Plenary 01: Pediatric Oncology Cases OS 217 Plenary 01: Pediatric
advertisement

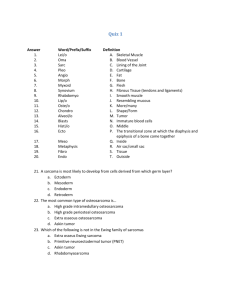
OS 217: Systemic Diseases – Oncology Module Plenary 01: Pediatric Oncology Cases Plenary 01: Pediatric Oncology Case 2 C. Villegas, MD; M.Y. Lesaca-Medina, MD; M. Calaguas, MD; P. Fajardo, MD TOPIC OUTLINE I. II. III. IV. V. VI. VII. September 18, 2014 ( - ) polyuria, polyphagia, polydipsia, tremor ( - ) dizziness, headache, lightheadedness ( - ) arthritis, sprain/strain ( - ) pruritis, bruising, cyanosis, pallor, rashes, clubbing ENDOCRINE History Physical Examination Differential Diagnoses Pathophysiology Work-up Management Comments from Panelists OS 217 1 NEUROLOGIC MSK SKIN E. PAST MEDICAL HISTORY (-) previous hospitalizations and infections Allergy to excessive hamburgers at 8 months old Allergic reaction to diclofenac (NSAID) given to her in one medical mission last May due to persistent leg pain o Presented with difficulty of breathing and skin manifestations (-) Cancer (+) Hypertension (mother) (+) Arthritis (grandfather) (-) DM (-) TB (-) Kidney disease (-) Brain disease Born via CS at a hospital in Camarines Norte 2nd of 5 siblings (-) fetomaternal complications At par with age Currently, 9th grade student enrolled at a home study program – prior to this, patient was a regular high school student at Dasmarinas National High School with average grades Not breastfed and given formula instead Diet consists mostly of vegetables and meat with rice 2 MONTHS PTA (JULY 2014) Complete immunization administered by family paediatrician (EPI: BCG, Hep B, DPT, Measels, OPV) Unrecalled if given booster shots Credits to Block 6 for presenting the case and providing us with their PPT presentation. I. HISTORY ● A.GENERAL DATA J.M., 14 years old Female ○ Student (Grade 9) ○ Roman Catholic ○ Originally from Camarines Sur but resides in Dasmarinas, Cavite. B. CHIEF COMPLAINT Persistent pain on distal left thigh C. HISTORY OF PRESENT ILLNESS G. BIRTH AND MATERNAL HISTORY 4 MONTHS PTA (MAY 2014) Experienced weakness on the left leg after jogging (not induced by trauma) described as “nangangalay, namimintig, iika-ika” Experienced body malaise the next day On the last week of may also started experiening pain on distal left thigh (graded 7/10) described as “makirot”. Pain was non-radiating and lasted 15 minutes per episode. It was sudden in onset and often awakened the patient at night No associated back pain, joint pain, and numbness A palpable mass (2 inches) on the distal left thigh was reported. The mass was pulsating, warm, and non-erythematous. Tried hilot, vicks, and Salonpas but these did not relieve the pain Consultation at UMC Hospital in Dasmarinas o Labs done o Given tramadol and paracetamol (325 mg every 8 hours) to relieve pain. Pain persisted but is relieved by medications Went to PGH for further tests: labs, CT scan, MRI Patient was not able to walk after the biopsy procedure due to the rapidly increasing mass. Consulted at the PGH Orthopedics Department every week. MRI: revealed L distal femoral metaphyseal solid mass suggestive of parosteal osteosarcoma, Ewing sarcoma, primitive neuroectodermal tumor, or lymphoma) 3 DAYS PTA (SEPTEMBER 12 2014) Experienced intermittent febrile episodes of unrecalled temperature (4x in 3 days) o Leg pain was persistent and was not associated with febrile episodes In the interim Experienced difficulty of breathing Noted weight loss (1 peso coin → 25 centavo coin) September 15, 2014 Admitted to Cancer Institute at PGH for chemotherapy (-)Synaptophysin (-)Chromogranin bone marrow scan result is still pending D. REVIEW OF SYSTEMS HEENT RESPIRATORY CARDIOVASCULAR GIT GU YNA – ANGELI - ANTON F. FAMILY HISTORY ( - ) blurring of vision, ringing of ears, ear pain, eye redness ( - ) wheezing, cough, hemoptysis ( - ) chest pain, ortopnea, edema, easy fatiguability ( - ) abdominal pain, jaundice, diarrhea, bloody stools, nausea, vomiting, loss of appetite ( - ) intermittency, hematuria, nocturia, urgency, inocontinence, pain in urination H. DEVELOPMENTAL