Post-operative sensitivity in glass
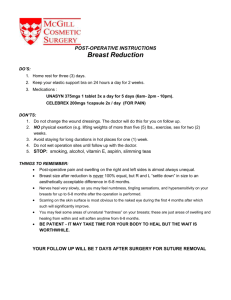
advertisement

C.E. Article #4-101 (1 credit/AGD code 253) Research Article Post-operative sensitivity in glass-ionomer versus adhesive resin-lined posterior composites ENOSAKHARE S. AKPATA,BCHD,MDSC,FDS & WALIDSADIQ,BDS,MS ABSTRACT: Purpose: To compare objective and subjective assessments of post-operative sensitivity when class 1 cavities, lined with glass-ionomer or adhesive bonding system, were restored with resin-based composite (RBC). Materials and Methods: Occlusal cavities on homologous contra-lateral posterior teeth in 44 male patients attending primary health centers in Riyadh, Saudi Arabia were restored with RBC after a cavity lining of either a light cured glass-ionomer cement (Vitrebond) or an adhesive bonding system (One-Step). Results: Cold response measurements 24 hrs, 7 days and 1 month post-operatively showed that the threshold of pulpal response was significantly lower (P< 0.05) in the restored teeth when the adhesive bonding system served as cavity liner. In addition, based on the patients' subjective assessments, the prevalence of mild or severe post-operative sensitivity was significantly higher (P< 0.05), 24 hrs and 7 days post-operatively, in the teeth with the adhesive bonding system as a cavity liner. After a post-operative period of 1 month, however, there was no significant difference (P> 0.05) between the prevalence of post-operative sensitivity when the restored teeth received a lining of either glass-ionomer or adhesive bonding system. (Am J Dent 2001;14: 34-38). CLINICAL SIGNIFICANCE: Post-operative sensitivity was more severe and prevalent in posterior teeth following the placement of occlusal resin-based composite restorations when the cavities were lined with an adhesive resin than when they received a glass-ionomer lining. CORRESPONDENCE: Prof. E.S. Akpata, Department of Restorative Dental Sciences, College of Dentistry, King Saud University, P.O.Box 60169, Riyadh, Saudi Arabia. Fax: 966 1 467 8548. E-mail: akpata@ksu.edu.sa Introduction Post-operative sensitivity following resin-based composite (RBC) restorations may result from microleakage, a condition that may be minimized by bonding the restoration to the cavity walls. RBC restorations can be bonded to both enamel and dentin using modern adhesive bonding systems. As these bonding systems are capable of sealing off the dentin tubules by forming resin tags firmly hybridized1 to the etched peritubular dentin, it was hypothesized that post-operative sensitivity would be minimal when adhesive bonding systems are used for lining cavities for RBC restorations. Similarly, glassionomer cement is known to bond to calcified dental tissues as well as to RBCs3. When used as a cavity liner in teeth restored with RBC, glass-ionomer cement has the potential to minimize microleakage and therefore post-operative sensitivity. Chan & Swift4 studied microleakage following RBC restorations of cavities lined with three adhesive bonding systems: All Bond 2,a Gluma 2000,b and Scotchbond Multipurpose.0 They observed that microleakage was less in the group of teeth that received the adhesive linings, when compared with the unlined control group. Nevertheless, Yap et af reported that microleakage was significantly less when cavities restored with RBC were lined with glass-ionomer cement than when they received an adhesive lining of Scotchbond Multipurpose. Using silver nitrate, Sano et af studied nanoleakage in the hybrid layer in cavities lined with dentin bonding systems (Clearfil Liner Bond Systemd and All Bond-2). Both systems demonstrated silver nitrate accumulation beneath the hybrid layer, suggesting that irritants might penetrate the hybrid layer even when cavities were lined with dentin bonding agents. Browning et af compared post-operative sensitivity from amalgam restorations in cavities that received an adhesive liner, OptiBond6 or conventional liner and base. The teeth that received an adhesive liner were not less sensitive to cold stimuli than those that received conventional liner and base. However, reports are scarce on controlled clinical studies comparing post-operative sensitivity when cavities for posterior RBC restorations are lined with an adhesive bonding system or a conventional liner. This study, therefore, compared post-operative sensitivity following Class I posterior RBC restorations in teeth that received a cavity