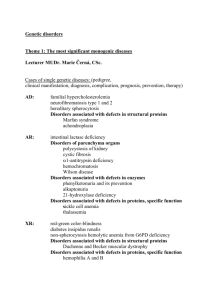
Chem Path Revision Notes
advertisement

Chemical Pathology Notes Fluid Balance - ⅔ INTRACELLULAR - ⅓ EXTRACELLULAR Electrolytes Cations Intracellular = K+ (3.5 - 5) Extracellular = Na+ (135 - 145) Anions Intracellular = protein and phosphate Extracellular = Cl- and HCO3- (22 -26) Osmolality “Total number of solute particles in solvent” (280-295 mosmol/l) Calculated Plasma osmolality = 2([Na+] +[K+]) + urea +glucose Osmolar Gap (<10) = Measured osmolality – calculated osmolality Anion Gap (~ 18 mmol) = Na + K - Cl - Bicarbonate Key controllers of ECF Extra-renal System Stimulated by: o Osmoreceptors o Baroreceptors (low volume) Action by: o Thirst o Anti-diuretic hormone from posterior pituitary o ANF (reduced sensitivity of osmoreceptors, RAA antagonism) Intra-renal System Stimulated by: o Reduced renal perfusion Action by: o Renin-angiotensin-aldosterone system (positive) o ANF (negative) Too much fluid Increased intake (rarely a problem) Increased/inappropriate sodium reabsorption o Cardiac failure o Nephrotic syndrome Too little fluid Inadequate intake (during illness) Distribution problem o Sepsis o 3rd spacing Reduced excretion o Renal failure o Nephritic syndrome Excess loss o Fluids (gut, kidneys, skin, respiratory) o Blood (internal vs. external) Sx Confusion/coma Cool hands Cap. Refill Tachycardia Tachypnoea BP/postural drop JVP Sunken eyes Dry mouth Lungs clear Urine output (< 30ml/hr) No oedema Tx CRYSTALLOIDS - electrolytes in water COLLOIDS - fluids with high molecular weight molecules Types Normal saline Dextrose saline 5% dextrose Hartmannʼs Natural (e.g. blood, albumin) Synthetic (e.g. Gelofusin, Haemaccel) Contents 154 mmol Na+ in 1L 30 mmol/l Na+ + 40g dextrose 50g dextrose in IL Anions + Cations + Ca + lactate Dextran compounds Electrolyte Disorders Hyponatraemia Na+ < 135 mmol/l Serum sodium (mmol/l) 130-135 125-130 115-125 <115 Hypovolaemia Cause Renal Adrenal failure (Addisons) Diuretics U. Na+ (mmol/l) >20 Features Asymptomatic MILD - N/V, mild disorientation MODERATE - confusional state SEVERE - seizures/coma Normovolaemia Non-renal Vomiting Diarrhoea Skin loss <10 Hypervolaemia Renal ARF/CRF SIADH >20 >20 Syndrome of Inappropriate ADH Malignancy o Small cell malignancies (lung, pancreas, lymphoma) Lung pathology o TB, pneumonia, abscess CNS pathology o Infections, bleeds Drugs (carbamezapine, chlorpropramide, cyclophosphamide, ectasy (MDMA)) Sx ↓ [Na] Euvolaemia Non-renal Cardiac Failure Cirrhosis Nephrotic syndrome Inappropriate IV fluid <10 ↓osmolality ↑urinary [Na] No other cause (diagnosis of exclusion) Increased loss (common) o Gut (diarrhoea, vomiting, fistulae) o Kidneys (↑mineralocorticoid, diuretics, RTA 1 & 2) Hypernatraemia Insufficient fluid intake Water loss increased relative to sodium loss o DI (low urine osmolality) o Osmotic diuresis (high urine osmolality) o Primary aldosteronism Hypokalaemia Reduced intake (rare) Cellular uptake o Insulin, alkalosis Sx: Generally asymptomatic Muscle weakness Reduced gut motility Cardiac arrhythmias Hyperkalaemia Increased intake (rare) Cellular loss o Acidosis, severe haemolysis/rhabdomyolysis Decreased loss o Renal failure o Decreased mineralocorticoids (RTA 4) o Potassium sparing diuretics + NSAIDs + ACEi Sx: Cardiac arrest Muscle weakness Tx Stabilise the myocardium o 10ml 10% calcium gluconate Drive