Cutaneous nerves of the arm and forearm
advertisement

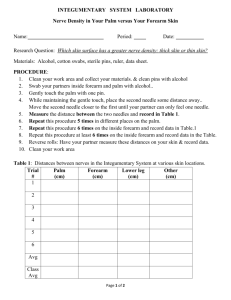
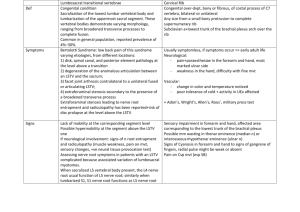
Cutaneous nerves of the arm and forearm - how small can we go ? The introduction of Ultrasound guidance for nerve blocks has revolutionised regional anaesthesia practice over recent years, improving success rate, reducing procedure time and volume required to achieve a successful nerve block. Advancing US technology has improved resolution capabilities of portable US machines and has allowed practitioners to identify not only the main plexus anatomy, but also smaller components of nerve plexus and individual peripheral nerves, which were previously beyond reliable detection. This has also sparked a renewed interest in peripheral functional anatomy and improved our understanding of nerve territories and innervations of peripheral structures. Clinical practice can be adapted using this understanding and achieve more selective peripheral nerve blockade to minimise undesired block effects and maximise analgesia. This presentation will focus on the anatomy of smaller nerves of the arm and forearm and discuss block approaches for a variety of applications. Medial cutaneous nerve arm (MCNA)/ Intercostobrachial nerve: The MCNA arises from the median cord and communicates closely with the intercostobrachial nerve to innervate the median aspect of the upper arm. It pierces the deep fascia covering the axillary blood vessels and main plexus nerves at midhumeral level and branches into a number of smaller nerves. Its block is required for cubital tunnel release. It is best approached at the high axillary block at the level of the conjoint tendon with a combined subcutaneous infiltration superficial and deep to the deep fascia. Medial cutaneous nerve of forearm (MCNF): Together with the medial cutaneous nerve of the arm (MCNA) the MCNF is formed off the medial cord off the lower trunk and in the axilla is closely associated to the ulnar nerve. It travels towards the elbow following the basilic vein and branches into a palmar and volar nerve supplying the palmar and volar ulnar aspect of the forarm. Both nerves remain close to the basilic vein until they reach the elbow crease where they travel over the anterior aspect of the medial epicondyle. Blockade of the nerve, often difficult to achieve with blocks above the clavicle, is required for surgery on the ulnar aspect of the forearm such as ulnar plating, ulnar shortening or skin grafting. The nerve or its branches can be identified on US by moving the transducer at the lower third of the humerus from the brachial artery and median nerve towards the triceps muscle, releasing the transducer pressure to reveal the basilic vein where the main nerve or its branches tend to be on the 3 and 9 o’clock position of the vein. The ulnar nerve is seen further on related to the triceps muscle. Blockade of the MCNF is most reliably achieved at this level, which also allows median and ulnar nerve to be blocked with one needle approach. The branches of the MCNA are often seen in the superficial subcutaneous layer. (Pic 1) Lateral cutaneous nerve forearm (LCNF): The musculocutaneous nerve arises from the lateral cord of the brachial plexus and travels between long head of biceps and coracobrachialis muscle. It gives motor supply to the biceps and brachialis and continues between these two muscles moving towards the lateral aspect of the arm. At this point the nerve continues as the lateral cutaneous nerve of forearm. At the elbow crease the LCNF pierces the brachial fascia lateral to the biceps tendon and comes to lie next to the cephalic vein, between brachioradialis muscle lateral and biceps tendon (medial). It divides into an anterior and a posterior branch, with 30% dividing proximally and 70% distally. The nerve supplies skin on the lateral aspect of the forearm from the elbow to the base of the thumb. It’s territory overlaps with the superficial radial nerve at the wrist and the medial cutaneous nerve forearm on the anterior aspect of the forearm. Blockade of the nerve is vital for operations on the radial aspect of the forearm such as arteriovenous fistula formation, radial plating, trapezectomy or De Quervains release. Advantages of blocking the nerve distal to the motor nerve is the preservation of biceps function and reduction of LA required to achieve longer lasting sensory block. It is most reliably found at the elbow and can be blocked together with the deep and superficial radial nerve in one approach. Due to its smaller size 1-2 ml of LA are sufficient and give a quick onset block. During the needle approach from lateral a ‘give’ needs to be appreciated as the needle leaves the brachioradials muscle fascia to lay lateral to biceps muscle and next to cephalic vein. Posterior cutaneous nerve of forearm (PCNF): The PCNF is a branch off the radial nerve which it follows through the spiral groove of the humerus to the lateral aspect of the arm, where the PCNF pierces the lateral intermuscular septum to lie in the subcutaneous layer. It divides into various branches to innervate the posterior aspect of the forearm. It’s main branch or branches can be found over the prominence of the brachioradialis muscle at the level of the elbow. In muscular individuals the nerve will be flat on the muscle fascia, in more adipose patients is more clearly seen among subcutaneous fatty tissue. It requires to be blockes specifically for procedures on the posterior aspect of the forearm such as ganglion removals, wrist arthroscopy. It can be blocked with one needle puncture together with the radial nerve and LCNF. Superficial radial nerve: As one