HISTORY I. NUTRITIONAL HISTORY J. IMMUNIZATION HISTORY K. MENSTRUAL HISTORY Menarche at 11 y/o (Grade 6) Regular menstruation with moderate flow (2 pads per day) lasting for 7 days LMNP 1st week of September L. PERSONAL AND SOCIAL HISTORY The patient is 2nd of 5 siblings (all girls). Father is a truck driver and mother is a housewife (-) Alcohol, smoking, illicit drug use PE classes in school were her only exercise routine before onset of symptoms Living conditions in the province: houses are far apart, no known exposure to environmental toxins and chemicals II. PHYSICAL EXAMINATION BP 90/60 right arm supine, HR 123 bpm, RR 26 breaths/min Temp 36.9°C, Ht: 139.7 cm, Wt: 43 kg, BMI: 22.0 (within normal limits in growth chart) Skin: (-) jaundice, (-) pallor, (-) cyanosis, pink nailbeds, (-) clubbing, CRT < 2 secs HEENT: pink conjunctiva, anicteric sclerae, pink oral mucosa, (-) visible neck masses or distended veins, (-) CLAD Observable mass on left leg around the distal thigh/knee area. (+) tenderness, (-) erythema, (-) discharge, unable to fully extend L leg, superficial vessels/striae Page 1 / 7 Plenary 01: Pediatric Oncology Cases OS 217 III. DIFFERENTIAL DIAGNOSES Rule In Osteosarcoma Rule Out Weakness and pain on left leg No history of injury Palpable mass along metaphysis of distal left thigh Limitation of motion Figure 1. Mass on Distal Knee Intermittent fever 23 cm span (half circumference) 39 cm base circumference 6 cm elevation 8 cm longest diameter Body malaise Weight loss CARDIO-RESPIRATORY Inspection: (-) chest wall deformities, adynamic precordium, (-) chest retractions, (-) alar flaring, (-) use of accessory muscles, but with noted tachypnea (RR 26 breaths/min) Palpation: (-) tenderness or masses on the chest, (-) heaves or thrills, point of maximal impulse at 5th ICS MCL, equal and symmetrical tactile fremitus, symmetrical chest expansion Auscultation: tachycardic (HR 123 bpm) with regular rhythm, clear distinct heart sounds, (-) murmurs, apex beat at 5th ICS MCL, (-) abnormal breath sounds Ewing Sarcoma Most common primary malignant bone tumor in children and adolescents Pain on left leg with nighttime awakening Palpable mass at distal left thigh Characteristic location (diaphysis of long bones and flat bones) Age (usually <10 y/o) Limitation of motion ABDOMINAL Inspection: Abdomen does not appear distended. (-) flank bulges, (-) masses or organs visible, (-) scars, (-) striae, (-) dilated veins. Umbilicus is midline, neither depressed nor everted. Palpation: (-) abdominal tenderness on light palpation, (-) abdominal tenderness on deep palpation, (-) masses, liver edge not palpated Auscultation: normoactive bowel sounds (13/min/quadrant) Percussion: liver span = 7 cm Splenic Percussion Sign and CVA Tenderness were not assessed. Intermittent fever Body malaise Weight loss Second most common primary malignant bone tumor in children and adolescents MUSCULOSKELETAL Upper Extremities: o Muscles were symmetrical and without any observable atrophy, hypertrophy, involuntary movements, fasciculations, joint contractures or postural tremors. o Muscle Tone and Strength: (-) spasticity/rigidity, Grade of 5/5 for shoulder abduction, elbow flexion and extension, wrist flexion and extension. 4/5 for finger extensors and finger abductors of both hands, 4/5 for finger flexor of left arm. 5/5 for the other hand and finger muscles. o Light touch Sensation: intact and symmetric (R to L, proximal to distal) o Pain Sensation: intact and symmetric (R to L, proximal to distal). But not able to differentiate dull from sharp in C6 of right arm. o Position sense: intact for both left and right. Lower Extremities: o Not tested because of painful mass in left leg. o (+) L knee/distal thigh swollen mass spanning 23 cm, (-) erythema, (+) tenderness, (-) discharge, unable to extend L, superficial vessels/striae o Light touch Sensation: intact and symmetric (R to L, proximal to distal) o Pain Sensation: intact on right and left sides (left side was not tested but patient reported pain from the mass) o Position sense: