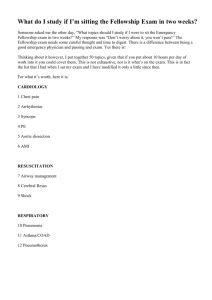
Paeds and neonatal resus fact sheet
advertisement

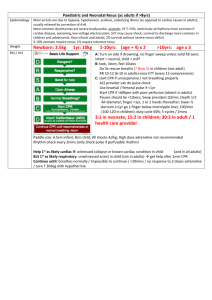
Paediatric and Neonatal Resus Epidemiology Most arrests are due to hypoxia, hypotension, acidosis, underlying illness; usually relieved by correction of A+B Most common dysrhythmias are severe bradycardia, asystole; VF 7-15%; ventricular arrhythmia more common if cardiac disease, poisoning, low voltage electrocution; SVT may cause shock 5-10% neonate require resus; 1% require intensive resus Weight Newborn: 3.5kg 1yr: 10kg 1-10yrs: (age + 4) x 2 >10yrs: age x 3 BLS / ALS A: Turn on side if drowning; no finger sweep unless solid FB seen; infant = neutral, child = sniff B: look, listen, feel 10secs 5x rescue breaths (?Now 2) in children (not adult) RR 10-12 (6-10 in adults) once ETT (every 15 compressions) C: start CPR if unresponsive / not breathing properly ALS provider can do pulse check Use brachial / femoral pulse if <1yr Start CPR if <60bpm with poor perfusion (absent in adults) Pauses should be <10secs; Swap providers Q2min; Depth 1/3 AP diameter; lower ½ sternum; 100-120/min (100 in adults); duty cycle 50%; 5 cycles / 2mins 3:1 in neonate 15:2 in children (30:2 if layperson or 1 person) 30:2 in adult at all times Paddle size: 4.5cm infant, 8cm child All shocks 4J/kg High dose adrenaline not recommended Rhythm check every 2mins (only check pulse if perfusable rhythm) Infant: 2 fingers <8yrs: 1 hand >8yrs: 2hands Adult: 2 hands Help 1st as likely cardiac if: witnessed collapse or known cardiac condition in child (and in all adults) st BLS 1 as likely respiratory: unwitnessed arrest in child (not in adults) get help after 1min CPR Continue until: breathes normally / impossible to continue A B Neutral position if infant, sniffing for children; measure guedel from centre of mouth to angle of mandible Use continuous ETCO2 monitoring BVM size: round mask 000-2 for infants / young child; shaped mask 3-5 for young child / adult Bag size: 250ml bag in prem 500ml with pressure valve in neonate / infant 1500ml in young / older child ETT: Mm: (age / 4) + 4 (uncuffed) + 3.5 (cuffed) Decr size by 0.5mm if severe croup / epiglottitis Length: (age / 2) + 12 (or 15) <28/40 Weight ETT width ETT length LMA Larngoscope 34-38/40 2.5mm 6.5-7cm 3.5mm 7-8cm 0 Miller 0 Miller >38/40 3.5kg 3.5-4mm 9cm 1 1 Miller 1yr 10kg 4mm 11cm 1.5-2 5yr 20kg 5mm 15cm 2-2.5 2 Miller 10yr 30kg 6mm 16-17cm 2.5-3 2 Mac . . . LMA: <5kg =1; 5-10kg = 1.5; 10-20kg = 2; 20-30kg = 2.5; 30-50kg = 3; 50-70kg = 4; 70-100kg = 5; >100kg = 6 Surgical: use cricothyroid puncture if <12yrs Ventilator: RR 20-30 (infant), RR 12-20 (child); TV 7-10ml/kg; PIP 15 (neonate), 25 (RDS), 20-25 (child); PEEP 3-5; I:E 1:2; FiO2 100% initially; have small air leak; NG mandatory IC catheter: neonate 8-12F Infant 14-20F Child 20-28F Adolescent 28-36F 4x ETT size Cricothyroidotomy cannula: adults 6mm, child 4mm, baby 3.5mm C BP = (age x 2) + 85 UO = 2ml/kg/hr in infant, 1ml/kg/hr in child IVA: use IO if can’t get IVL in <90 secs if critically ill child IO: insert in antmedial prox tibia 1 finger (2-3cm) beneath tibial tuberosity sup to med malleolus antlat distal femur 3cm above lateral condyle Will not be able to aspirate from tibia if >5yrs due to fatty marrow; not reliable for PO2, PCO2, LFT; can do Hb, but not FBC; can do pH; same onset of drugs; can give up to 10-15ml/min (125ml/min under pressure); flush all drugs with 10ml N saline; CI = OP, osteogenesis imperfecta, #, recent same bone IO, cellulitis, burns; complications rare (<1%; D E 2Y survey Post-resus mng Neonatal resus tibial #, growth retardation, compartment syndrome, cellulitis, OM, extravasation of fluid) Shock: 20ml/kg IVF if still shocked after 40ml/kg, use inotropes / blood products 4ml/kg PRBC incr Hb 1 10ml/kg plt incr plt 50 Fluids: avoid 5% dex (worsens neuro outcome, causes 2Y diuresis; hypoNa) Maintenance: use 0.45% saline + 2.5-5% dex in children Use 