lining of either glass-ionomer cement or adhesive bonding system. Materials and Methods Selection of patients and informed consent - Approval for this study was obtained from the College of Dentistry Research Center of the King Saud University, Riyadh. The nature of the research was explained to the patients selected from primary health centers in Riyadh, Saudi Arabia. After the explanation, the patients gave their consent and agreed to attend follow-up appointments for at least 1 month. Forty-four male patients aged 16-52 yrs with homologous contra-lateral posterior teeth having occlusal caries were selected for the study. The patients were free of orofacial pain, including toothache. Selection and isolation of teeth - The homologous contra-lateral posterior teeth selected for the study were neither tender to percussion nor did they show any sign of periapical radiolucency. If maxillary premolars or molars were selected, both right and left teeth were restored at the same visit. On the other hand, if mandibular teeth were selected for the study, one tooth was restored at each visit, to avoid giving two inferior dental blocks simultaneously. The teeth selected had small or moderately large carious lesions. The bucco-lingual dimension of each carious cavity was less than half the intercuspal width. \ American Journal of Dentistry, Vol. 14, No. 1, February, 2001 The experimental teeth were isolated with rubber dam throughout the operative procedures. A detailed description of the operative procedures was given to four general dental practitioners who carried out the clinical work. Cavity preparation - After administering local anesthetic, an occlusal cavity was prepared with a high-speed handpiece using a number 330 pear-shaped tungsten carbide bur, cooled with a water spray. Residual caries was removed with the largest possible spoon excavator. If there was pulp exposure or pink dentin was visible, the tooth was excluded from the sample. The enamel walls were smoothened with a water-cooled cylindrical finishing bur at slow speed. The cavosur-face angle of the prepared cavity was approximately 90°. The cavity was cleaned with a water spray from the triple syringe of the dental unit. The depth of the prepared cavity was measured against the mesial and distal marginal ridges, using a graduated periodontal probe. In addition, the width of the cavity was recorded as a proportion of the intercuspal width. For each patient, the prepared cavity on one of the selected teeth was lined with glass-ionomer and the contra-lateral homologous tooth with an adhesive bonding system. Placement of glass-ionomer lining and etching of enamel cavity wall - One scoop of light-cured glass-ionomer liner (Vitrebond0) powder was mixed with one drop of the liquid on a mixing pad. Using the applicator supplied by the manufacturers, a creamy mix of the liner was spread on the pulpal floor and dentin axial walls of the cavity. The lining was then light-cured for 20 s. The enamel walls of the cavity were etched with 37% phosphoric acid for 20 s, washed with water for 20 s and then dried for 20 s. The etching was repeated for 20 s if the enamel was not frosty white. Cavity lining with bonding system - The enamel and dentin walls on the contra-lateral homologous tooth were etched with 32% phosphoric acid (Uni-etcha) for 15 s, washed, dried, and then lined with three coats of One-Step3 according to the manufacturer's instructions. There was randomization in the selection of the right and left teeth for the adhesive or glassionomer lining. Restoration with RBC - The lined cavity was restored with three pie-shaped wedges of heavily filled hybrid RBC (BisFil P a). The first layer was placed on the buccal wall and then extended diagonally to the pulpal floor. The RBC was cured from the buccal direction for 60 s. The procedure was repeated on the lingual wall, again curing through the lingual enamel for 60 s. Lastly, the RBC was placed in the mid-portion of the cavity and cured from the occlusal direction.8 Occlusion was adjusted with a football-shaped diamond point. The restoration was finally polished with aluminum oxide polishing paste. Evaluation of post-operative sensitivity Objective assessment of post-operative sensitivity - Prior to cavity preparation, an ice stick of standard diameter and length, prepared by freezing water in a local anesthetic cartridge, was placed against the buccal surface of the experimental