docx 148KB - Mental Health Tribunal
advertisement
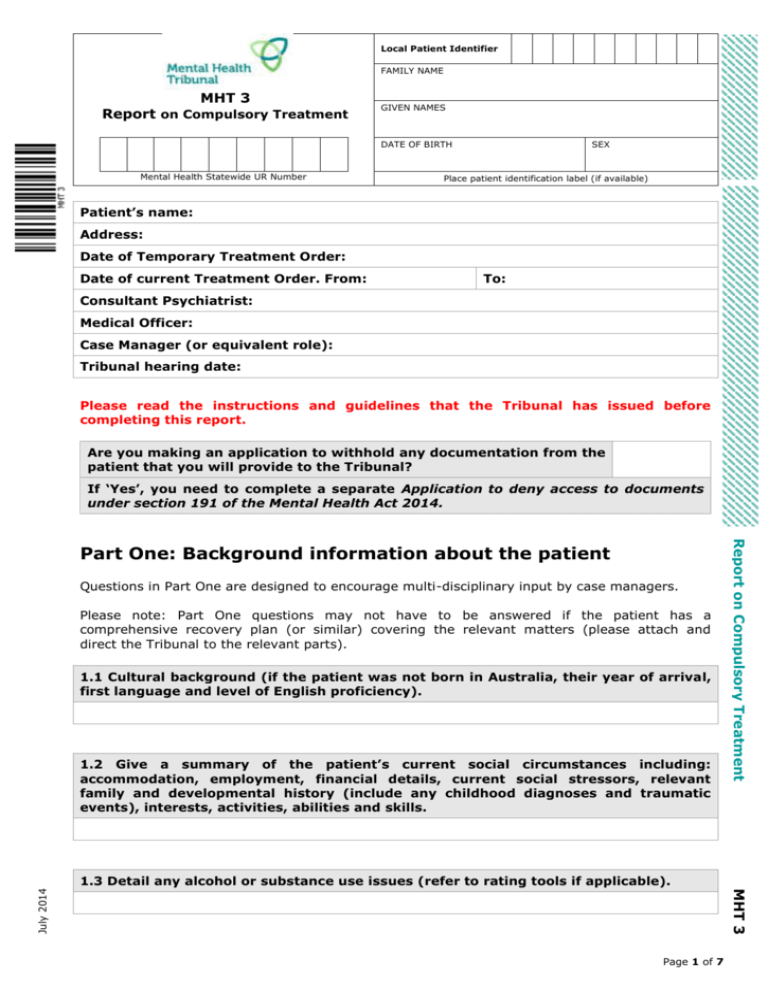
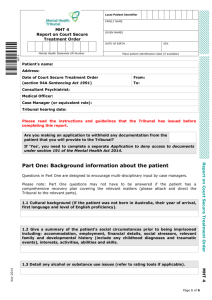
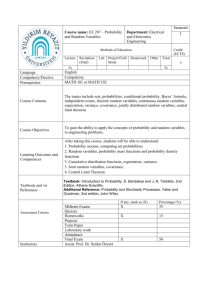
Local Patient Identifier FAMILY NAME MHT 3 Report on Compulsory Treatment GIVEN NAMES DATE OF BIRTH Mental Health Statewide UR Number SEX Place patient identification label (if available) Patient’s name: Address: Date of Temporary Treatment Order: Date of current Treatment Order. From: To: Consultant Psychiatrist: Medical Officer: Case Manager (or equivalent role): Tribunal hearing date: Please read the instructions and guidelines that the Tribunal has issued before completing this report. Are you making an application to withhold any documentation from the patient that you will provide to the Tribunal? If ‘Yes’, you need to complete a separate Application to deny access to documents under section 191 of the Mental Health Act 2014. Questions in Part One are designed to encourage multi-disciplinary input by case managers. Please note: Part One questions may not have to be answered if the patient has a comprehensive recovery plan (or similar) covering the relevant matters (please attach and direct the Tribunal to the relevant parts). 1.1 Cultural background (if the patient was not born in Australia, their year of arrival, first language and level of English proficiency). 1.2 Give a summary of the patient’s current social circumstances including: accommodation, employment, financial details, current social stressors, relevant family and developmental history (include any childhood diagnoses and traumatic events), interests, activities, abilities and skills. Report on Compulsory Treatment Part One: Background information about the patient MHT 3 July 2014 1.3 Detail any alcohol or substance use issues (refer to rating tools if applicable). Page 1 of 7 Local Patient Identifier FAMILY NAME MHT 3 Report on Compulsory Treatment GIVEN NAMES DATE OF BIRTH Mental Health Statewide UR Number SEX Place patient identification label (if available) 1.4 Other relevant medical issues or relevant history. 1.5 List all current medications (psychotropic and general). 1.6 Relevant legal matters (such as VCAT orders, court orders and police/forensic matters. List historic and current matters). 1.7 How long has the current treating team been treating the patient? Part Two: Criteria for Compulsory Treatment Section 5(a) – the person has mental illness. Section 4 defines mental illness as a medical condition that is characterised by a significant disturbance of thought, mood, perception or memory. 2.1 What is the patient’s current diagnosis? 2.2 Please give details as to the information regarding this diagnosis that has been communicated to the patient. Report on Compulsory Treatment Under the Mental Health Act 2014 a person can only be treated as a compulsory patient if they satisfy all of the criteria in section 5. MHT 3 July 2014 2.3 Describe the patient’s psychiatric history (in chronological order). Consider the pattern of the patient’s illness, pre-morbid mental state and functioning, initial presentation/first episode, severity of relapse and precipitants, recovery and response to treatment, disability. Page 2 of 7 Local Patient Identifier FAMILY NAME MHT 3 Report on Compulsory Treatment GIVEN NAMES DATE OF BIRTH Mental Health Statewide UR Number SEX Place patient identification label (if available) 2.4 If the patient is an inpatient, detail the circumstances and referral leading to the patient’s current admission. 