Chapter 4 Notes
advertisement

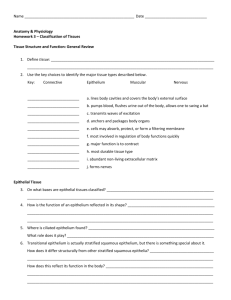
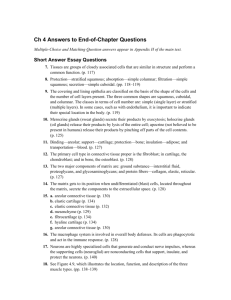
Anatomy/Physiology Chapter 4 Tissues Epithelial Tissue: (epithelium) A sheet of cells that covers a body surface or lines a body cavity. (epithe = laid on or covering) 1. Covering and lining epithelium: forms outer layer of the skin, dips into and lines the open cavities of the cardiovascular, digestive, and respiratory systems, and covers the walls and organs of the closed ventral cavity. 2. Glandular: covers the glands of the body Epithelia form boundaries between different environments. Ex. epidermis of the skin separates the inside from the outside of the body. Also, the epithelium lining in the bladder separates the bladder wall from the urine. As an interface tissue epithelium has many functions: 1. Protection 2. Absorption 3. Filtration 4. Excretion 5. Secretion 6. Sensory reception Epithelial tissue characteristics: 1. Polarity: all epithelia have an apical surface, an upper free surface exposed to the body exterior or the cavity of an internal organ, and a lower attached basal surface. All epithelia exhibit apical/basal polarity, the cell regions near the apical surface differ from those near the basal surface in both structure and function. Most apical surfaces have microvilli which give them a “fuzzy” appearance (brush border). Some epithelia (lining of the trachea) have cilia. Lying next the basal surface is the a supporting sheetbasal lamina. 2. Specialized contacts: epithelial cells fit close together to form continuous sheets (except for glandular epithelia). Adjacent cells are bound together at many points by lateral contacts, including tight junctions and desmosomes. Tight junctions help keep proteins in the apical region of the plasma membranes from diffusing into the basal region helping it to maintain its polarity 3. Supported by connective tissue: all epithelial tissue rests upon and is supported by connective tissue. Just deep to the basal lamina is the reticular lamina (layer of extracellular material containing a fine network of collagen fibers. Together the two lamina make up the basement membrane which reinforces it to resist stretching and tearing forces defining the epithelial boundary. 4. Avascular but innervated. (contains no blood vessels but does have nerves). It is nourished by substances diffusing from blood vessels in the underlying connective tissue. 5. Regeneration: epithelium has high regenerative capacity. If and when their apical-basal polarity and their lateral contacts are destroyed, they begin to regenerate themselves rapidly through cell division. Classification of epithelia: Simple epithelia: composed of a single layer of cells (usually very thin), concerned with absorption, secretion and filtration Stratified epithelia: consisting of 2 or more layers of cells (stacked on top of one another) common in high abrasion areas where protection is important. They regenerate from below, the basal cells divide and push apically to replace the older surface cells. It is more durable than simple epithelia. Major role is protection. 3 common shapes: (both simple and stratified) Squamous, flattened or scale-like (squam= scale) nucleus is flat and disk like Cuboidal: are boxlike – approx. as tall as they are wide. The nucleus is spherical Columnar: are tall and column shaped. Nucleus is elongated and near the base of the cell Transitional: These “transitional cells” can change their shape (transition) to allow for greater elasticity. They form the lining of hollow urinary organs which stretch as they fill with urine. To help identify the cell types keep the nucleus shape in mind. (see pages 120-124) Glandular Epithelia: A gland consists of one or more cells that make and secrete (export) a particular product. The product is called a secretion is a water based (aqueous) fluid that usually contains proteins but can release lipids or steroids. Glands are classified as endocrine (internally secreting) or exocrine (externally secreting) depending on where they release their product. Endocrine glands: They eventually lose their ducts and are called “ductless glands” secreting hormones by exocytosis directly into the extracellular space. The hormones then enter the blood or lymphatic system and travel to their target organs. Exocrine Glands: They secrete their products directly onto the body surfaces (skin) on into the body cavities. They include: mucous, sweat, oil, and salivary glands, the liver (bile), the pancreas (digestive enzymes) and others. Modes of secretion: (most multicellular exocrine glands) Merocrine glands secrete their products by exocytosis. The secretory cells are not altered in any way. The pancreas, sweat and salivary glands belong to this class. Holocrine glands accumulate their products within them until they rupture (they are replaced by underlying cells). They “die for their cause” ex. Sebaceous (oil) glands in the skin Connective Tissue: Found everywhere in the body. It is the most abundant and widely distributed of the primary tissues. 