Catheter Associated Urinary Tract Infections - Jenna Ruimveld
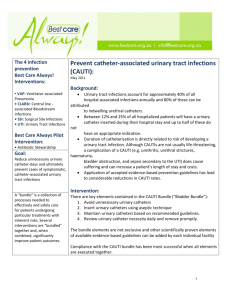
advertisement
Running head: CATHETER ASSOCIATED URINARY TRACT INFECTIONS Catheter Associated Urinary Tract Infections Jenna L. Ruimveld, Courtney Rehm, Michelle Heim, & Abigail Lee Ferris State University 1 CATHETER ASSOCITED URINARY TRACT INFECTIONS 2 Abstract Catheter associated urinary tract infections are a common infection that occurs in the healthcare setting. In order to improve patient outcomes overall, it is best to constantly evaluate clinical practice procedures and guidelines to ensure that best practice is being utilized. Currently, indications for indwelling urinary catheter (IUC) placement by Spectrum Health are those set forth by the Center for Disease Control. These include urinary retention or bladder obstruction, need for accurate intake and output, urologic/gynecologic surgery, assist in healing of sacral or perineal wound of incontinent patient, prolonged immobilization from trauma or surgery, and improved comfort for end of life care (Gould, Umscheid, Agarwal Kuntz, & Pegues, 2011). The purpose of this paper is to identify a current clinical problem, obtain information regarding the subject, develop a plan for quality improvement, implement recommended changes, and evaluate effectiveness. CATHETER ASSOCITED URINARY TRACT INFECTIONS 3 Catheter Associated Urinary Tract Infections Catheter associated urinary tract infections (CAUTI) are described as preventable infections related to co-morbidies, extended hospital stays, and increased hospital costs (Oman et al., 2012, p.548). CAUTIs are “one of the most common health care-associated infections in the critical care setting” (Marra et al., 2011, p.817). Nurses are responsible to be the patient advocates, supporting them by providing the highest standards of care. There are evidence-based practice guidelines to follow in order to prevent CAUTIs and nurses are responsible to implement these measures to ensure patient safety and health. Quality improvement practices are defined as “an ongoing process of innovation, prevention of error, and staff development that is used by a institutions that adapt quality management philosophy” (Yoder-Wise, 2011). In nursing it is important for nurses to advocate for their patients by not only adhering to best practice guidelines, but also recognizing a gap in quality care. Policy changes would be best when implemented using the transformational leadership (Yoder-wise, 2011). Transformational leadership focuses on the leader meeting the needs of the followers and motivating them to reach a higher standard. (Yoder-Wise, 2011, p. 10). The leadership role in this theory is one that promotes change in a positive, creative, and optimistic way using five key practice steps; challenge, inspire, enable, model, and encourage (Yoder-Wise, 2011, p.40). Once the need for improvement is identified by staff (CAUTI), an interdisciplinary team is created consisting of nurses, nursing managers, and other staff. This team works together to develop a change in clinical guidelines. In order to do this, both current policy and research is utilized. Clinical Need As stated before, CAUTIs are one of the most common hospital acquired infection, “Urinary tract infections (UTI’s) account for approximately 40% of all hospital-acquired infections in the United CATHETER ASSOCITED URINARY TRACT INFECTIONS 4 States; more than 80% are associated with an indwelling catheter,” (p. 247). Gray (2008) also reports that the cost of treating a single episode of CAUTI ranges between 1,000 and $3,000, with 90,000 additional hospital days needed cumulatively each year for this treatment (p. 247). CAUTIs are one of eight hospital-acquired conditions that health care facilities would no longer receive reimbursement for, according to the Centers for Medicare and Medical Services, making CAUTI prevention an important topic in the eyes of many healthcare employees (Saint, Meddings, Calfee, Kowalski & Krein, 2009). Catheter care and infection prevention falls firstly to that of the nurse. These can include catheter placement, catheter care, perineal care, and identification of IUC continuation or removal. Interdisciplinary Team Interdisciplinary teams are vital to quality improvement, “Interprofessional teams are essential to quality patient care…[members] must work together to achieve cost-effective care while achieving the highest quality of care in the healthcare setting” (Yoder-Wise, 2011, 362). The interdisciplinary team not only involves those who have