Tulane Longitudinal Curriculum
advertisement

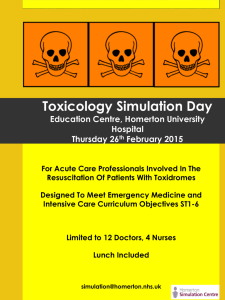
LONGITUDINAL EM CURRICULUM - TU Emergency Medicine (EM) as a discipline is a critical component of a well-rounded undergraduate medical education. The LCME recognizes that "educational opportunities must be available in multidisciplinary content areas, such as emergency medicine ..." (ED-17) Furthermore, EM provides a unique and broad setting to develop and evaluate the core competencies set forth by the ACGME as central to the proper education and training of physicians. Recognizing that EM is best thought of and taught as a longitudinal curriculum throughout all years of undergraduate medical school, other academicians have proposed goals of EM student education: acquisition of basic life support (BLS) skills and basic procedural skills differentiation and treatment of common acute problems assessment of the undifferentiated patient (Burdick et al., Acad Emerg Med 1998) These core tenets can be taught beginning in the first year of medical school, and proceeding in depth and breadth throughout the student's career. In detail, Acquisition of BLS skills and basic procedure skills: Undergraduate learners should be able to recognize the patient with a serious, life-threatening condition that requires immediate attention understand how to prioritize attention to and care of those patients with the most serious conditions (triage) take the first steps necessary to stabilize a patient or save a life, specifically non-invasive airway techiniques (opening maneuvers) respiratory support (BVM) circulatory assistance (external hemorrhage control, fluids) recognize serious neurologic insults and poisonings Differentiation and treatment of common acute problems: Undergraduate learners should have basic knowledge of conditions that commonly affect the general public, by organ system and disease process, their diagnosis and management, to include: chest pain respiratory infections/colds headache minor trauma basic orthopedic complaints (back pain, fractures, sprains) abdominal pain/nausea & vomiting common infections (absesses/cellulitis, UTI, pharyngitis, otitis media etc) dermatologic complaints (rashes/burns) eye complaints gynecologic conditions Assessment of the undifferentiated patient: Undergraduate learners should: be able to provide a broad differential of an acutely ill patient, with appropriate focus on the most common diagnoses given the particular clinical situation appropriately target testing, treatment & management of the undifferentiated patient and follow the case to resolution and disposition Suggested methodologies and content areas by year of training have been proposed and are detailed below. First Year Medical Students Focus: first aid/BLS exposure to/first aid training in: airway obstruction, altered mental status, shock, simple burns/lacerations, extremity injuries introduction to history taking/physical exam, counseling & communication skills Objectives: perform mouth-to-mouth/mask ventilation/chest compressions on mannequin understand how/when to activate 911/emergency response system provide first aid for choking perform simple airway opening maneuvers (chin lift/jaw thrust) take a pulse and blood pressure correctly understand & apply initial pain control measures, dressings and splints for simple burns & extremity injuries Means of Implementation: ED/EMS observation period BLS instruction, reading materials, and simulation simulation labs for basic and advanced procedural techniques Second Year Medical Students Focus: basic concepts of emergency care exposure to toxicology, pharmacology, physiology and pathology ED-set case-based learning to demonstrate practical applications of preclinical tenets instruction in simple procedural skills (IV, venipuncture, Foley catheters, etc) increase proficiency in history taking and physical exam skills Objectives: be able to perform a basic, focused history and physical exam on an undifferentiated patient be able to perform simple airway techniques (BVM, oxygen application) and basic procedures (IV, venipuncture) Means of Implementation: students will be exposed to basic history & physical exam skills through the SPM course, and the interviewing of patients in the ED is encouraged basic skills labs for simple techniques Third Year Medical Students Focus: become familiar with the course of disease from ED through inpatient wards/outpatient clinics become competent with basic clinical procedures become competent with basic history taking/physical exam Objectives: perform a targeted history & physical of the undifferentiated patient, and generate a differential diagnosis addressing possible urgent and emergent conditions understand the usual course of care/disposition for patients presenting with common medical conditions perform common procedures and techniques: airway (including endotracheal intubation) oxygenation (nasal cannula, mask, BVM, pulse oximetry, ABG) venipuncture/IV access/fluid administration NG tube, Foley catheterization wound care Means of Implementation: simulation labs/didactic lectures dealing with emergency patients exposure to the ED on consulting services (Medicine, Surgery, OB) Fourth Year Medical Students Focus: evaluation of undifferentiated patients in the ED setting apply clinical knowledge to "hands-on," real-time patient settings emphasis on clinical reasoning skills/application of textbook learning advanced cardiac life support and resuscitation skills elective opportunities: toxicology, ultrasound, pediatrics, critical care, research understand the roles of the health care team and how to function within one Objectives: perform a focused history and physical exam, develop a broad differential diagnosis, provide a treatment and management plan for undifferentiated patients in the ED demonstrate competence in basic resuscitation skills as well as more advanced techniques (endotracheal intubation, central venous access, defibrillation, administration of advanced life support medications, trauma resuscitations, ultrasonography) understand the impact of health care systems, resource