4 main classes: 1. connective tissue (proper) which includes fat and fibrous tissue of ligaments 2. cartilage 3. bone tissue 4. blood Major functions: 1. binding and support 2. protection 3. insulation 4. transportation (blood) of substances within the body Common Characteristics: 1. Common origin: connective tissue arises from mesenchyme (embryonic tissue) so they have a common kinship 2. Degrees of vascularity, cartilage is avascular, dense connective tissue is poorly vascularized while other types have a rich supply of blood. 3. Extracellular matrix, connective tissues are largely composed of extracellular matrix (non-living). Because of this connective tissue can bear weight, withstand great tension, and endure abuses (physical trauma and abrasion) Structural elements of connective tissue: 3 main elements: 1. ground substance 2. fibers 3. cells Ground substance and fibers make up the extracellular matrix. The properties of the cells and the arrangement of the matrix elements vary tremendously providing an amazing diversity of connective tissues. The common structural plan is called areolar connective tissue. Ground substance is unstructured material that fills space between the cells and contains fibers. It is composed of interstitial (tissue) fluid, cell adhesion proteins, and proteoglycans. Fibers provide support. 3 types; 1. Collagen fibers, made of collagen, provide high tensile strength to the matrix they have a white appearance “white fibers” 2. Elastic fibers, made up of a rubber like protein elastin. Yellowish appearance “yellow fibers” stretch like a rubber band. Found in the skin and lungs and blood vessel walls. 3. Riticular fibers, are short fine collagenous fibers (slightly different chemistry and form) they are continuous with collagen fibers. They surround the small blood vessels and support the soft tissue of organs. Cells: each major class of connective tissue has a fundamental cell type that exists in immature and mature forms. Undifferentiated cells, indicated by the suffix “blast” are actively mitotic cells that secrete the ground substance and fibers of their particular cells. The primary blast cell types: 1. Connective tissue proper – fibroblast 2. Cartilage – chondroblast 3. Bone – osteoblast 4. Blood – hematopoietic stem cell (this does not form the matrix like the others) Once they synthesize the matrix, they mature and become less active. They are identified by the suffix “cyte” Connective tissue is also home to other cells: White blood cells: neutrophils, eosinophils, lymphocytes Mast cells and macrophages; concerned with tissue response to injury Mast cells act as sentinels to detect foreign substances (bacteria, fungi) and initiate local inflammatory response against them. Macrophages: (macro = large, phago = eat) Phagocytize foreign materials and dead tissue cells. They can be “fixed” in connective tissue or migrating throughout the matrix Types of connective tissue: All classes of connective tissue consist of living cells surrounded by a matrix. Mature connective tissues come from a common embryonic tissue called Mesenchyme Connective Tissue Proper: has 2 subclasses: Loose connective tissue: areolar, adipose, and reticular Dense connective tissue: dense regular, dense irregular, and elastic. Except for bone, cartilage, and blood, all mature connective tissues belong to this class Areolar Connective Tissue: Functions: (share by some but not all connective tissues) 1. Supporting and binding other tissues (the job of the fibers) 2. Holding body fluids (the ground substance role) 3. Defending against infection (via activity of WBC’s and macrophages) 4. Storing nutrients as fat (in fat cells) Areolar connective tissue is the most widely distributed connective tissue in the body. It serves as a kind of universal packing material between other tissues. Adipose (fat) Tissue: Similar to areolar tissue in structure and function but has a greater nutrient storage capacity. Usually accumulates in subcutaneous tissue and acts as a shock absorber, insulation, and energy storage sites. Reticular Connective Tissue: Limited to certain sites, forms a labyrinth-like stroma (“bed”or “mattress”) an internal framework that supports free blood cells (mostly lymphocytes) in the lymph nodes, spleen, and bone marrow. Dense Regular Connective Tissue (fibrous connective tissue) Enormous tensile strength, they form tendons which attach muscles to bones, muscles to other muscles (aponeuroses) and fascia (fibrous membrane that wraps around muscles, groups of muscles blood vessels, and nerves. Like plastic wrap. Dense Irregular Connective Tissue: Found in the skin (dermis), forms fibrous joint capsules and coverings that surround some organs (kidneys, bones, cartilages, muscles and nerves) Cartilage: Tough and flexible, providing resilient rigidity to the structures it supports. Lacks nerve fibers and is avascular. Composed of up to 80% water, this enables the cartilage to rebound after compression. 