tooth to determine how long it took for the patient to feel cold sensation. The time was measured, in seconds, with a stopwatch, and this was recorded as the baseline cold re- Post-operative sensitivity 35 Table 1. Frequency (%) of experimental teeth. Left Right Molars Premolars Premolars Total 12(13.6) Maxillary Mandibular 16(18.2) Total 11(12.5) 5 (5.7) Molars 28(31.8) 16(18.2) 28(31.8) 46 42 11(12.5) 5 (5.7) 12(13.6) 16(18.2) 16(18.2) 88 Table 2. Intercuspal widths of the Class I experimental cavities. One-Step Vitrebond Total Premolars Molars 10 8 5 12 1 5 0 3 9 9 7 9 0 9 0 1 32 56 Total 18 17 6 3 18 16 9 1 88 sponse measurement (CRM). At the recall appointment 24 hrs, 7 days and 30 days after the restoration, the CRM was repeated. The measurement of CRM at the recall visits was by another dentist who was unaware of the lining that the experimental teeth had received. Subjective assessment - of post-operative sensitivity - At the recall visits 24 hrs, 7 days and 30 days post-operatively, each of the patient's subjective assessment of post-operative sensitivity was recorded. At each of these appointments, the patient classified the pain from each of the restored teeth into none, moderate or severe; accordingly, the patient's assessment was scored on a scale of 1-3, respectively. Statistical analysis - Chi-square test was used to determine the statistical significance of the difference between the widths and depths of the cavities prepared on the homologous contra-lateral teeth. In addition, paired Mest and Wilcoxon matched pairs rank sum test were used to compare the objective and subjective assessments of post-operative sensitivity from teeth that received a lining of One Step or Vitrebond, respectively. Results Patients and experimental teeth - The mean age of the 44 patients who participated in the study was 27.9 yrs (range 16-52 yrs) and about 70% of them were aged between 16-30 yrs. Of the 88 experimental teeth, 46 were in the maxilla, while molars accounted for about 64% of the selected teeth (Table 1). Cavity width and depth - Most of the prepared cavities were either about a quarter or a third the intercuspal width of the posterior teeth: 40% of the cavities lined with One-Step or Vitrebond were about a quarter the inter-cuspal width, while 36-38% were about a third the inter-cuspal width. Only about 27% of the cavities was more than half the intercuspal width (Table 2). A Chi-square test showed that there was no statistically significant difference between the widths of the cavities that received a lining of glass-ionomer or adhesive bonding system. About 30% of the prepared cavities were 0.5 mm into dentin while approximately 40% extended 1 mm beyond the den-tinenamel junction (Table 3). Again, a Chi-square test showed that there was no statistically significant difference between the depth of the cavities lined with the glass-ionomer or adhesive bonding system (P> 0.05). 36 Akpata & Sadiq American Journal of Dentistry, Vol. 14, No. 1, February, 2001 American Journal of Dentistry, Vol. 14, No. I, February, 2001 post-operative period, however, there was no significant difference in the prevalence of post-operative sensitivity in the teeth lined with the adhesive bonding system or glass-ionomer (P> 0.05). Discussion Class I occlusal cavities were selected for this study because their preparation is relatively easy and involves less variability than compound cavities. Thus there was no statistically significant difference between the depth and width of the cavities lined with the glass-ionomer or the adhesive bonding system. Furthermore, exclusion of cases showing pink dentin at the pulpal floor of the prepared cavities minimized the confounding effect of pre- and post-operative pulp disease on the prevalence and severity of post-operative sensitivity. As there was equal distribution of cases with centric occlusal contact at the restoration margin among the teeth that received a lining of the adhesive bonding system or glass-ionomer, it is unlikely that occlusal breakdown of restoration margins had a significant effect on the results obtained in this study. Polymerization shrinkage stresses contribute to postoperative sensitivity following RBC restoration by causing coronal deformation and micro-fracture.9 These stresses may be reduced by incremental filling technique10 and by curing the RBC indirectly through the cusps; thus, polymerization shrinkage, directed towards