is recognised that moving presumed stroke patients longer distances increases the potential issues with repatriating stroke mimic patients back to an appropriate centre. Ambulance turn-around and send back is NOT PERMITTED. Escalation The process outlined below is to be used when the whole of the London stroke system is experiencing periods of reduced/minimal capacity. This protocol outlines different levels of escalation, the planned responses and the communications plan. The protocol is based on the assumption that the London HASU model can be considered as an inner group of units (5) and an outer group of units (3) (see map below). Because of journey times redirection to a further HASU is likely to be inappropriate for the 3 outer London units unless HASU is formally closed through NHS London. It should be noted that this protocol is to be seen as a temporary measure to ease short term capacity issues and not a change to the agreed London stroke model. The period of time that this protocol is in operation will not be included in assessment data (assuming the period does not exceed 7 days). 3 All acute stroke patients should be assessed and treated in a HASU. If the HASU does not have a bed, it is incumbent on the HASU provider trust to have a contingency plan to accommodate these stroke patients. It is not appropriate to operate a reduced 'thrombolysis only' service or to transfer a stroke patient from one HASU to another for HASU care. The only occasion it may be appropriate to transfer a HASU patient is if they require other specialist intervention. Network HASU capacity Network HASU Total number of HASU beds North Central London University College Hospital 18 The Royal London Hospital 12 Queen’s Hospital 12 Charing Cross Hospital 20 Northwick Park Hospital 16 King’s College Hospital 12 Princess Royal Hospital 14 St. George’s Hospital 20 North East London North West London South East London South West London Escalation level one Information is received that 3 or more HASUs are reporting capacity of one or zero beds for more than 12 hours. In this instance the following steps will be taken; 1. HASU services reporting low capacity will initiate their provider trust contingency plans to accommodate any stroke patients that require HASU services after low capacity is reported. This is so that patients arriving at the affected HASUs by a route other than through LAS are managed appropriately. 2. Any delay in the transferring of non-stroke patients to the appropriate setting is escalated by the HASU teams in line with cluster mimic repatriation policies where they exist. In the absence of local mimic repatriation protocols, refer to section 3 of the Pan London HASU SU Repatriation Protocol V4 July 2010 (electronic link to be added). If these delays are cross sector they are escalated to the HASU Site Manager1 on call. 3. The relevant network team will contact stroke units in the network to ascertain whether HASU capacity is under pressure due to stroke patient repatriation issues. If this is a factor the Network will request that the appropriate steps are taken to enable repatriation in line 1 See; Appendix two – HASU manager on call communications list 4 with section 5 of the Pan London HASU SU Repatriation Protocol V4 July 2010. This could include, but is not limited to, requesting that stroke units with capacity take patients from outside of their defined SU catchment areas as quickly as possible. These spells will attract the London SU tariff. Escalation level two Information is received that there is a total of 3 or less beds in the inner group of units for at least 12 hours, or if a HASU has to close due to infection (complete steps 1-3 as above). 4. Notification that the London stroke system has moved to escalation level two is sent out from the London Stroke Clinical Director to both the HASU leads and the HASU site managers on call. 5. The HASU consultant on call will cascade this message to the clinical leads at the stroke units in their sectors. 6. During the week (Mon to Friday 9 to 5) the relevant network teams contact the affected HASUs to confirm that their provider trust contingency plans to accommodate any stroke patients that require HASU services have been activated and to receive confirmation of capacity that includes beds provided in these contingency plans. Out of hours and at the week end this is done by the London Stroke Clinical Director or their designated deputy. 7. If capacity pressures are due to stroke patient repatriation issues; all network teams to contact SUs within their sectors that are able to operate timely repatriation in order to arrange for the opening of additional SU capacity and to take patients from outside their normal catchment areas (this could mean taking patients from other sectors). These spells will attract the London SU tariff. Arrangements for additional capacity can be flexible, and agreed on at unit by unit basis with the relevant Network Director. 