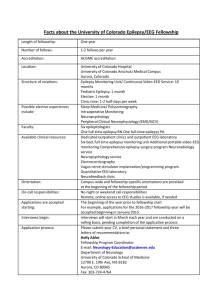
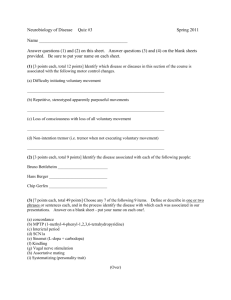
Epilepsy
advertisement

Part 1 Position Title: Division: Unit: Award: Location: Hours of Work: Fellow in Epilepsy (FIE) Medicine Neurosciences Senior Registrar Royal Prince Alfred Hospital, Camperdown, 2050 Grosvenor Outreach Clinic, Ashfield, 2131 0800-1700 (plus on call availability) Supervisor: A/Prof Armin Mohamed Staff Specialist Neurologist, Epileptologist and Position Emission Tomography Director of the Comprehensive Epilepsy Service (DCES) Additional Neurologists: Professor Craig Anderson Professor Michael Halmagyi Dr Jonathan Ell Professor David Burke Professor Michael Fulham Dr Judy Spies A/Professor Leo Davies Dr Michael Barnett Dr Stacey Jankelowitz Dr Simon Lewis Dr Kaitlyn Parratt Departmental Facilities: Royal Prince Alfred Hospital Camperdown, Sydney Facilities as per core training posts Part 2 Educational Objectives The main educational objective of this training post is to provide the Fellow with subspeciality experience in the clinical management of newly diagnosed, chronic and refractory epilepsy in the setting of a Comprehensive Epilepsy Service. Advanced technical skills in the acquisition and interpretation of routine, telemetry, ambulatory and inpatient video EEG will be obtained. In addition experience in the multidisciplinary, neuropsychological and surgical aspects of epilepsy will be gained. The comprehensive epilepsy service (CES) at RPA is one of three adult centres for treatment of complex epilepsy in New South Wales. The service provides care for patients with newly diagnosed and refractory epilepsy. In addition to a consultative service for outpatients and hospital in patients, there is an outreach clinic at the Grosvenor Centre in Ashfield for patients with severe intellectual disability. A wide range of diagnostic services including outpatient ambulatory recordings, prolonged video e.g. recordings, inpatient EEG monitoring with surface and intracranial electrodes are available. The unit works in close collaboration with the departments of PET, neurosurgery, radiology, neuropsychology, psychology and psychiatry. The primary role of the FIE is to maintain the highest standards of clinical care for all patients in the CES; this patient group includes all neurology inpatients and consultations from other wards and the Emergency Department. The FIE will be required to work closely with the Senior Medical, Nursing and Allied Health staff to provide a Quality Neurology Service to the patients of RPAH and SSWAHS. Members of the Comprehensive Epilepsy Service are committed to the fostering, teaching, training and development of quality Neurologists and will, where necessary, provide access to training in neurophysiology (EEG) to ensure that training requirements are met. The FIE will be supervised and trained in review and reporting of inpatient and outpatient EEG with the supervision of the DCES and the clinical nurse consultant in epilepsy. The FIE is not required to take part in the after-hours roster of Department of Neurology but is encouraged to do so. It is emphasised that the Fellow in Epilepsy (FIE) is an essential and important member of the CES Team whose aim is to deliver the highest quality medical care to patients at Royal Prince Alfred (RPA) Hospital whilst undergoing training in Epilepsy and EEG. The Team includes, in addition to the FIE, the Neurologists, Nurses, Technical, Secretarial and Laboratory staff of the Comprehensive Epilepsy Service and outside the Department the Ward Nurses, the Resident Medical Staff, the Allied Health staff and the Medical Imaging Technologists who also help care for our patients. RPA provides an opportunity to be exposed to a plethora of unusual epilepsy conditions, sophisticated and unique technologies and experts-in-their-fields. The FIE will have the opportunity to learn the fundamental skills necessary for a sound, productive and enjoyable career as a Neurologist. Job Description The FIE will have responsibility, through the Director of the CES (DCES), for the operational medical management of all epilepsy inpatients, however, there is a duty of care to ensure that the DCES is informed of all aspects of daily patient care even on weekends and after hours. All admissions and discharges (ward, ED etc) must be discussed with the DCES prior to admission or discharge. The FIE will perform daily ward rounds with the junior Medical staff and medical students (when applicable) on all patients. These rounds should be documented and dated in a clear, concise and legible manner in the individual patient’s medical record. Although it may not be possible for nursing staff to attend all such rounds, nursing input on each patient’s clinical condition should be sought and they should be informed of the plan of management for each patient