allocation, cultural differences and access to care for patients presenting to the ED understand situations that are unique to EM: acute critical illness; acute intoxications; relationships with prehospital providers; disaster medicine/mass casualty events; death notifications for sudden unexplained death; environmental exposures; time-constrained patient care and decision making Means of Implementation: clinical rotation in the University Hospital ED direct faculty/resident examination of students to assess history and physical skills and patient management complementary didactic lectures, online modules, simulation and procedure labs learn time management/efficiency skills to improve ability to manage multiple patients at once formal examination to assess acquisition of knowledge of emergency care and disease processes Sources: Burdick WP et al, Acad Emerg Med 1998; Manthey DE et al, Annals Emerg Med 2006; DeBehnke DJ et al, Acad Emerg Med 1998; Hobgood C Isr J Emerg Med 2009. FIRST YEAR MEDICAL STUDENTS T1 EMERGENCY MEDICINE ELECTIVE First or second year medical students may elect to spend an observership period in the University Hospital ED. During this rotation, the student will: observe EM practice, emergency medical systems (EMS), and the application of basic and advanced life support skills in a real-time setting. observe practical history taking and physical exam skills in the acute undifferentiated patient participate in a simulation and procedure lab with other EM students write a brief (< 500 word) essay on their experience in the ED and how it informs their medical career goals Opportunities listed above are complementary to the standard first year curriculum, which should include: BLS instruction/certification (didactics/simulation lab) introduction to history & physical exam (lectures/standardized patients/small groups) SECOND YEAR MEDICAL STUDENTS 1. T2 EMERGENCY MEDICINE ELECTIVE First or second year medical students may elect to spend an observership period in the University Hospital ED. During this rotation, the student will: observe EM practice, emergency medical systems (EMS), and the application of basic and advanced life support skills in a real-time setting. observe practical history taking and physical exam skills in the acute undifferentiated patient participate in a simulation and procedure lab with other EM students write a brief (< 500 word) essay on their experience in the ED and how it informs their medical career goals 2. ED observation volunteer opportunities Through the Emergency Medicine Interest Group (EMIG), students may elect to do brief observation periods in the ED to further their understanding of the practice of EM as well as resuscitation techniques, critical illness management, and procedures Opportunities listed above are complementary to the standard second year curriculum, which should include: Instruction in physiology of common disease processes (didactics) further introduction and practice of history & physical exam (small groups/standardized patients/lectures) simulation/procedure labs for basic skills THIRD/FOURTH YEAR MEDICAL STUDENTS Since Tulane allows students to do core rotations in either the third or fourth year, the experience provided can be done either as a junior or senior clinical student. CLINICAL ROTATION IN EMERGENCY MEDICINE Students planning to pursue any specialty can benefit from an in-depth exposure to EM, as our specialty has a broad application to many aspects of medicine. During this rotation, students will: 1. work 6 clinical shifts* in the ED (Main ED and Urgent Care/Fast Track). Student schedules will mirror those of rotating interns, as senior students are considered "acting interns" or "subinterns" on their EM rotation. Students will gain experience with managing multiple patient workups at once, and learn efficiency and appropriate management skills. 2. be responsible for full evaluation and care of patients from start to finish, including: full history and physical exam; development of treatment and management plans under supervision of EM residents and faculty; assistance with or supervised performance of any necessary resuscitation or procedures on their patients. 3. participate in team resuscitation efforts for acute, critically ill trauma and medical patients. 4. be responsible for reading provided material on EM core topics, as well as attending didactic lectures, simulation and procedure labs, and completing selected online learning modules. 5. receive feedback on history and physical exam skills. 6. take an end of rotation exam designed to assess their acquisition and understanding of core EM topics. 7. participate in a team approach to patient care. 8. develop an understanding of health care system delivery, resource allocation, cultural diversity and access issues as they pertain to ED patients. * Students are required to do a two-week EM rotation during their clinical years; this experience is pass/fail only and includes the requirements above. For the EM-interested student, or those wishing a more in-depth rotation, a four-week clerkship is available with increased clinical shift and examination requirements, and is graded on an honors/high pass/pass/fail scale. This rotation should provide the student with the exposure to all of the core competencies required of a medical student rotation, namely: Patient care: 1,2,3,7 TU SOM Goals & Objectives: S3-4; S9;S16-22; S24-25, K14 Medical knowledge: 2,4,5,6 TU SOM Goals & Objectives: K2, K4; S1; K11-13;K16; S13-14 Practice-based learning: 4 TU SOM Goals & Objectives: K6;K16;S7; S23 Interpersonal/communication skills: 2,7 TU SOM Goals & Objectives:AB9; AB14-7;S2;S27;S29-30;S32;K20 Professionalism: 7,8 TU SOM Goals & Objectives: AB1-7;AB10;AB12 System-based practice: 8 TU SOM Goals & Objectives: K10;AB8;AB14;AB18;AB20 Opportunities listed above are complementary to the standard third/fourth year curriculum, which should include: exposure to the ED on consulting services simulation and procedure labs dealing with acute critical illness on other services ACLS certification (didactics/simulation lab)