0.18% saline + 10% dex in neonates Shocks: unstable SVT: 0.5-1J/kg; pulsatile VT 0.5-2J/kg Check: LOC, pupils, posture, glu Beware T loss Head to toe B: aim SaO2 94-98% (PaO2 60-80mmHg); aim normocarbia C: maintain adequate perfusion D: therapeutic hypothermia (32-34deg) within 6hrs of cardiac arrest, and maintain up to 72hrs; avoid hypo/hyperG Epidemiology: required in 10% births; extensive resus in 1%; in >50% VLBW Causes: iNborn errors of metabolism, Electrolytes, OD, Seizures, Enteric, Cardiac, Recipe (formula etc…), Endocrine, Trauma, Sepsis Perinatal asphyxia: umbilical artery pH <7; 5min Apgar <4; neuro probs; MOF Apgar score: measured at 1 and 5mins; if <7 at 5mins, continue Q5minly until >7 @1min, correlates with acidosis and survival; @5mins correlates with neuro outcome 0 1 2 . Colour Blue/pale Acrocyanotic Completely pink HR Absent <100/min >100/min Reflex irritability No response Grimace Cry / active withdrawal Tone Limp Some flexion Active motion Respiration Absent Weak cry / hypoV Good, crying . If >8, no resus needed If 4-7 IPPV intubate if no improvement at 30secs If <4 intubate Fluid requirements in neonate: D1-2: 60-80ml/kg/day; D3-7: 100-150ml/kg/day; D 8-28: 120-180ml/kg/day Meconium aspiration: occurs in 12-20%, but aspiration rare; 25-50% require mechanical ventilation; 5% die; due to in utero fetal distress; if stained, suction as soon as head delivered do laryngoscopy and tracheal suction through ETT if: meconium staining + not vigorous (decr RR, decr tone, HR <100); repeat until no further meconium withdrawn; if still severely depressed after meconium cleared, start active resus Stimulate, dry, warm (if prem, may need plastic bag) A: open airway, suction mouth and nose; do Apgar after this B: O2 if SaO2 <95% Indications for IPPV via BVM: Apnoea for 30secs / gasping HR <100 Persistent central cyanosis despite 100% O2 Apgar 4-7 Use RR 30-40; give for 30-60secs; p 20mmHg (may need inflation p 30-35mmHg briefly, 20-25mmHg in prems) Indications for considering ETT: Not improving after 30sec IPPV Apgar <4 Prolonged resus (ie. Need for chest compressions) Prem Meconium aspiration ?congenital diaphragmatic hernia VLBW May need higher airway p and PEEP in prems C: Indications for chest compressions HR <60 after 30secs ventilatory support Use 3:1; 1/3 depth of chest; lower ½ sternum, 100/min, will have RR 30 For umbilical vein: insert catheter 10-12cm Drugs FB aspiration Prognosis Adrenaline: 10mcg/kg IV/IO (= 0.1ml/kg 1:10,000) 100mcg/kg ETT (= 0.1ml/kg 1:1000) Give after 2nd shock then every 2nd cycle Amiodarone: 5mg/kg after 3rd shock rpt dose after 5th shock Atropine: 0.02mg/kg (max 600mcg) IV Adenosine: 50mcg/kg 100mcg/kg 240mcg/kg (max 12mg) Sux: 3mg/kg (neonate) 2mg/kg (child) 1.5mg/kg (adult) Vec: 0.1mg/kg Diazepam: 0.25mg/kg IV Midaz: 0.15mg/kg IV Dextrose: 2-5ml/kg 10% dex HCO3: 1mmol/kg if pH <7.1 Naloxone: 0.1mg/kg IM/IV (give if maternal opiates <4hrs and resp depression after IPPV has restored normal HR and colour; CI if maternal narcotic addiction) Calcium: only if hyperK/Mg, hypoCa, Ca channel blocker OD Effective cough: cough Ineffective cough: unconscious CPR, direct laryngoscopy ASAP Conscious 5x back blows 5x chest thrusts (alternate with abdo thrusts in children) Finger sweep if visible material Outcomes from resus worse than in adults; 9% survival to discharge (<10% intact survival rate); if arrive to ED pulseless, death in 95%, all survivors have poor neuro outcome If CPR continued for 30mins with no ROSC, then continued resus is futile (may continue longer if arrest was witnessed and CPR immediately) Notes from: Dunn, Starship guidelines Normal vital signs: Age Term 3/12 6/12 1yrs 2yrs 4yrs 5-6yrs 8yrs 10yrs 12yrs 14yrs Weight 3.5kg 6kg 7.5kg 10kg 12kg 16kg 20kg 24kg 30kg 36kg 42kg HR 110 – 170 RR 40 – 60 30 – 50 30 – 40 100 – 160 20 – 30 80 – 130 20 70 – 115 16 70 – 110 60 – 100 SBP 50 - 90 60 - 90 65 - 90 70 – 100 75 – 110 80 – 110 85 – 120 90 – 120 tone tone