after the round is completed. This will ensure effective communication and enable the efficient use of Hospital resources. It is preferable that these rounds are done early in the day so that emerging management issues can be dealt with promptly. Wherever possible these rounds should be done prior to any commitments (e.g teaching sessions) that may require that the FIE is absent from the ward. It is recognised that the FIE has Departmental approval to attend the inter-Hospital teaching program for the Sydney FIEs which are currently held on Wednesday afternoons at 1400 hrs. Nevertheless it is emphasised that emergency patient care should always take priority over such sessions. The FIE should communicate with patients and other medical, nursing, allied health (neuropsychology, nurse technicians, physiotherapy, occupational therapy, clerical staff, social work) staff in a professional and timely manner regarding patient management at all times. A professional manner embodies clear, courteous, respectful and considerate communication. Unprofessional behaviour detracts from quality patient care and will not be tolerated. The FIE is responsible for epilepsy clinics every week under the supervision of the DCES. This includes patients in epilepsy trials. The FIE may have to attend outreach clinics. The Registrar on-call should receive handover of all patients, including ward consultations that require on-going neurological input, on a daily basis as well as on Friday evenings prior to the weekend In which the FIE has been involved. The FIE has primary responsibility for organising and ensuring the smooth running of the New South Wales Epilepsy Group meeting (0800-930 hrs Thursdays) and the Epilepsy Clinical Case Reviews. The FIE may be required to present at the Neurology Clinical Case Reviews, citywide, statewide, national and international meetings. The FIE should be in attendance in the Comprehensive Epilepsy Service at least during the hours indicated in the relevant award unless the FIE is taking approved leave (see under General Accountabilities below). Authority to be absent during this period can only be given by the Director of CES. It is preferable that all requests for leave in such situations are made well in advance so that there is minimal disruption to patient care. Although urgent situations may arise and the Director of CES may be unavailable, approval should then be sought from the designated deputy. The FIE should explain the nature (details, risks, benefits) of all procedures that patients undergo prior to the test and should obtain written informed consent prior to these procedures where appropriate. The FIE should ensure that patients undergoing procedures are in a stable condition on the day of the test The FIE should be familiar with specific CES protocols (e.g. management of status epilepsy, etc.) and recommend revision where appropriate. The FIE will be involved in a daily the working meeting on EEG reviews both inpatients and outpatients and in the discussion and of management of cases of complex epilepsy. Part 3 Additional Educational Opportunities The FIE will be encouraged to attend the National Brain School on a monthly basis. Attendance at extra - Departmental meetings e.g. Neurology rounds / lectures at other Hospitals is approved, by the Director of Comprehensive Epilepsy Service, subject to there being appropriate cover for this period and that attendance at such meetings does not adversely impact on the clinical service of the Department. The FIE is to participate in quality activities to improve service delivery and patient outcomes. The FIE will assist in collection of data regarding performance of the CES in cooperation with the clinical nurse consultant in epilepsy. The FIE will attend weekly NSW Epilepsy Group Meetings. The FIE will be involved in preparation of and presentation at the local Epilepsy Society of Australia (ESA) meetings held in Sydney throughout the year. Attendance at the annual ESA meeting and EEG course will also be encouraged. Should the FIE wish to attend a relevant international meeting every effort would be made to accommodate this educational experience. The FIE is encouraged and expected to contribute to the further education and teaching of other resident staff, medical students, nurses and allied health staff through clinical cases (short / long cases), in-services and tutorials on topics of common or unique interest. The FIE will be actively involved in teaching of both basic physician trainees and Neurology Advanced trainees. This will include clinical teaching and specific EEG teaching for advanced trainees. Research opportunities are a significant focus of the FIE training year. The CES has a commitment to active ongoing research and projects will be discussed and selected early in the training year to maximise