direct access to patient care, but the stakeholders in the organization as well. The interdisciplinary team should consist of nursing aids/techs, nurses, physicians, infection prevention team, and organization members. Nurses and nursing aids are the first line of defense against CAUTI’s because they are the ones that are directly involved with patient care; nurses place indwelling urinary catheters and nursing aids assist in maintenance and catheter care. Nurses are also involved in the evaluation of IUC removal or continuation, they must advocate for their patients by discussing the indications for earliest removal. Physicians play a large role in CAUTI prevention, they have the power to continue or discontinue orders for IUCs, “The physicians in charge made decisions regarding inserting or removing the urinary catheters” (Huang, et al, 2004, p.975). The infection prevention team is a group of members that’s main goal is to reduce infection within the hospital. They are involved in this change by assisting in the CATHETER ASSOCITED URINARY TRACT INFECTIONS 5 research as well as in the creation of the changes in policy and procedures. The board members are also involved in the interdisciplinary team, as they approve changes in policy and procedures. Board members are also some of the biggest stakeholders for CAUTI prevention because it is such a large cost for many hospitals. The team will work together and individually, all performing their own parts to improve quality and patient outcomes. Data Collection Method Before policy changes can be implemented, research and evidence must be collected, “After the multidisciplinary team forms, the group collects data to measure current status of the activity, service or procedure under review” (Yoder-Wise, 2011, p.396). A literature search must be performed in order to obtain the most valid and current research and recommendations. Articles must meet criteria in order to ensure that the data is valid and reliable to use to influence best practice. Articles must be published in peer reviewed nursing journals, using randomized control trials, meta-analysis, or others of a high level of evidence, using the evidence pyramid. Each article will be critiqued for not only author biases, but also limitations and recommendations for future practice. Data will also be collected from patient chart as well as data reported from each individual unit. All CAUTIs will be reported to the charge nurse, who in turn will report them to infection prevention team. In the process of transformational leadership the first key aspect is challenge the process. This was performed initially when the need for change was identified. The interdisciplinary team was formed, which would be considered “inspiring shared vision”. Lastly data collection falls under the next step; enabling others to make a change. Outcomes CAUTI prevention is a large topic for many hospitals, “In recent years, prevention of CAUTI has become even more important as the Centers for Medicare & Medicaid Services no longer CATHETER ASSOCITED URINARY TRACT INFECTIONS 6 reimburses hospitals for costs related to the treatment of CAUTIs on the grounds that they are largely preventable” (Purvis et al., 2014). Most CAUTIs can be prevented if the proper policies and procedures are utilized. Because of this, a goal is within one year’s time reduce the CAUTI rate by 40% hospital wide. Decreasing the rate of catheter associated urinary tract infections can improve many standards of nursing care. First of all is “Quality of Practice” (ANA, 2010, p.11). Quality of nursing practice would significantly improve because a decrease in infection rates directly correlates to an increase of quality of care given. Another standard that is affected is communication. The American Nurses Association (2010) describes communication as “communicating effectively in all areas of practice” (p. 10). The implementation of prove it or remove it, requires an increase in communication between physicians and nurses in order to decrease the length that a indwelling urinary catheter is in place. Implementation Strategies Change in the nursing environment can best be implemented using the “Seven Phases of Planned Change” by Lippit, Watson, and Westley (Yoder-Wise, 2011, p. 328). In this process the need for change is identified (high incidence of CAUTIs), the nursing leader or manager makes a connection with bedside staff, the problem is then defined, outcomes and goals are set and ways of achieving said goals are explored, the plan for change is set in place, change