the source of curing light,11 is towards the axial cavity walls. Although some investigators question the value of these techniques,12'13 in the present study precautionary measures of placing the Class I RBC restorations incrementally and curing from the buccal and lingual directions were taken.8 The fact that there was no significant difference between the mean baseline CRM obtained for the contra-lateral homologous teeth indicates that the measurements with the standardized ice stick was reasonably accurate. The relatively large standard deviations may be due to biological variation and sub-clinical histopathological pulpal changes in the carious experimental teeth. The significantly higher severity and prevalence of postoperative sensitivity in teeth lined with the adhesive bonding system was rather surprising, in view of the relatively high resinous content of One-Step. A number of factors may have contributed to this finding. The use of the glass-ionomer liner does not involve acid etching the cavity dentin walls. Consequently, the cement is bonded to both the smear layer and the underlying dentin wall to block the dentin tubules, and perhaps controlling post-operative sensitivity. In contrast, the cavity dentin walls were etched with 32% phosphoric acid for 15 s before the application of the adhesive bonding system. This is capable of removing the smear plugs and opening (funneling) the ends of the dentinal tubules.14 The open dentin tubules could then cause post-operative sensitivity by permitting hydraulic fluid shift due to thermal stimulation or flexion of the RBC restoration under masticatory load. Additionally, the acid, on account of its osmotic pressure, might cause dentin fluid movement, resulting in post-operative sensitivity.15 However, Cox et a/16 reported the biocompatibility of nine adhesive systems with exposed and non-exposed dental pulps in monkeys, while Hebling et a/17 demonstrated more severe pulpal inflammatory response to adhesive cavity lining of All- Post-operative sensitivity 37 Bond 2 than to calcium hydroxide in deep cavities in human teeth. The effect of species difference on these contrasting reports is, however, uncertain. The bond mediated by One-Step is mainly micro-mechanical18 rather than chemical. This makes microleakage, and therefore hydrodynamic fluid shift in the dentin tubules, more likely in cavities with the adhesive lining than those lined with glass-ionomer bonded chemically to the cavity walls. Besides, it has been demonstrated that a demineralized porous zone, not penetrated by adhesive resin, may exist beneath the hybrid layer.6 This zone may prevent total sealing of the dentin tubules, resulting in post-operative sensitivity from cavities with adhesive lining. It would therefore appear desirable to develop bonding systems with micro-mechanical and enhanced chemical adhesion, to provide better sealing of dentin tubules. It is possible that the application of three coats of OneStep recommended by the manufacturer is insufficient to provide an uninterrupted layer of the dentin-bonding agent. Future research should therefore investigate the relationship between post-operative sensitivity and the number of coats (up to 6) of the bonding system. When there is polymerization shrinkage of RBC in a cavity lined with an adhesive system, the gap formation is usually between the RBC and the hybrid layer.19 If there is discontinuity in the coating of the cavity wall by the bonding system or micro-porous zone beneath the hybrid layer, however, hydrodynamic fluid shift or bacterial toxins penetrating the dentin tubules could cause post-operative sensitivity. In contrast, on account of its relatively high film thickness and low cohesive bond strength,20 a glass-ionomer lining is likely to suffer cohesive bond failure when there is polymerization shrinkage of the RBC restoration. Under this situation, the glass-ionomer cement still bonded chemically to the cavity dentin wall, would block the dentinal tubules, therefore controlling postoperative sensitivity. Another possible explanation for the difference in post-operative sensitivity due to the two cavity linings could be that the glass-ionomer, on account of its more plastic behavior, provided more stress relief to the RBC restoration and therefore less cavity deformation. Lining the entire pulpal and axial cavity walls with Vitrebond in half of the experimental teeth in this study facilitated comparison of post-operative sensitivity between the teeth in which the cavities were lined with either glass-ionomer or One-Step. This experimental model may be utilized in the evaluation of post-operative sensitivity following the use of other adhesive bonding systems. Nevertheless, as glass-ionomer liner or base is more often applied selectively to deep areas of prepared cavities in clinical practice, future studies should compare post-operative sensitivity from teeth with selective glass-ionomer lining and those with adhesive lining following the total etch technique. a. b. c. d. e. Bisco, Schaumburg, IL, USA. Heraeus Kulzer, Dormagen, Germany. 