- Organ Donation Alliance
advertisement
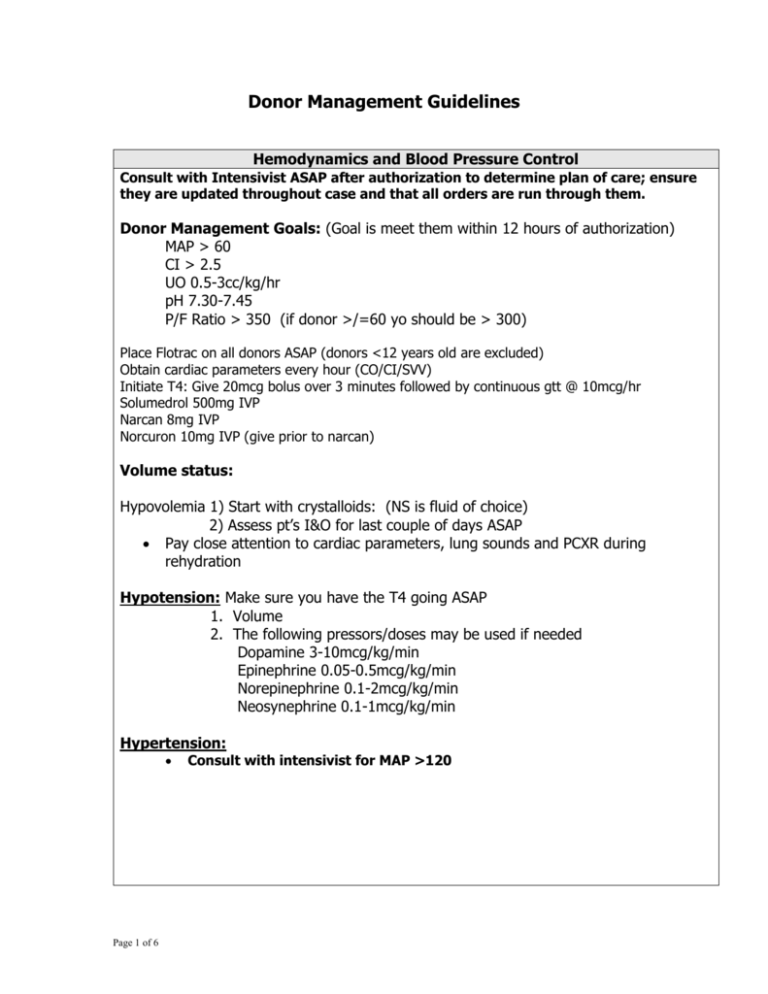
Donor Management Guidelines Hemodynamics and Blood Pressure Control Consult with Intensivist ASAP after authorization to determine plan of care; ensure they are updated throughout case and that all orders are run through them. Donor Management Goals: (Goal is meet them within 12 hours of authorization) MAP > 60 CI > 2.5 UO 0.5-3cc/kg/hr pH 7.30-7.45 P/F Ratio > 350 (if donor >/=60 yo should be > 300) Place Flotrac on all donors ASAP (donors <12 years old are excluded) Obtain cardiac parameters every hour (CO/CI/SVV) Initiate T4: Give 20mcg bolus over 3 minutes followed by continuous gtt @ 10mcg/hr Solumedrol 500mg IVP Narcan 8mg IVP Norcuron 10mg IVP (give prior to narcan) Volume status: Hypovolemia 1) Start with crystalloids: (NS is fluid of choice) 2) Assess pt’s I&O for last couple of days ASAP Pay close attention to cardiac parameters, lung sounds and PCXR during rehydration Hypotension: Make sure you have the T4 going ASAP 1. Volume 2. The following pressors/doses may be used if needed Dopamine 3-10mcg/kg/min Epinephrine 0.05-0.5mcg/kg/min Norepinephrine 0.1-2mcg/kg/min Neosynephrine 0.1-1mcg/kg/min Hypertension: Page 1 of 6 Consult with intensivist for MAP >120 Management of Heart Rate and Rhythm Symptomatic Bradycardia (hypotension or decreased cardiac/urine output: Notify intensivist ASAP Look for underlying cause!! - acidosis - electrolyte imbalance - cardiac contusion - hypothermia - handling of the heart Immediate intervention--Isuprel gtt or cardiac pacing Isuprel-1mg/250cc D5W Start @ 2-10mcgs/min and titrate Pacing-external, or if available can do transvenous if placed by a cardiologist If continues to be unstable proceed to the OR!! Symptomatic Tachycardia: Notify intensivist ASAP Look for underlying cause and treat!! - Hypovolemia - Hyperthermia - Infection - Vasopressin infusion (if caused by this, it is usually evidenced within 30” of start of infusion and takes 2-3hrs to stop) - Dopamine or Epinephrine infusion -Consider discontinuing T4 (after consultation with intensivist) V-Tach/V-Fib Initiate ACLS Cardiac Catheterization Management Consult with intensivist and consider pre-treatment if creat > 1.2 2amps Bicarb/1liter sterile water, run at 300/hr for 1 hr then at 100/hr until liter finished 600mg Mucomyst via NG q 12hrs x2 doses Instruct cardiologist to use no more than 60-70 cc of contrast Make sure cardiologist knows that we do not need an LV gram, only coronaries ***Make sure the pt is adequately resuscitated before going to CVL*** IV Orders Maintenance IV: D5 1/2NS U.O. Replacement: 1/2NS Page 2 of 6 Urine Output Polyuria: (Normal 0.5-3cc/kg/hr) Usually is caused by diabetes insipidus which results from the insufficiency of ADH from the posterior pituitary and is evidenced by rising Na and UO > 3cc/kg/hr. 1. Vasopressin (aqueous) IV drip use 1:1 concentration 1-2.5u/hr 2. DDAVP (desmopressin) 0.5-2.0mcg IVP over 10” (This may be repeated q2-3hrs) Hyperosmolar diuresis can be caused by elevated glucose, check glucose level and treat appropriately Oliguria/Anuria: Check patient’s volume status (use the Flotrac and I&O to guide you) REHYDRATE! If oliguria does not resolve with rehydration consult with intensivist for diuretic management. Blood Glucose