is accepted by staff, and lastly staff redefine their practices (Yoder-Wise, 2011). Nursing leaders must also support their staff and their opinions, advocating not only for the patients but also for the staff they are managing, “…facilitation is considered necessary for enabling successful implementation. Facilitation is the “process of enabling (making easier) the implementation of evidence into practice” (Dogherty, Harrison, Graham, Vandyk, Keeping-Burke, 2013, p. 129). The consideration of the nurse’s attitude towards this change is key to implementing the best practices and improving patient quality and safety. The best outcomes for CATHETER ASSOCITED URINARY TRACT INFECTIONS 7 change would be for a leader to use the transformational leadership strategies, setting examples and motivating staff to make quality improvement changes. Evaluation The main goal of this quality improvement is to decrease and eliminate the occurrence of CAUTIs in hospitalized patients. Decreasing the risk of CAUTIs and infections in hospitalized patients will not only decrease hospital costs, but increase patient satisfaction and improve overall patient outcomes. To identify a change in the incidence of CAUTIs, data will be collected day to day from nurses and patient charts. Charge nurses will report the number of CAUTIs to the nursing manager where data can be track and analyzed. There are many benefits to decreasing CAUTI rate in hospitals, including decreased hospital and patient costs, as well as patient satisfaction. Hospital costs can be evaluated through monthly budgeting and spending reports, and patient satisfaction can be determined by patient exit surveys as well as length of stay. Conclusion It is vital for nurses to use critical thinking to develop the best practices in order achieve positive patient outcomes. Every day, nurses work as part of an interdisciplinary team, along with nursing leaders and managers to improve patient safety, health, and satisfaction. In order to make these changes the staff must be receptive to these evidence based changes and willing to modify patient care to obtain positive patient outcomes. Changing hospital policy and procedure is not an easy task, however it is a necessary one when patients are at risk. All healthcare professions need to always strive to meet the highest standards of quality care possible and to motivate others to do the same. CATHETER ASSOCITED URINARY TRACT INFECTIONS 8 References American Nurses Association. (2010). Nursing Scope and Standards of Practice. Silver Spring, MD. Dogherty, E. J., Harrison, M. B., Graham, I. D., Vandyk, A., & Keeping-Burke, L. (2013). Turning Knowledge Into Action at the Point-of-Care: The Collective Experience of Nurses Facilitating the Implementation of Evidence-Based Practice. Worldviews On Evidence-Based Nursing, 10(3), 129-139. doi:10.1111/wvn.12009 Gould, C., Umscheid, C., Agarwal, R., Kuntz, G., & Pegues, D. (2011). Healthcare Infection Control Practices Advisory Committee. Guideline for Prevention of Catheter-Associated Urinary Tract Infections 2009. Journal Of Wound, Ostomy & Continence Nursing, (4S), S30. Gray, M. (2010). Reducing catheter-associated urinary tract infection in the critical care unit. AACN Advanced Critical Care, 21(3), 247-257. doi: 10.1097/NC1.0b013e3181db53cb Huang, W., Wann, S., Lin, S., Kunin, C., Kung, M., Lin, C., & ... Lin, T. (2004). Catheter-associated urinary tract infections in intensive care units can be reduced by prompting physicians to remove unnecessary catheters. Infection Control & Hospital Epidemiology, 25(11), 974-978. Oman, K. S., Flynn, Fink, R., Schraeder, N., Hulett, T., Keech, T., & Wald, H. (2012). Nurse-directed interventions to reduce catheter-associated urinary tract infections. American Journal Of Infection Control, 40(6), 548-553. doi:10.1016/j.ajic.2011.07.018 Marra, A. R., Zinsly, Gonçalves, P., Cristina B., M., Moura, D., Guastelli, L., & ... Edmond, M. B. (2011). Preventing catheter-associated urinary tract infection in the zero-tolerance era. American Journal Of Infection Control, 39(10), 817-822. doi:10.1016/j.ajic.2011.01.013 Purvis, S., Gion, T., Kennedy, G., Rees, S., Safdar, N., VanDenBergh, S., & Weber, J. (2014). Catheter-Associated Urinary Tract Infection. Journal Of Nursing Care Quality, 29(2), 141148. doi:10.1097/NCQ.0000000000000037 CATHETER ASSOCITED URINARY TRACT INFECTIONS Saint, S., Meddings, J., Calfee, D., Kowalski, C., & Krein, S. (2009). Catheter-associated urinary tract infection and the Medicare rule changes. Annals Of Internal Medicine, 150(12), 877-884. 9