3M Dental Products, St. Paul, MN, USA. J. Morita, Osaka, Japan. Kerr Corp., Orange, CA, USA. Acknowledgements: We are grateful to Drs. A. Al-Rabiah, F. Al-Rossais, A. Al-Shayea and H. Al-Robiaan for their clinical input to this investigation. American Journal of Dentistry, Vol. 14, No. 1, February, 2001 38 Akpata & Sadiq This project was registered at the King Saud University College of Dentistry Research Center, NF 1352. Dr. Akpata is Professor, Department of Restorative Dental Sciences; Dr. Sadiq is Assistant Professor, Department of Prosthetic Dental Sciences, College of Dentistry, King Saud University, Riyadh, Saudi Arabia. References Nakabayashi N. Bonding of restorative materials to dentine: The present status in Japan. Int Dent J 1985; 35: 145-154. Kent BE, Lewis BG, Wilson AD. The properties of glass-ionomer cement. BrDentJ 1973; 135:322-326. McLean JW, Powis DR, Prosser HJ, et al. The use of glass-ionomer cement in bonding composite resin to dentine. Br Dent J 1985;158:410-414. Chan KC, Swift EJ. Marginal seal of new-generation dental bonding agents. J Prosthet Dent 1994;72:420-423. Yap AUJ, Mok BYY, Pearson G. An in vitro microleakage study of "bonded base" restorative technique. J Oral Rehabil 1997; 24: 230-236. Sano H, Shono T, Takatsu T, et al. Micro-porous dentin zone beneath resin impregnated layer. Oper Dent 1994; 19: 59-64. 7. Browning WD, Johnson WW, Gregory PN. Post-operative pain following bonded amalgam restorations. Oper Dent 1997; 22: 66-71. 8. Dale BG, Ascheim KW. Esthetic dentistry: A clinical approach to techniques and materials. Malvern: Lea & Febiger, 1993; 44. 9. Bowen RL, Nemoto K Rapson JE. Adhesive bonding of various materials to hard tooth tissues: forces developing in composite materials during hardening. J Am Dent Assoc 1983; 106:475-477. 10. Opdam NJM, Feilzer AJ, Roeters JJM. Class I occlusal resin restorations: In vivo post-operative sensitivity, wall adaptation, and micro-leakage. Am J De n t\ 998; 11:229-234. 11. Lutz F, Krejci I, Luescher B, et al. Improved proximal margin adaptation of class 11 composite resin restorations by use of light reflecting wedges. Quintessence Int 1986; 17: 659-664. 12. Versluis A, Douglas WH, Cross M, et al. Does an incremental filling technique reduce polymerization shrinkage stresses? J Dent Res 1996; 75: 871-878. 13. Versluis A, Tantbirojn D, Douglas WH. Do dental composites always shrink towards the light? J Dent Res 1998; 77: 1435-1445. 14. Pashley DH, Homer JA, Brewer PD. Interactions of conditioners on dentine surface. Oper Dent 1992; (Suppl.) 5:137-150. 15. Pashley DH. The effect of acid etching on the pulp-dentin complex. Oper Dent 1992; 17:229-242. 16. Cox CF, Hafez AA, Akimoto N, et al. Biocompatibility of primer, adhesive resin and resin composite systems on non-exposed and exposed pulps of non-human primate teeth. Am J Dent 1998; 11: S58-S63. 17. Hebling J, Giro EMA, Costa CAS. Human pulp response after an adhesive system application in deep cavities. J Dent 1999; 27: 557-564. 18. Kanca J. One-step bond strength to enamel and dentin. Am J Dent 1997; 10:5-8. 19. Asmussen E, Hansen K. Dentine bonding systems. In: Vanherle G, Degrange M, Willems G. State of the art in direct posterior filling materials and dentine bonding. Proceedings on the International Symposium. EuroDisney, Pans, March 23-25, 1993;33-47. 20. Lin A, Mclntyre NS, Davidson RD. Studies on adhesion of glass-ionomer cements to dentin. J Dent Res 1992;71: 1836-1841. Authors: Please note: As of March 15, 2001, the address for the Editorial Office of the American Journal of Dentistry for submission of manuscripts has changed. Please send all manuscript submissions to: Dr. Franklin Garcia-Godoy Biomaterials Research School of Dental Medicine Tufts University One Kneeland Street Boston, MA 02111