intact for both. NEURO: CRANIAL NERVES CN I: Not tested but no complaints on olfaction. CN II: Visual acuity OD 20/20 -2, OS 20/20 -3. (-) visual field cuts CN II and III: Pupils symmetric in size. Consensual and direct reflexes were intact. CN III, IV, VI: Full range of motion for EOMs, good accommodation, (-) nystagmus CN V: Intact and symmetrical pain and light touch sensation for ophthalmic, maxillary, and mandibular nerves. Strength grading of 5/5 for muscles of mastication. CN VII: Intact facial nerve, (-) asymmetry, (-) spasms, (-) facial weakness, taste sensation not tested CN VIII: Rinne BC>AC both ears. (-) lateralization in Weber. CN IX and X: Able to phonate. (-) dysphagia. Gag reflex not tested. CN XI: Strength grading 5/5 and symmetrical SCM and trapezius muscles. CN XII: Tongue is midline, (-) atrophies, (-) fasciculations. Grade 5/5 YNA – ANGELI - ANTON Osteomyelitis Pain on left leg No draining sinus tract Palpable warm mass at distal left thigh No fever at onset of symptoms Intermittent fever 4 months duration Characteristic location (metaphysis of long bones) Tachycardia, tachypnea Benign Bone Tumors Pain on left leg (osteochondroma, osteoblastoma, osteoid osteoma, fibroma etc.) Palpable mass distal left thigh Limitation of motion at Intermittent fever Body malaise Characteristic location (metaphysis of long bone e.g., distal femur, proximal humerus, proximal tibia) Weight loss One of the most common benign tumors in children Soft Tissue Tumors (rhabdomyosarcoma, non-rhabdomyosarcoma) Pain on left leg Palpable mass distal left thigh at Page 2 / 7 Plenary 01: Pediatric Oncology Cases Most common pediatric soft tissue sarcoma (usually < 20 y/o) Lymphoma Weakness and pain on left leg OS 217 V. WORK UP Diagnostic Pivot: Bone pain with or without swelling No CLAD No hepatomegaly Bone cyst (e.g. aneurismal bone cyst) Weight loss Weakness and pain on left leg Palpable mass distal left thigh at Limitation motion of No associated neurologic symptoms or spinal involvement Reactive lesion of bone seen in <20 y/o Characteristic location (femur, tibia, spine) Histiocytosis Progressively growing, expansile lesion Pain on left leg (e.g. Eosinophilic granuloma) Characteristic (skull) location Age group (5-10 yrs.; mean age of 5.5 yrs.) IV. PATHOPHYSIOLOGY Primary Working Impression: OSTEOSARCOMA on distal left femur to rule out SOFT TISSUE MALIGNANCY • • Osteosarcoma is the most common primary bone malignancy, with a high incidence in children and adolescents Tumors most often arise in the long bones from osteoid-producing neoplastic cells near the growth plates The most common sites include: o Femur (42%, most in the distal femur) o Tibia (19%, most in proximal tibia) o Humerus (10%, most in proximal humerus) Interplay between genetic and environmental factors Genetic cause largely unknown but research shows: o Mutations involving p53 and Rb gene o High level of chromosomal instability microsatellite instability (MIN) CpG island methylator phenotype (CIMP) o Unstable telomere maintenance Females- shorter telomere length > inc. risk o Lack of Sprouty2 protein expression Increased cell proliferation and migration o Human P2X7 receptor expression P2X7RA and truncated P2XRB7 are powerful stimuli for growth o Increased calcium mobilization and enhanced NFATc1 activity stimulate growth and metastasis Certain genetic and acquired conditions (hereditary retinoblastoma, Li-Fraumeni syndrome, Rothmund-Thomson syndrome) predispose patients to development of osteosarcoma. Known environmental risk factors o Radiation exposure o Methylcholanthrene o Chromium salts o Beryllium oxide o Zinc beryllium silicate o Aniline dyes o Asbestos YNA – ANGELI - ANTON STAGING AND RISK ASSESSMENT Definitive diagnosis requires histological examination of tumor material obtained by open biopsy performed by an orthopedic oncologist Primary tumor must be evaluated by plain radiographs (X-ray) in two planes MRI is the most useful to evaluate intramedullary and soft tissue extension of osteosarcoma and its relation to vessels and