K into the cells o 10u insulin + 50ml 50% dextrose o Salbutamol Mop up K o Calcium resonium, haemofiltration Calcium Serum calcium: 2.2 - 2.6 mmol/l Paraesthesiae Hypocalcaemia Ca < 2.2 mmol/l Causes: Parathyroid removal Vit. D deficiency Renal disease Diagnosis U&Es - ? Renal disease Serum PTH Clinical features: Asymptomatic Perioral paraesthesia Trousseau’s sign, Chvostek’s sign Prolonged QT Cataract (chronic) Severe o Calcium gluconate infusion Vit. D intoxication Diuretic therapy Tertiary hyperparathyroidism Milk-alkali syndrome Osteitis fibrosa cystica Treatment Mild o Calcium supplements In renal failure o Alphacalcidol Hypercalcaemia Ca > 2.6mmol/l Causes: 1° Hyperparathyroidism Myeloma Bony mets PTH-related protein Granulomatous disease (TB, sarcoid) Sx: Asymptomatic Nephrogenic DI (thirst, polyuria etc) Renal stones Abdominal symptoms (vomit, constipation, pain) Weakness Fatigue Confusion Treatment 3.5 = MEDICAL EMERGENCY Fluids (0.9% normal saline) - promote diuresis Bisphosphonate - inhibit further bone resorption Others: surgery, steroid for sarcoid Acid-base balance pH pCO2 pO2 HCOBase excess Normal range 7.35 - 7.45 4.5 - 6 11-14 22 - 26 -2 to +2 Metabolic Acidosis ↑[H+] = pCO2 ↓[HCO-] Metabolic Alkalosis ↓[H+] = pCO2 ↑[HCO-] Respiratory Acidosis ↑[H+] = ↑pCO2 [HCO-] Respiratory Alkalosis ↓[H+] = ↓pCO2 [HCO-] Hydrogen ions are buffered by: Bicarbonate H++HCO3- ↔ H2CO3 Haemoglobin H+ + Hb- ↔ HHb Phosphate H++HPO4- ↔ H2PO4 Renal Function Tests GFR “Volume of unit plasma that can be completely cleared of marker substance per unit time.” Normal = 60 - 120 ml/min Varies considerably (1ml/min per year) Urine Microscopy White blood cells o Infection o Sterile pyuria - partially treated UTI or stone/tumour Bacteria o Infection Hyaline casts (normal mucoprotein) o Healthy Red cell casts o Glomerulonephritis/severe tubular damage White cell casts o Pyelonephritis/glomerulonephritis Crystals o Calcium oxalate (75%) - spikey and radio-opaque [metabolic/idiopathic] o Triple phosphate (17%) - large, radio-opaque may form staghorn calculus [proteus UTIs] o Uric acid (5%) - smooth, brown, radio-lucent [hyperuricaemia] o Hydroxyapatite (1%) o Cysteine (1%) - yellow, crystalline, semi-opaqe [renal tubular defects, cystinuria] Liver Function Tests Test Bilirubin (total) Direct Bilirubin (conjugated) Alkaline phosphatase Aspartate transaminase Alanine transaminase Albumin -glutamyl transpeptidase Albumin -globulin Prothrombin time Normal Values 5 – 17 mol/L < 5 umol/L 35 – 130 iu/L 5 – 40 iu/L 5 – 40 iu/L 35 – 50 g/L 10 – 48 iu/L 35 – 50 g/L 5 – 15 g/L 12-16 seconds Congenital Syndromes Condition Crigler- Najjar Inheritance AR Gilbert’s Variable Dubin-Johnson AR Rotor (D-J subtype) AR Abnormalities ↑ with choleostasis ↑when hepatocytes die (ischaemia, toxins, viruses) ↓in sepsis, malnutrition, chronic LD ↑ with ETOH & phenytoin Deficiency Bilirubin metabolism (UGT1A1) ↓ glucoronyltransferase activity Defective anionic conjugate transfer Unknown Presentation Hyperbilirubinaemia +/- Kernicterus ↑bilirubin N. liver chemistry Asymptomatic/no abnormal LFTs ↑Urine coproporphyrin Unpigmented liver Uric acid metabolism Plasma concentrations. o Men 0.12 – 0.42 mmol/l o Women 0.12 – 0.36 mmol/l Gout Monosodium urate crystals Men>women Clinical features Exquisite pain Red, hot and swollen joint 1st MTP joint is classical Allopurinol