2.5 Does the patient have a significant disturbance of thought (form or content)? Does the patient have a significant disturbance of mood? Does the patient have a significant disturbance of perception? Does the patient have a significant disturbance of memory? 2.6 If you answered ‘Yes’ to any of the questions at 2.5, please provide details. Refer to current mental state, current symptoms and symptoms that have responded to treatment. You must include a summary of the evidence being relied upon (e.g. a description of the content of delusional thoughts or the nature of auditory hallucinations and when it was observed and/or any supporting assessments). 2.7 Does the patient need immediate treatment to prevent serious deterioration in their mental health? Does the patient need immediate treatment to prevent serious deterioration in their physical health? Does the patient need immediate treatment to prevent serious harm to himself/herself? Does the patient need immediate treatment to prevent serious harm to another person? 2.9 Have these matters been discussed with the patient? What views has the patient expressed? Page 3 of 7 MHT 3 July 2014 2.8 If you answered ‘Yes’ to any of the questions at 2.7, please provide details and the evidence on which this assessment is based, including the source of that evidence and how recently it was observed or occurred. Report on Compulsory Treatment Section 5(b) – because the person has mental illness, the person needs immediate treatment to prevent serious deterioration in the person's mental or physical health or serious harm to the person or to another person. Local Patient Identifier FAMILY NAME MHT 3 Report on Compulsory Treatment GIVEN NAMES DATE OF BIRTH Mental Health Statewide UR Number SEX Place patient identification label (if available) Section 5(c) – the immediate treatment will be provided to the person if the person is subject to a Treatment Order. Section 6 defines treatment as things done to the person in the course of the exercise of professional skills to remedy the mental illness or to alleviate the symptoms and reduce the ill effects of the mental illness. 2.10 What immediate treatment does the patient require? 2.11 How does the (proposed) Treatment Order facilitate this treatment? Explain the purpose, method and duration of the immediate treatment. 2.12 Describe the beneficial and adverse effects of the patient’s treatment and provide details of how any side effects are being addressed. This criterion involves an assessment of whether the patient can receive treatment voluntarily rather than compulsorily. This criterion is not about treatment setting (i.e. inpatient or community), which is addressed below. 2.13 Provide details of key relationships, social connections and other services (e.g. Mental Health Community Support Services, general practitioner, private psychiatrist, carer, family, friend/s, guardian, nominated person) involved and the patient’s acceptance of the involvement of these in their care, treatment and support. 