Management Monitor accuchecks every 1-2hrs, if sugars unstable do every 1hr Insulin infusion to keep BS between 80 - 200 Electrolytes Potassium: <2.5 consult with intensivist 2.5-2.9 = 40meq via NG 3.0-3.5 = 30meq via NG 3.5-5.0 = Monitor If > 5.0 = consult with intensivist **You are much safer with a low potassium that a high one ** If giving lots of insulin your K+ will decrease,remember it is there, just hiding—get your sugars down** Phosphorus/Magnesium: Standards: Phos 3-4.5 Mag 1.7-2.3 Treatment(s): Bolus of Mg and Phos: 2gms MgSO4/100cc NS TRO 2 hours Kphos or NaPhos 30mmols/100cc NS TRO 2 hours If above Mg and PO4 are just slightly decreased then the above doses may be placed in the maintenance fluid. Use NaPhos if the K+ is elevated Use Kphos if NA elevated Calcium: monitor Ionized Calcium and replace with CaCl after consultation with intensivist Page 3 of 6 Thermoregulation Standard: 97-99O F or 36-37.5O C Hypothermia: wrap head, warm fluids, warming blanket, increase room temp Hyperthermia: infection should be considered Contact intensivist for further orders Hematology and Coagulopathy Parameters Maintain Hgb 8.0-10.0; Consider transfusion if <8.0 and after consultation with the intensivist **use leuko-reduced blood if possible** Labs: PT: normal 11.5-15.0 PTT: normal 28-38 Fibrinogen: normal 100% Platelets: normal >50 Page 4 of 6 If patient displays signs of frank bleeding, order PT/INR/PTT/Fibrinogen/Platelet count and call the intensivist for treatment. After all treatment, repeat CBC and coagulation tests Pulmonary Management Ventilation: Utilize Intensivist on call to determine appropriate ventilator settings Obtain ABGs on current ventilator settings and contact intensivist for further orders; consider the following: Ventilator settings: Mode: Pressure Regulated Volume Control (PRVC) Rate: Set initial rate to 12 PEEP: 8.0 FiO2: 1.0 TV: Target to 8ml/kg ideal body weight based on height to keep plateau pressure < 30cm/H2O If plateau pressure > 30 cmH2O, decrease TV in 1ml/kg IBW (no lower than 6ml/kg) and increase respiratory rate to maintain the same minute volume. ABGs 30min after above settings initiated. Target pH between 7.30 and 7.45 Ongoing management: Wean FiO2 to keep SpO2 > 93% and do not go below 40% Once TV determined, titrate respiratory rate to maintain pH within target range Lung recruitment maneuver q 2-4hrs after patient properly resuscitated: CPAP of 40cmH2O for 40 seconds For wheezing or signs of reactive airways give 8puffs Combivent MDI q 4hrs PRN ABGs a minimum of q 4hrs Consider prone positioning if refractory hypoxemia persists Contact Intensivist for: Persistent acidemia with minute ventilation > 15 and/or pH <7.30 Persistent hypoxemia, PaO2 < 75mmHg or SpO2 <93 on more than .60 FiO2 and/or more than 12cm PEEP Ventilator changes not included on the order sheet Total respiratory rate >30 bpm Does not tolerate lung recruitment manuever Lung Placement O2 challenge: After patient stable on above ventilator settings Increase FiO2 to 100% get ABG after 10 minutes If PO2 > 300 and there are no absolute contraindications for lung placement make lung offers Sputum gram stain Lung measurements, chest circum. @ nipple line during full expansion CXR Have O2 challenge and CXR current w/in 2 hours of lung offers Page 5 of 6 Page 6 of 6