for chronic episodes Diagnosis Negatively birefringent crystals Treatment NSAIDS are the first line treatment acutely Colchicine lowers urate levels Pseudogout Pyrophosphate crystals Self limiting 1 – 3 weeks Positively brefringent crystals Endocrine Investigations Condition Cushing’s Syndrome (↑Cortisol) Causes Pituitary (Micro/macroadenoma) Adrenals (Adenoma/carcinoma) Malignancy Exogenous steroids Diagnosis Midnight plasma cortisol Low dose DEXA test Salivary cortisol Urinary free cortisol Conn’s Syndrome (↑Aldosterone) “Hyperfunction of aldosterone secreting cells” Adenoma, carcinoma, hyperplasia Plasma aldosterone ↑ Plasma renin ↓ Addison’s Disease (↓Cortisol) Short Synacthen test Thyroid Disease TSH T3 +/- thyroid autoantibodies Protein Markers Protein CRP α-1 anti-trypsin Transferrin Caeruloplasmin Function Acute phase protein Prevents neutrophil elastase activation Plasma Fe Transport Contains Cu Mops-up superoxide radicals Ferritin Haptoglobin β2-microglobulin Information Peaks at 48h ↓ in emphesema & cirrhosis Deficiency in Wilson’s disease ↓ in IDA, ↑ in Fe overload & acute inflammation ↓ in haemolysis MHC Class I component Nutrition Fat Soluble Vitamins A Retinol D Cholecalciferol E Tocopherol K Phytomenadione Deficiency Colour Blindness Osteomalacia/rickets Anaemia/neuropathy ?malignancy/IHD Defective clotting Excess Exfoliation Hepatitis Hyper-calcaemia Test Serum Serum Serum PT Water Soluble Vitamins B1 Thiamin B2 Riboflavin B6 Pyridoxine B12 Cobalamin C ascorbate Folate Niacin Deficiency Beri-Beri, Neuropathy Wernicke Syndrome Glossitis Dermatitis/Anaemia Pernicious anaemia Scurvy Megaloblastic Anaemia Neural tube defect Pellagra Excess Neuropathy Renal stones Test RBC transketolase RBC glutathione reductase RBC AST activation Serum B12 Plasma RBC, folate Trace Elements Iron Iodine Zinc Copper Fluoride Deficiency Hypochromic Anaemia Goitre Hypothyroid Dermatitis Anaemia Dental caries Excess Haemochromatosis Test FBC, Fe, Ferritin, TFT Wilson’s Flourosis Cu, Caeroplasmin Metabolic Disorders Disorder(s) Amino acid disorders Organic acidurias Urea cycle defects Carbohydrate disorders Peroxisomal disease Mitochondrial disease Examples Autosomal recessive defect in metabolism of single amino acid Defective late metabolism of single amino acid (usually branched) Deficiency of an enzyme involved in the urea cycle → build up of ammonia Alteration of carbohydrate cycling in the cell Disorders of lipid metabolism where there are empty cell persoxisomes Mutations in mitochondrial DNA. Most serious when affects muscle, brain. Defect PKU (↑ phenylalanine) Homocystinuria (↑ Methylmalonic acidaemia, Propionic acidaemia, Isovaleric acidaemia, Maple syrup urine disease 6 disorders e.g. arginaemia, citrullinemia Lactose intolerance Gycogen storage disorders Zellweger syndrome Clinical characteristics Failure to thrive Seizures Musty skin odour Developmental delay Organic acids in urine sample Encephalopathy Irreversible neurological damage Hypoglycaemia Lactic acidosis Cataract formation Liver/kidney problems Hypotonia Seizures Mitocondrial myopathies Lots e.g. diabetes mellitus and deafness, Leber’s hereditary optic neuropathy Lysosomal storage disorders Various defects in lysosomal function that lead to accumulation of toxic substances Gauncher’s disease Niemann-Pick disease Tay-Sachs disease Present late (adulthood)