2.14 Has the patient expressed any views about voluntary treatment? Are the patient’s current actions compatible with those views? Report on Compulsory Treatment Section 5(d) – there is no less restrictive means reasonably available to enable the person to receive the immediate treatment. MHT 3 July 2014 2.15 Why does the treating team believe less restrictive treatment is not reasonable at present? Page 4 of 7 Local Patient Identifier FAMILY NAME MHT 3 Report on Compulsory Treatment GIVEN NAMES DATE OF BIRTH Mental Health Statewide UR Number SEX Place patient identification label (if available) 2.16 Describe the changes or strategies that need to occur in order for the patient to be able to be treated less restrictively. (This may include things that the patient needs to do, supports that need to be put in place or strategies to address non-adherence.) Part Three: Treatment and Recovery Please note: Part Three questions may not have to be answered if the patient has a comprehensive recovery plan (or similar) covering the relevant matters (please attach and direct the Tribunal to the relevant parts). However, you must answer questions 3.4 and 3.5 about the duration and category of Treatment Order being sought. 3.1 Describe how the patient has participated in the development of their recovery plan (or equivalent plan) and/or how their wishes have been taken into account. 3.2 Describe the patient’s current stage of recovery and anticipated progress. 3.4 What is the proposed treatment setting of the Treatment Order? Give details as to why community/inpatient treatment is necessary. If inpatient treatment is proposed, give details regarding plans to progress the patient to discharge (via community treatment or voluntary treatment). 3.5 What is the proposed duration of the Treatment Order? Give details as to why the duration is proposed. Report on Compulsory Treatment 3.3 If there are any alternatives to the current treatment plan being considered or other proposed treatment, please provide details. MHT 3 July 2014 3.6 Any other relevant information not covered in Parts One to Three. Part Four: Carer, family, nominated person’s views Page 5 of 7 Local Patient Identifier FAMILY NAME MHT 3 Report on Compulsory Treatment GIVEN NAMES DATE OF BIRTH Mental Health Statewide UR Number SEX Place patient identification label (if available) 4.1 If the patient is being supported by a carer, family, friend/s, guardian, or nominated person, please list their names and relationship to the patient. 4.2 Has the patient’s diagnosis been discussed with the patient’s carer/ family/ nominated person? 4.3 If the patient’s carer/ family/ nominated person (on behalf of the patient) has expressed views about the patient’s treatment and/or Treatment Order, please provide details (including whether these views can be complied with). MHT 3 July 2014 Report on Compulsory Treatment Page 6 of 7 Local Patient Identifier FAMILY NAME MHT 3 Report on Compulsory Treatment GIVEN NAMES DATE OF BIRTH Mental Health Statewide UR Number SEX Place patient identification label (if available) Signed: Print name: Date: Length of time you have known the patient: Date you last reviewed the patient: Date the patient was given a copy of this Report: If more than one person has authored the Report, please list their names and positions below: CONFIRMATION OF REPORT BY AUTHORISED PSYCHIATRIST I have reviewed and confirm the accuracy of this report. Print name: Authorised psychiatrist/ delegate Date: Date you last reviewed the patient: PATIENT RECEIPT OF REPORT If possible, please ask the patient to sign below to indicate they have received and read this Report. Signed: Date: Report on Compulsory Treatment Signed: MHT 3 July 2014 Last updated: July 2014 Page 7 of 7