Tubular Transport Processes
advertisement

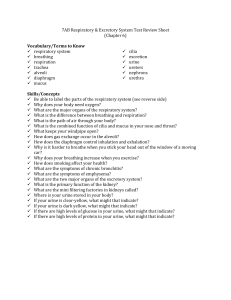
Tubular Transport Processes Lecture Objectives: 1) List the percentage of the filtered load of NaCl and water reabsorbed in the proximal tubule, thin descending and thick ascending limb of the loop of Henle, and the distal tubule and collecting duct a. Proximal tubule (high water permeability + Na, H antiport) - primary active transport of sodium i. Sodium is transported from the lumen through the brush border by a symport or antiport and then from inside the cell to the blood by the Na, K ATPase ii. Chloride and water reabsorption occurs in the proximal tubule and follows sodium as it is transported from the lumen to the blood 1. Na reabsorption decreases urine sodium concentration about 2.5 mEq/L a. Decreased urine [Na] causes passive back leak i. Net reabsorption = reabsorption – passive back leak 2. Urine osmolality decreases about 5 mOsm/Kg water 3. Decreased urine osmolality causes H2O reabsorption (trans- and paracellular) 4. Paracellular chloride reabsorption follows sodium reabsorption iii. The rate of active sodium transport controls the rate of renal oxygen consumption via changes in cell [ADP] and [Pi] 1. Renal oxygen consumption is linearly related to net renal sodium reabsorption a. ATP is needed for the Na, K ATPase --- which means the more the pump functions to reabsorb sodium, the more ATP is needed, the more oxygen is needed b. Thin descending c. Thick ascending – sodium diffuses across the luminal membrane via Na+, K+, 2Cl- symport i. Potassium and chloride enter the cell via secondary active symport with sodium ii. This segment reabsorbs 25% of filtered NaCl and 20% of K+ 1. Loop diuretics (ethacrynate and furosemide) are competitive inhibitors of the luminal symport mechanism iii. The thick ascending limb is NOT permeable to WATER under any conditions iv. Lumen positive potential drives PARACELLULAR reabsorption of cations d. Distal tubule 2) Describe the changes that occur in the concentration of Na, Cl, K, urea, inorganic PO4, bicarbonate, glucose, and amino acids in the tubular flow (urine) as it flows through the proximal tubule a. As urine flows through the proximal: i. Cl-, K+, and urea concentration in the urine INCREASE ii. Na+ and osmolality in the urine DECREASE SLIGHTLY iii. Pi, HCO3, and Glucose leave the urine almost all together 1. Pi remains slightly (0.7) 3) Describe the mechanism responsible for transport of Na across the luminal membrane (from urinary space to the cell) in: a. Proximal tubular cells i. In the peritubular capillary, the balance of Starling forces favors reabsorption from ISF to capillary ii. Primary Active Transport – used to reabsorb sodium from proximal tubule b. Cells of the thick ascending limb of the loop of Henle i. Na+, K+, 2Cl- Symport c. Principal cells of the collecting duct i. Sodium transport is stimulated by ALDOSTERONE 4) 5) 6) 7) 8) 1. Short term (45minutes) – increase in number of luminal channels for Na and K 2. Long term (hours) – increase in synthesis of Na+, K+, ATPase ii. Antidiuretic Hormone (ADH) – inserts H2O channels in luminal membrane 1. Collecting duct paracellular path has low sodium permeability, little sodium back leak 2. Collecting duct produces a urine with very low [Na] when Na+ is low Compare the osmolality of the urine in the proximal tubule to the osmolality of the peritubular capillary plasma a. Osmolality of urine in proximal tubule SIMILAR to Osmolality of peritubular capillary plasma Define these terms: primary active transport, secondary active transport, symport (cotransport), and antiport (countertransport) a. Primary Active Transport – directly uses energy to transport molecules across a membrane b. Secondary Active Transport - contrast to primary active transport, there is no direct coupling of ATP; instead, the electrochemical potential difference created by pumping ions out of the cell is used. i. The two main forms of this are counter-transport (antiport) and co-transport (symport). c. Symport - an integral membrane protein that is involved in movement of two or more different molecules or ions across a phospholipid membrane such as the plasma membrane in the same direction, and is therefore a type of cotransporter i. Typically, the ion(s) will move down the electrochemical gradient, allowing the other molecule(s) to move against the concentration gradient d. Antiport - an integral membrane protein which is involved in secondary active transport of two or more different molecules or ions (i.e. solutes) across a phospholipid membrane such as the plasma membrane in opposite directions. Name the mechanism responsible for reabsorption of glucose, lactic acid, and amino acids in the proximal tubule a. Secondary active transport – glucose transport from lumen to cell is energized by diffusion of sodium from lumen to cell i. Symport mechanisms exist for other sugars, amino acids, and some organic anions (lactate, pyruvate) ii. These molecules are moving against their concentration gradients by the energy from sodium moving down its gradient Define the term “transport maximum (Tm)” as used in renal physiology a. The maximal transport rate for secondary active symport is determined by the NUMBER OF TRANSPORTERS AVAILABLE Define “osmotic diuresis”, explain how an osmotic diuresis occurs and how sodium, anion, and water excretion increase during an osmotic diuresis a. Osmotic Diuresis – an increase in urine flow and in solute excretion i. Osmotic diuresis occurs when any filtered solute is not reabsorbed 1. Example: uncontrolled diabetes mellitus, hyperglycemia leads to filtration of excess glucose a. The osmotic effect of glucose in the urine retards water reabsorption increased urine flow b. Glucose transporters are saturated (Tm is exceeded) c. Sodium pump continues while glucose holds water in urine i. Low urine sodium creates an abnormal large [Na] gradient favoring back leak ii. When passive sodium back leak = active sodium reabsorption, NET sodium reabsorption goes to zero as urine flows through the tubule 9) Explain the difference between an osmotic diuresis and a water diuresis a. While an osmotic diuresis is an increase in urine flow and solute excretion, a Water Diuresis is an increase in urine flow WITHOUT an increase in solute excretion 10) Compare the osmolality of urine leaving the thick ascending limb of the loop to the osmolality of plasma. Also, describe the transport characteristic of the loop that is responsible for the difference in osmolality a. The thick ascending limb is not permeable to water b. Osmolality therefore is decreased because water is retained while ions are reabsorbed 11) Name the tubule segments and cell type affected by aldosterone and ADH a. Aldosterone – collecting duct b. ADH – collecting duct 12) In a subject adapted to a low sodium diet, compare the urine sodium concentration in the proximal tubule versus the medullary collecting duct a. When sodium intake is low, the collecting duct urine will have very low [Na+] 13) Describe the short and long term effect of aldosterone on collecting duct sodium transport a. Short term – increased channels b. Long term – increased ATPase synthesis 14) Describe the effect of ADH on the cortical and medullary collecting ducts a. ADH inserts water channels into the luminal membrane i. Allows for increased water reabsorption and decrease in urine volume 15) Compare the value of urine osmolality to plasma osmolality for urine entering the early distal convoluted tubule, and for urine leaving the late distal convoluted tubule, when plasma [ADH] is high and when plasma [ADH] is low a. HIGH plasma ADH will lead to higher urine osmolality because more water is reabsorbed i. Plasma osmolality will decrease because of the increase in water b. LOW plasma ADH will lead to higher urine osmolality because less water is reabsorbed i. Plasma osmolality will increase because of the loss of water Proximal tubule Descending limb Thick ascending limb Distal tubule and collecting duct TOTAL NaCl 67% ZERO 25% 7% 99% H2O 67% 15% ZERO 17% 99%