- Zoo and Wildlife Solutions
advertisement

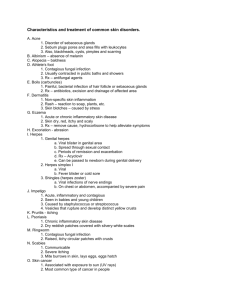
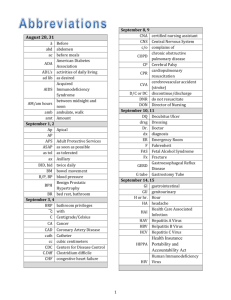
Summary of Risks Associated with Herpes B Virus in Macaques. KEY POINTS Herpes B virus causes few symptoms in infected macaques and does not significantly impact their welfare. Infection of humans with Herpes B virus is very rare with less than 50 cases recorded despite thousands of human exposures. No cases of human infection with Herpes B have ever occurred in zoos. Currently all human cases have occurred secondary to contact with Macaca mulatta, all in laboratories in the US. No documented cases of transmission have occured from other Macaca spp. However, if transmitted to a human, B virus infection has a nearly 80% casefatality rate.There are no vaccines. All Asian macaques should be assumed to be infected Implementing comprehensive biosecurity practices significantly reduces risk of human exposure. All zoos should have a written exposure protocol. Staff should be trained in disease prevention and action in the event of exposure. Introduction Herpes B virus occurs as a enzootic, life-long and generally asymptomatic infection of macaques. Barbary Macaques (Macaca sylvanus) have never been reported be infected with Herpes B Virus despite testing of large groups of wild and zoo animals. At present the infection status of most groups of Asian Macaca species in the managed programmes (and the wild) is unknown. Infection in Macaques The disease in macaques is usually mild and self-limiting. Clinical disease is characterised by the appearance of small vesicles on the lips or in the oral cavity. The vesicles typically rupture, scab and heal within 7-14 days. Conjunctivitis or nasal discharge may also be seen. Animals will start shedding virus (i.e. be infectious to other macaques and humans) at this time both from the site of infection and also from other body secretions. Gradually their body mounts an immune response and the virus goes into dormancy in nerve cells. The animals are likely to remain infected for life. Re-activation of latent infection, with viral shedding ± clinical signs, can occur; the factors leading to this are poorly understood, but may include stress, fever, injury and immunosuppression Surveillance and Testing Regimes. Testing macaques for herpes B virus infection is not straight forward. There is no herpes B specific antibody test available in Europe. False negative results are possible because latently-infected individuals will only maintain an antibody response for a period of 6-12 months after viraemia and hence infected animals can test negative with antibody detection tests. So if the animal did not shed virus for a long time it is possible that you will not detect any antibodies (false negative results) but when they start shedding the can infect the others in the group. Negative tests do not indicate an individual, or colony, is not infected with herpes B virus, and should not be relied upon for risk management purposes. However false positives are very unlikely. Produced by Zoo and Wildlife Solutions Ltd All macaque deaths should be thoroughly investigated The necropsy should preferably be carried out in a biohazard safety cabinet. Zoos which are unable to meet sufficient biosecurity standards for necropsy of macaques should consider submitting the body to an appropriate diagnostic laboratory. Zoos undertaking diagnostic testing should discuss their testing regimes and protocols with the OWM TAG Vet advisors before commencing and should inform the vet advisors of results. Infection in Humans Transmission to humans is by contamination of wounds or mucous membranes with body secretions or tissues from infected animals. B-virus disease in humans usually results from macaque bites or scratches Incubation periods may be as short as 2 days, but more commonly are 2 to 5 weeks. Vesicles on the skin develop at the site of inoculation 1–5 days post exposure in many cases, followed by swelling of local lymph nodes. Itchy skin and pain at the inoculation site may be intense. Other signs of infection include influenza like symptoms, such as persistent fever, headache, nausea, vomiting, and muscle pain. The disease progresses quickly to paralysis, numbness dizziness, double vision, difficult swallowing and confusion, respiratory difficulties, and coma. Death occurs 10–14 days post exposure in 70–80% of herpes B virus infected humans. Minimising exposure risk to humans Control of Herpes B infection in humans must focus on prevention of exposures and good education of staff. No protective vaccines are available Institutions should identify and collaborate with a local medical practitioner for establishing policy and protocols, and coordinating the response to an exposure event. All personnel, including contractors, students and volunteers, should receive appropriate training on the risk associated with herpes B virus, appropriate methods of restraint, and the use of protective clothing. Personnel should be required to sign that they acknowledge comprehension of institutional guidelines. Access to macaque areas should be restricted to people that have completed this process. Macaques should not be utilised for direct contact experiences, such as handling or feeding, for the general public. Asian macaques should not be housed in walk-through exhibits. Where Barbary macaques are housed in walk-through exhibits contact with the macaques and macaque body fluids (eg urine, saliva, faeces) should be avoided. Personnel coming into contact with macaques or their biological products should wear appropriate clothing that minimises the risk of contamination of skin and mucous membranes (e.g. eyes, mouth) with macaque secretions or excretions, and prevents scratches. This should include (at a minimum) longsleeved and long-legged garments. Strict personal hygiene is essential for herpes B virus risk management. Hand washing is the most effective means of preventing transmission of zoonotic diseases generally. Disposable gloves should be used in higher risk situations, but they do not negate the importance of hand washing after Produced by Zoo and Wildlife Solutions Ltd working around macaques, or after servicing areas potentially contaminated by macaques. The use of high pressure hosing in macaque areas should be avoided to minimise the production of aerosols from faeces, saliva and other secretions/excretions. Herpes B virus is readily destroyed by common detergents and disinfectants; these should be used when cleaning enclosures and associated equipment. Direct handling of macaques should be minimised. Capturing, restraining or otherwise handling fully conscious macaques is not recommended. Macaques should be physically restrained in a squeeze-cage and hand injected with a chemical restraint agent prior to handling. Behavioural conditioning of macaques is a practical and very useful technique to complement physical and chemical restraint options. All veterinary procedures on macaques should be carried out by suitably experienced and competent veterinarians with a full understanding of herpes B risk and risk management. Veterinary procedures should only be performed on animals that are sufficiently chemically restrained. Post exposure prophylaxis and first aid Humans should be considered as potentially exposed following any wound received from a macaque or contamination of mucous membranes or broken skin by macaque excretions and secretions. The adequacy and timeliness of wound decontamination procedures are the most important factors in preventing the risk of infection after herpes B virus exposure. Institution specific post-exposure first aid protocols should be developed in conjunction with the zoos medical practitioner. Information sheets containing basic information about herpes B virus, postexposure treatment protocols, and contacts for further information should be readily accessible and accompany the patient to the medical facility. The identified medical practitioner(s) may be unavailable at the time and the patient could be seen by a doctor unfamiliar with herpes B virus. For further information and advice please contact the Old World Monkey Taxon Advisory Group Veterinary Advisors Matt@zooandwildlifesolutions.com Produced by Zoo and Wildlife Solutions Ltd