Kidder County Community Health Center Pediatric Health
advertisement

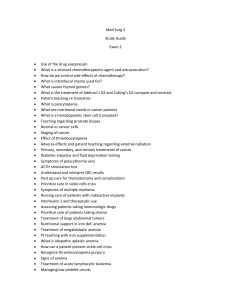
Kidder County Community Health Center Pediatric Health Questionnaire 2-18 years. Patient Name:_______________________________________________Date of Birth:_______________ Do you have any allergies? If yes, please list: ________________________________________________ Drug store preference: __________________________________________________________________ Does this child take any medications, vitamins or supplements daily? If yes, please list below: Medication Dose Frequency Pediatrician/Family Doctor:______________________________________________________________ Date and Purpose of last doctor visit:______________________________________________________ Date of last Well Child Visit:______________________________________________________________ Immunization Dates: HEP B_________ OPV_________ MMR__________ DTP___________ HIB__________ VAR___________ Date of Childhood Disease: Measles___________ Chicken Pox___________ Whooping Cough__________Mumps_________ Other__________________________________ Has this child been treated for any emergency? Please circle: Yes No Describe:_____________________________________________________________________________ _____________________________________________________________________________________ Has this child had any surgeries? Please Circle: Yes No Describe:_____________________________________________________________________________ _____________________________________________________________________________________ Medical History: Please circle Chicken Pox Asthma Hepatitis Eczema Heart Murmur Irregular Pulse PE Tubes (ear tubes) Diabetes Fainting Spell Psychiatric Problems Anemia Ulcers Hyperactivity Cancer Sickle Cell Anemia Blood transfusion Appendix removed Bed wetting Constipation Diarrhea Muscle jerking Chronic ear aches Tuberculosis Walking Problem Please list any other pertinent medical history this child may have: Pneumonia Serious allergic reactions Cleft palate High blood pressure Downs syndrome Asperger’s Syndrome Rheumatic Fever Tonsils removed Paralysis Hearing trouble Ruptures/Hernias Broken Bones Family History: Please circle any family history listed below. Asthma Rheumatic Fever Pneumonia Stroke Chronic Lung Disease High Blood Pressure Tuberculosis Diabetes Congestive Heart Failure Atrial Fibrillation High Cholesterol Heart Murmur Hypothyroidism Hyperthyroidism Kidney Infections Kidney Stones Chrohn’s Disease Ulcerative Colitis Hepatitis Liver Disease/Problems Psychiatric Illnesses Anxiety Bleeding Disorders Seizures Migraines Tension headaches Osteoporosis Chronic neck and back pain Macular Degeneration Glaucoma Leukemia Juvenile Arthritis Acid Reflux Gastro esophageal Reflux Disease Hiatal Hernia Gall Bladder Disease Irritable Bowel Syndrome Heart Attack Cancer: Type:________________ Ulcers: Location:______________ Diverticulitis Depression Anemia Epilepsy Arthritis: Location:____________ Carpal Tunnel Osteopenia Sickle Cell Anemia Social History: Who is the primary caregiver for this child?_________________________________________________ Does this child attend day care? If yes, where?_______________________________________________ Is this child exposed to second hand smoke?_________________________________________________ Number of children in the home:__________________________________________________________ Has this child ever been exposed to lead?___________________________________________________ What does this child diet consist of?________________________________________________________ Does this child ride in a car seat?__________________________________________________________ Is there anything else we should know about this child?________________________________________________________________________________ _____________________________________________________________________________________ I certify that the information on this form is true to the best of my knowledge. Print childs/patients name:______________________________________________________ Signature of parent or legal guardian:______________________________________________