of the two endbranches of the superficial radial nerve (SRN) separates from the main radial nerve at the level of the elbow and continues under the brachioradialis muscle towards the wrist. It is closely associated with the radial artery, placed in a triangular space radial to it. It emerges from under brachioradials muscle on the volar aspect of the forearm close to the wrist and divides into two smaller branches to innervate the base and radial aspect of the thumb via the digital nerve and volar radial aspect of the hand. It communicates with the LCNF and volar branch of ulnar nerve. It rarely requires blockade on it’s own (eg. Dupuytrens affecting the first web space) and is usually blocked together with the deep radial nerve at the elbow or above. On US it can be followed from the elbow under brachioradialis muscle distally to its smaller branches and may blocked in one needle pass with the median nerve. Posterior interosseous nerve (PION): As the radial nerve branches into deep and superficial radial nerve, the deep radial nerve continues as the main motor branch for the extensor muscles of the forearm and passes through the supinator tunnel (Ligament of Frohse) where it becomes the PION. The PION descends onto the interosseous membrane, at the wrist in a mirror position to the anterior ION, both of which supplying the wrist joint and MCP Joints. The PION can be identified at the supinator tunnel, after which it becomes more difficult to follow, however, it can be blocked on the interosseous membrane further distally. The main application for PION block is for chronic pain syndromes such as chronic wrist pain, potentially also for CRPS, or as a diagnostic block at the supinator muscle to confirm radial tunnel syndrome. Anterior interosseous nerve (AION): The AION branches off the median nerve where it passes through the heads of pronator teres muscle at the elbow. It accompanies the IO artery on the interosseous membrane, supplies the deep flexors of the forearm and pronator quadratus muscle at the wrist. It needs to be blocked together with the PION for surgery on the wrist joint or MCP joints. It can be identified on US in the forearm next to the IO artery. Thereby it can be approached in the forearm and combined with a median nerve block instead of blocking the main nerve above the elbow, allowing a quicker onset of block. Digital nerves: The digital nerves, formed by median and ulnar nerve, can be identified on each side of the flexor digitorum superficialis tendons un der the palmar aponeurosis in the palm of the hand for surgery on individual fingers. At this point a hockey stick probe will be required. Discussion: It is possible to identify smaller nerves in the upper limb on US. There is a degree of variability and communication which limits block approaches to the main part of these smaller nerves in order to provide appropriate anaesthesia. Several objectives need to be balanced to achieve a patient centred outcome. - The need for tourniquet block during surgery. This can be achieved either with a separate block using short acting LA to minimise motor block duration after surgery or as a single injection to cover both tourniquet and postoperative analgesia requirements. The latter option will lead to prolonged and unnecessary motor block when long acting LA is used. - Several injections versus single injection: For a complete forearm block 5 nerves require to be blocked, in addition a tourniquet block needs to be considered. Radial nerve, LCNF and PCNF can be blocked with one needle approach at the elbow, first approaching RN and LCNF, then reversing the needle direction for the PCNF. Ulnar, median and MCNF can be blocked with one approach at midhumeral level. Depending on site of surgery more distal approaches are feasible, eg median and ulnar nerve for Dupuytrens surgery with shortacting tourniquet block. In the experience of the author, who performs first distal blocks, then tourniquet block, the majority of patients tolerate the procedure very well and prefer to gain motor function shortly after surgery whilst having longer lasting analgesia. - Frequency of blocks performed. It may be unrealistic to maintain the expertise required to perform peripheral nerve blocks for only the occasional list. - Blocking too little too distal. It is imperative to know the surgeon operating to avoid missing overlapping nerve territories or different incisions from expected. If in doubt a more proximal block will be more appropriate. - More injections, higher risk: The practice of differential regional blocks requires appropriate training in US guidance and remains a high skilled application to minimise risk of nerve injury and procedure discomfort to the patient. If peripheral blocks are performed, doing so before a tourniquet block adds to safety, speeds up onset of the most important part of the anaesthetic and allows testing of the block before tourniquet block may cloud assessment. Summary: US guidance allows reliable identification of peripheral nerve structures for more selective and differential regional anaesthesia for surgery of the upper limb. This also has applications for chronic pain medicine. This practice requires a highly skilled practitioner to provide safe and reliable anaesthesia. Pic 1: transverse scan just above the elbow with Median Nerve (MN) next to brachial artery (BA), MCNF at 3 o’clock of Basilic Vein (BV) and Ulnar Nerve (UN) on surface of triceps muscle. Pic 2: Superficial and Deep Radial Nerve under Brachioradialis Muscle, lateral cutaneous nerve (LCN) under Cephalic Vein (CV) and Median Nerve (MN) under Brachial Artery (BA) between heads of Pronator Muscle.