nerves Chest X-ray (10% negative) or CT scan to check for lung metastases o Cannonball-like lesions on CXR, nodules on CT scan Radionuclide bone scan or skeletal survey (X-ray) to check for bone metastases PLAIN RADIOGRAPH Osteosarcoma o Sclerotic destruction (less commonly lytic) o “Sunburst pattern” Page 3 / 7 Plenary 01: Pediatric Oncology Cases Ewing Sarcoma o Primarily lytic o Multi-laminar periosteal reaction o “Onion-skinning” OS 217 Taken 8/2/14 (UPMC) Fairly defined 10.6 x 8 x 6.7 mass arising from the medial and posterior cortical aspects of the distal femoral metaphysis associated with periosteal upliftment as well as abnormal marrow signals. o Suggestive of parosteal osteosarcoma, Ewing sarcoma, PNET, or lymphoma Myositis, edema of the vastus medialis and biceps femoris muscles Abnormal intrasubstance signals in the popliteus tendon (tumor infiltration or partial tear) The rest of the musculature, bones, subcutaneous fatty layer, superficial veins, acetabulofemoral and tibiofemoral joints are unremarkable. CHEST CT-SCAN PLAIN Taken 9/10/14 (Cavite) There are hazy and patchy densities seen in the superior segment of the right lower lobe. There is subcentimeter nodular density seen in the antero-basal segment of the left lower lobe abutting the lateral pleura. No evident enlarged lymph nodes. No pleural effusion nor atelectasis noted. The heart and blood vessels are normal. The tracheo-bronchial tree is patent with no intraluminal lesions evident. Additional sections of the liver and adrenal glands reveal no focal lesion. The rest of the soft tissues and osseous structures are intact. ASSESSMENT Angiography can assist in surgical planning and estimate response of tumor to preoperative chemotherapy o High-grade tumor = ↑ vascularity = ↑ contrast enhancement o Enhancement referred to as “tumor blush” o Disappearance of tumor vascularity after preoperative chemotherapy correlates with good treatment response See Appendix I for Radiologic Studies used in the Evaluation of Osteosarcoma and Detection of Mets Alkaline phosphatase (30%) and lactate dehydrogenase (40%) are elevated levels correlate with poor prognosis Before interdisciplinary treatment, assessment of organ function and general health must be performed including complete blood count (CBC) with differential count, blood group typing, coagulation profile, renal and liver function test as well as hepatitis and HIV testing Before chemotherapy, baseline assessment of cardiac and auditory function including echocardiogram or radionuclide ventriculography and audiogram LABORATORY FINDINGS See Appendix II for complete laboratory findings tables. DIAGNOSIS OSTEOSARCOMA (Stage IVa) on distal left femur with PULMONARY METASTASIS VI. MANAGEMENT MRI Determine: Intraosseous vs extraosseous tumor extension Neurovascular bundle identification SURGERY Primary objective is to achieve long-term disease-free survival while preserving limb function as much as possible o Limb-sparing/limb-salvage operation If limb-sparing resection cannot be performed amputation should be considered Multimodal treatment of high-grade osteosarcoma increases disease-free survival probabilities from only 10-20% to >60% CHEMOTHERAPY YNA – ANGELI - ANTON Doxorubicin, cisplatin, high-dose methotrexate with leucovorin rescue and ifosfamide Standard protocol: Doxorubicin + cisplatin +/- methotrexate Preoperative chemotherapy (Neo-adjuvant therapy) o Induce tumor necrosis of primary tumor o Treatment of micrometastasis o Facilitates surgical resection with wide margins o Prognostic factor Page 4 / 7 Plenary 01: Pediatric Oncology Cases OS 217 REHABILITATION Early prosthetic fitting and gait training Patient information and counseling Monitor for local and systemic recurrence o History and PE plus imaging of extremity and chest Every 3 months for the first two years At least every 6 months from the 2nd to 5th years Yearly after the five years o Annual bone scan for the first two years Long-term effects of chemotherapeutic agents o Fatal: Cardiotoxicity from anthracycline FOLLOW-UP