research opportunities throughout the fellowship appointment. The FIE will be encouraged to participate in research activities in the Department but only after approval from the Director of Comprehensive Epilepsy Service. It is essential that exposure to Epilepsy through patient care remains the highest priority of the FIE and is not compromised by participation in research activities. Thus participation in ongoing clinical trials and other research activities should occur only after approval from the Director of Comprehensive Epilepsy Service. Part 4 Weekly Timetable MONDAY TUESDAY WEDNESDAY 8:00-8:30 08:30-09:00 Teaching Session Tutorial Rm L8 EEG reporting Consult 8 Public Clinic ) Private Clinic EEG reporting Consult 8 THURSDAY Statewide Epilepsy Network Meeting Tutorial Rm L8 9:00-9:30 9:30-10:00 FRIDAY Ambulatory & Inpt EEG reporting with Armin and Fellow Clinical Trials/First Sz clinic 10:00-1200 Clinic 12:00-1300 13:00-1400 Multidisciplinary Meeting Urgent Consults 14:00-16:00 Part 5 Additional Documents Curriculum for EEG Training RPAH Comprehensive Epilepsy Service •Instrumentation, Polarity and Localization –Basic electricity and electronics –Amplifiers and their characteristics –Calibration –Waveform measurements (voltage, frequency, and duration) –Filters, sensitivity and frequency response curves –Localization and polarity –Electrical safety Clinic Neurology Clinical Meetings –Principles of EEG digitalization including analog-to-digital conversion (vertical and horizontal resolution), sampling rate (aliasing and Nyquist frequency), screen or monitor display (sensitivity scale and pixel resolution), etc –Recording reference (electrode site, average reference and Laplacian reference) –Montages and reformatting •Artefacts –All physiological and non-physiological artefacts including artefacts caused by chewing, sweating, eye movements, ECG, pulse motion, movement of head/body, electrode pops or movements, electrical fields from electrical devices (TV, telephones), respirator-induced movements, intravenous drips/drip pumps, etc •Neuroanatomy and Neurophysiology –Anatomy of neural generation –Mechanisms of EEG generation –Pathophysiology of abnormal waveforms –Basic mechanisms of epileptogenesis •EEG Recording Techniques –Head measurement and marking –Electrode position nomenclature (International 10-20 & 10-10 System) –Electrodes: properties and application techniques –Impedance measurements) –Activation procedures such as hyperventilation, sleep deprivation, photic stimulation •EEG Interpretation and Reporting –Principles of interpretation –General classification of abnormal EEGs –Elements of EEG reports –How to make good reports •Normal EEG in Adult & Elderly –Normal awake and normal sleep patterns including alpha, beta, theta, delta waves, mu, lambda waves, POST, Vertex sharp transients, spindles, K-complex –Normal responses to hyperventilation and photic stimulation –Changes in EEG in the elderly •Normal EEG in Infants and Children –Normal patterns of various ages from neonates up to adolescents •Normal Variants & Uncommon Patterns of Doubtful Significance –Small sharp spike / benign epileptiform transients of sleep –Wicket spikes –Psychomotor variants –14&6 positive spike –Breech rhythm –Sub-clinical rhythmic EEG discharges in adults (SREDA) –Alpha variants, –Phantom spike-waves patterns Non-Epileptiform Patterns –Slow waves –Triphasic waves –Generalized periodic complexes/patterns –Periodic lateralized epileptiform discharges (PLEDs) –Coma and stupor •Epileptiform Patterns –Definition of epileptiform patterns –Types & recognition of various inter-ictal epileptiform patterns such as sharp waves, spikes, polyspikes, 3Hz spike & wave complexes, 4-6Hz spike & wave complexes, slow spike & wave complexes, photo-paroxysmal responses, hypsarrhythmia –Ictal patterns –How to differentiate interictal from ictal patterns –EEG patterns in specific epilepsy syndrome such as focal (e.g. Benign Rolandic Epilepsy, Benign Epilepsy of Childhood with Occipital Paroxysms) and generalized (West Syndrome, Lennox-Gastaut Syndrome, Absence Epilepsy, Juvenile Myoclonic Epilepsy, etc) epilepsy syndromes –EEG in status epilepticus •Long-term EEG Monitoring –Types of long-term EEG recording –Indications and limitation of ambulatory and video-EEG monitoring –Various semiology and their localizing & lateralizing values •Use of EEG in the Management of Seizure and Non-Seizure Disorders –Strength and limitations of EEG –Indications for ordering EEG –Yields of finding abnormality (e.g. epileptiform patterns) in patient with & without seizure disorders –Use of long-term EEG monitoring in patients with refractory epilepsy –Use of EEG in treatment & prognosis of epilepsy –Use of EEG in non-seizure disorders (e.g. CVA; metabolic & toxic encephalopathies; dementia; brain tumors; head trauma; headaches, etc)