3 types of Cartilage: Hyaline Cartilage (most abundant in body) covers the ends of long bones, tip of the nose, connects ribs to sternum, and supports most of the respiratory system passages. Most of the embryonic skeleton before bone is formed. Elastic Cartilage: elastic fibers, forms the “skeleton” of the external ear and the epiglottis. Exceptional strength and stretchability Fibrocartilage: compressible and tension resistant Intervertebral disks and spongy cartilage of the knee Bone (osseous tissue) support and protect body structures. Provides cavities for fat storage and blood cell synthesis. Along with collagen fibers the matrix also contains (inorganic) calcium salts. Osteoblasts produce the organic portion of the matrix. Osteocytes (mature bone cells) reside in the lacunae (small space within bone or cartilage) within they have made. Blood: The most atypical connective tissue. It is classified as connective tissue because it comes from mesenchyme and consists of blood cells, surrounded by a non-living fluid matrix called blood plasma. The vast majority of blood cells are RBC’s the fibers of the blood are soluble protein molecules (aide in blood clotting). Function of blood: transportation of nutrients, wastes, respiratory gases, and other substances throughout the body. Nervous tissue: The main component of the nervous system (brain, spinal column, nerves which regulate and control body functions. Neurons: highly specialized nerve cells that generate and conduct nerve impulses. Typically, they are branching cells with extensions or processes. These allow them to respond to stimuli (role of the dendrites) and to transmit electrical impulses over substantial distances in the body (role of the axons). These processes can be very long and myelinated (covered with a fatty sheath – think insulated wire) that increases the speed of transmission. Muscle Tissue: Highly cellular, well-vascularized tissues responsible for most types of body movement. They possess myofilaments (actin and myosin filaments) that cause movement or contraction in all cell types. 3 Types of muscle tissue: Skeletal Muscle: attached to bones of the skeleton. Make up the flesh of the body.. when they contract, they pull on the bones or skin causing movement. Skeletal muscle cells (also called muscle fibers) are long, multinucleated cylindrical cells. They have a striated (banded) appearance reflecting the precise alignment of their myofilaments. Cardiac Muscle: Found only in the wall of the heart. They are striated (like skeletal muscle) in appearance and help propel the blood though the blood vessels. They only have one nucleus, are branching cells that fit together tightly at junctions called intercalated discs. Smooth Muscle: Named because their cells have no visible striations. They are spindle shaped with one nucleus. Found mainly in the walls of hollow organs (other than the heart). It functions to squeeze substances through these organs by contracting and relaxing. Voluntary muscle: Skeletal muscle because we have conscious control over them. Involuntary muscle: cardiac and smooth Covering and lining membranes: 3 types: Cutaneous, mucous, serous All are continuous multicellular sheets composed of epithelium fused to a sheet of connective tissue proper. These membranes are simple organs. Cutaneous membranes: consists of 2 layers, the epidermis (keratinized squamous epithelium) attached to the dermis (dense irregular connective tissue). It is exposed to the air and is a dry membrane. Mucous Membrane: (mucosae) line the body cavities that open to the exterior (hollow organs of the digestive, respiratory and urinary tracts). They are “wet” membranes bathed in secretions. Adapted for absorption or secretion. Serous Membrane: (serosae) moist membranes found in closed ventral cavities. They are named for their site and specific organ associations: Pleura- lining the thoracic cavity and lungs; Pericardium – enclosing the heart; peritoneums – lining the abdominopelvic cavity and organs. Tissue repair: 3 steps: 1. Inflammation – the release of mast cells and macrophages and inflammatory chemicals. This causes blood vessels to dilate and diffuse WBC’s and clotting proteins and antibodies to the injured area. 2. Organization – blood clot is replaced by granulation tissue. A delicate pink tissue composed of capillaries that grow in from nearby areas. Granulation tissue becomes scar tissue is highly resistant to infection because it produces bacteria inhibiting substances. Once enough matrix has accumulated in the area, fibroblasts revert to a resting state or undergo apoptosis 3. Regeneration and fibrosis – during organization, the epithelium starts to regenerate (growing under the scab). As fibrous tissue matures and contracts, it thickens until it resembles the surrounding skin. The end result is a fully regenerated epithelium and an underlying scar which may or may not be visible. Regenerative capacity of different tissues: Epithelial tissues, bone, areolar connective tissue, dense irregular connective tissue, and blood forming regenerate extremely well. Smooth muscle, and dense regular connective tissue have moderate capacity to regenerate, and skeletal and cartilage have weak capability for regeneration. Cardiac and nervous tissues have virtually no functional regenerative capacity and are routinely replaced with scar tissue. Developmental aspects of tissues: In embryonic development, one of the first events is the formation of three primary germ layers (lie on top of one another like pancakes) Ectoderm, mesoderm and endoderm. These primary layers specialize to form the 4 primary tissues from which all body organs are derived.