8. Network teams to collate information with regard to any available additional SU capacity and share with the other network directors and the London Stroke Clinical Director so that additional capacity can be utilised effectively. This additional capacity information is then communicated to the relevant HASU leads. 9. If delays in the transferring of non-stroke patients remain, the network team will escalate to the appropriate Operational Director at both the HASU trust and the receiving trust (if different) in order to facilitate timely repatriation in line with local mimic repatriation protocols, where they exist. In the absence of local mimic repatriation protocols, refer to section 3 of the Pan London HASU SU Repatriation Protocol V4 July 2010. 5 10. If capacity pressures are due to a lack of HASU beds (increased demand) network teams will contact the nominated operational lead at the HASUs affected in their sectors to arrange for further additional capacity beyond the trust’s standard internal contingency plans. Escalation level three Information is received that there is 1 bed or less across the inner group of London HASUs and less than 3 beds are predicted to become vacant. (complete steps 1-10 as above). 11. Notification that the London stroke system has moved to escalation level three is sent out from the London Stroke Clinical Director to both the HASU leads and the HASU site managers on call.2 12. Network teams cascade this message to the clinical leads at the stroke units in their sectors. At the weekend this is done by the London Stroke Clinical Director. 13. The London Stroke Clinical Director or nominated deputy will call a crisis meeting with the Network Directors or their nominated deputies within 3 hours of the decision to escalate to level 3. If this happens over the weekend this meeting will be held as soon as possible on the next working day. 14. Any remaining non-stroke patients in HASUs are transferred to a SU if safe to transfer the patient. This activity should be distributed evenly across the stroke units and based on the postcode look up table as much as possible. 6 Area where redirection to a further HASU is likely to be inappropriate unless HASU formally closed through NHS London Appendix one – HASU lead communications LAS will communicate HASU capacity on a twice daily basis to this group. The London Stroke Clinical Director has the responsibility for reviewing HASU capacity on a daily basis and action this protocol when appropriate. London Stroke Clinical Director Tony Rudd, anthony.rudd@kcl.ac.uk 7 HASU Consultant on call telephone number Charing Cross Hospital King’s College Hospital Northwick Park 07774900504 Hospital Princess Royal Hospital Queen’s Hospital The Royal London Hospital Via Switchboard on 01708 435000 Vis Switchboard 0207 377 7000 St. George’s Hospital University College Hospital Clinical Lead Nurse Lead Diane Ames Julia Slark diane.ames@imperial.nhs.uk; julia.slark@imperial.nhs.uk; Dulka Manawadu Maria Fitzpatrick dulka.manawadu@nhs.net; maria.fitzpatrick@nhs.net; Memory Dzvene David Cohen mdzvene@nhs.net David.Cohen@nwlh.nhs.uk; Sue Fenwick Elliott Sue.fenwickelliott@nhs.net Bart Piechowski Chris Terrahe b.piechowski-jozwiak@nhs.net cterrahe@nhs.net; Sreeman Andole sreeman.andole@bhrhospitals.nhs.uk Ann Russell Ann.RUSSELL@bhrhospitals.nhs.uk; Ann Rush Patrick Gompertz ann.rush@bartsandthelondon.nhs.uk; patrick.gompertz@nhs.net; Jo Baylon josefa.baylon@nhs.net Hugh Marcus Alison Loosemore hmarkus@sgul.ac.uk; alison.loosemore@stgeorges.nhs.uk; Rob Simister Simone Browning robert.simister@uclh.nhs.uk; simone.browning@uclh.nhs.uk; Network Director Network Clinical Lead Hilary Walker hwalker3@nhs.net; Janet Lailey janet.lailey@nhs.net Charlie Davie c.davie@ucl.ac.uk; North West London Hilary Walker, as above Diane Ames, as above South East London Lucy Grothier lucy.grothier@slcsn.nhs.uk; South West London Lucy Grothier, as above Gill Cluckie gill.cluckie@gstt.nhs.uk; Geoff Cloud gcloud@sgul.ac.uk; Network North Central London North East London Patrick Gompertz, as above 8 Appendix two – HASU manager on call communications list HASU HASU manager on call contact number/email Charing Cross Hospital King’s College Hospital Northwick Park Hospital Sue Fenwick Elliott Copy communication to HASU Clinical Lead Diane Ames diane.ames@imperial.nhs.uk; Dulka Manawadu dulka.manawadu@nhs.net; David Cohen Sue.fenwickelliott@nhs.net David.Cohen@nwlh.nhs.uk; 07787005902 Princess Royal Hospital Bart Piechowski b.piechowski-jozwiak@nhs.net Cass O’Reilly Cass.O'Reilly@bhrhospitals.nhs.uk Queen’s Hospital The Royal London Hospital St. George’s Hospital University College Hospital 01708 435000 Extn 2968 & Dect Phone 6129 Out of Hours through Site Manager via Switchboard on: 01708 435000 Out of hours through Site Manager via switchboard on: 0207 377 7000 Sreeman Andole sreeman.andole@bhrhospitals.nhs.uk Patrick Gompertz patrick.gompertz@nhs.net; Hugh Markus hmarkus@sgul.ac.uk; Rob Simister robert.simister@uclh.nhs.uk; 9