PROGNOSIS Surgical resection alone is curative only for parosteal osteosarcoma patients Conventional osteosarcoma requires multi-agent chemotherapy o 5-year survival of patients with nonmetastatic extremity osteosarcoma is 65-75% with chemotherapy and surgery o Up to 75% with nonmetastatic extremity osteosarcoma are cured o Prognosis not favorable for pelvic tumors 20-30% with pulmonary metastases can be cured with aggressive chemotherapy and lung nodule resection Late isolated lung metastases may be cured with surgical resection alone Bone metastases and widespread lung metastases have poor prognosis VII. COMMENTS FROM PANELISTS From Dr. Villegas: I would amputate this patient for pain relief, this would also decrease the tumor burden for chemotherapy despite being stage IV, to improve the quality of life the remaining days of the patient. From Rad Onco: Proper treatment for this is still surgery. Radio oncologists are always the last to be consulted if necessary, or in cases where there are positive or close margins or the osteosarcoma is not responsive to other modalities. From Pedia Onco: o Include in your PE the Visual Pain Assessment Scale o Note that after the first day of chemo the patient will feel relief of pain and there will be control of Angiogenesis o You should probably also refer the patient and her family to hospice care o Try adding TB or TB joint to your differential diagnosis In TB joint you find mass, bone involvement, calcifications, soft tissue swelling and cold joints (painless) o What do you find on Xrays showing osteomyelitis? You find sequestrum, new bone formation and you may find a characteristic bowing of the knees known as saber shin o In bone tumors we usually see periosteal reaction wherein a new layer of bone forms and codman triangle, which is the new subperiosteal bone that is formed when a tumor raises the periosteum from the bone; these signs however are not specific to tumors o Note that in this patient palliative care is being given, thus, only 60% of the treatment regimen is being given to prevent neutropenic fever. END OF TRANSCRIPTION YNA – ANGELI - ANTON Page 5 / 7 Plenary 01: Pediatric Oncology Cases OS 217 APPENDIX I APPENDIX II: COMPLETE LABORATORY FINDINGS Taken 9/10/14 (Cavite) Exam Name CBC WBC Hemoglobin Hematocrit Platelet Differential Count Neutrophil Lymphocyte Monocyte Eosinophil Basophil Creatinine ALT Total Bilirubin Direct Bilirubin Indirect Bilirubin Albumin Calcium Magnesium Sodium Potassium YNA – ANGELI - ANTON Ref. Value Result 4 - 11 115 - 148 0.38 - 0.44 150 - 400 15.6 109 0.32 580 0.55 - 0.65 0.25 - 0.35 0.03 - 0.06 0.02 - 0.04 0.00 - 0.01 0.69 0.21 0.06 0.01 0.00 3.4 - 20.5 0.0 - 8.6 3.4 - 11.9 3.5 - 5.1 0.66 - 1.07 136 - 145 53 - 97 0 - 55 35 - 50 2.23 - 2.5 52.4 123 13.5 9.7 3.8 33 2.23 0.86 138 3.2 Unit x 109/L g/L Interpretation High Low Low High High Low Low umol/L IU/L umol/L umol/L umol/L g/L mmol/L mmol/L mmol/L mmol/L Low High High Low Page 6 / 7 Plenary 01: Pediatric Oncology Cases OS 217 Taken: 9/15/14 (UP-PGH) Exam Name CBC WBC RBC Hemoglobin Hematocrit MCV MCH MCHC RDW Platelet Differential Count Neutrophil Lymphocyte Monocyte Eosinophil Basophil Creatinine ALT Total Bilirubin Albumin Calcium Magnesium Sodium Potassium Urinalysis Color Specific Gravity Transparency pH Sugar Protein Microscopic RBC WBC Epithelial Cells Bacteria Mucus Thread Cast Crystals Special Bilirubin Urobilinogen Ketone Leucocytes Nitrite Blood YNA – ANGELI - ANTON Ref. Value Result Unit Interpretation 4.5 - 11 4.2 - 54 120 - 160 0.38 - 0.47 80 - 96 23 - 31 320 - 360 11 - 16 150 - 450 12.79 4.11 108 0.34 83.1 26.4 318 12.2 491 x 109/L x 1012/L g/L High Low Low Low 0.50 - 0.70 0.20 - 0.50 0.02 - 0.09 0.00 - 0.06 0.00 - 0.02 0.67 0.26 0.06 0.01 0.00 27 - 88 8 - 32 5.1 - 20.5 31 - 48 2.24 - 2.58 0.7 - 1 132 - 143 3.4 - 5.4 50 141 11.2 23 2.06 0.91 136 3.4 fL pg g/L Low Low x 109/L High umol/L IU/L umol/L g/L mmol/L mmol/L mmol/L mmol/L High Low Low Yellow orange 1.015 Hazy 7.0 +1 1-3 25 - 30 Few +4 Occasional - /hpf /hpf /hpf /hpf /hpf +1 +1 Trace Page 7 / 7