Equipment available in room
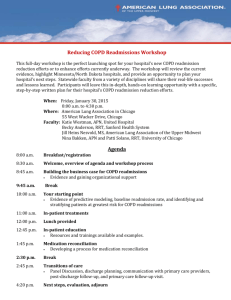
advertisement

Minnesota Simulation in Healthcare Education Professionals (M-SHEP)
Respiratory Distress Simulation
68 year old male patient admitted with an exacerbation of his COPD
Date:
Discipline:
Expected Simulation Run Time:
Location:
Admission Date: Today’s Date:
Brief Description of Patient:
File Name:
Student Level:
Debrief /Guided Reflection Time:
Location for Reflection:
Psychomotor Skills Required prior
to simulation:
Name: Roger Elofson Gender: M Age: 68
Weight: ____kg
Height: ____cm
Religion:
Major Support:
Phone:
Allergies:
Immunizations:
Attending Physician/Team:
PMH: COPD (emphysema)
Cognitive Skills Required prior to
Simulation: i.e. independent reading
History of Present illness:
(R), video review (V), computer
simulations (CS), lecture(L)
Review the pathophysiology of COPD
(emphysema). Consider etiology, symptoms,
“normal” lung sounds, “normal” ABGs.
Consider the following questions. Choose
your best answer. Provide rationale for your
choice, and rationale for not choosing other
answers.
1. The nurse is caring for a patient who was
admitted with an exacerbation of COPD. The
patient’s respirations are 28 with dyspnea on
exertion. The patient is receiving 2L of
oxygen per nasal cannula. The morning pulse
oximetry is 92%. Which nursing intervention
is of priority?
A. Monitor the patient
B. Notify the physician
C. Get an order to increase the oxygen
D. Place in semi-Fowler’s position
Social History:
Primary Diagnosis:
Surgeries/Procedures:
Submitted 2007 – Updated 2015
Page 1
Minnesota Simulation in Healthcare Education Professionals (M-SHEP)
2. A patient has a long history of COPD and
is currently experiencing an exacerbation of
his disease. The following lab work is done
this morning: CBC, ABGs and an electrolyte
panel consisting of K+, Na+, Cl-, BUN,
FBS. Which lab data requires immediate
follow up?
A. PaO2 WNL
B. increased RBCs
C. increased PaO2
D. Hgb WNL
3. A patient is admitted with an acute
exacerbation of COPD. Which assessment
finding is most indicative of a potential
complication?
A. R 32, increasingly anxious and restless
B. Using accessory muscles during
respiration
C. Pulse oximetry 92%, purse-lip breathing
D. Expectorating copious amount of white
phlegm.
Simulation Learning Objectives:
1.
2.
3.
4.
Prioritize the care for a patient with COPD (emphysema)
Apply assessment findings to the pathophysiology of COPD (emphysema)
Accurately calculate an IV drip rate
Administer medication via a secondary IV set-up
Fidelity
Setting/Environment
o Med-Surg
Medications and Fluids
o IV Fluids: D5 0.45% NaCl @ 75
ml/hr
Simulator Manikin/s Needed:
Vital Sim
Props:
Equipment attached to manikin:
o IV tubing with primary line
___________ fluids running at
__________ cc/hr
o Secondary IV line __ running at _
cc/hr
Submitted 2007 – Updated 2015
o Oral Meds:
Acetaminophen 650 mg q4h prn
Azmacort 2 puffs every 6 hours
Albuterol nebulizer 2.5 mg every 6
hours
o IVPB:
Ampicillin 500 mg every 4 hours
o IV Push:
Page 2
Minnesota Simulation in Healthcare Education Professionals (M-SHEP)
o
o
o
o
o
o
o
IV pump
Foley catheter ________cc output
PCA pump running
IVPB with ___ running at ___ cc/hr
02 _______
Monitor attached
ID band _______
Equipment available in room
o
o
o
o
o
o
o
o
o
o
o
o
o
Bedpan/Urinal
Foley kit
Straight Catheter Kit
Incentive Spirometer
Fluids
IV start kit
IV tubing
IVPB Tubing
IV Pump
Feeding Pump
Pressure Bag
02 delivery devices type
Crash cart with airway devices and
emergency medications
o Defibrillator/Pacer
o Suction
o Other_________
Roles / Guidelines for Roles
o
o
o
o
o
Primary Nurse
Secondary Nurse
Nursing Assistant
Family Member #1
Observer/s
o IM or SC:
Diagnostics Available
o
o
o
o
Documentation Forms
o
o
o
o
o
o
o
o
o
o
o
o
Physician Orders
Admit Orders
Flow sheet
Medication Administration Record
Kardex
Graphic Record
Shift Assessment
Triage Forms
Code Record
Anesthesia / PACU Record
Standing (Protocol) Orders
Transfer Orders
Other Props
Recommended Mode for simulation:
Student Information Needed Prior
to Scenario:
Important information related to
roles:
Wife (Family member): Sit very close to the
patient’s bedside. Hold patient’s hand. Keep
repeating – “He can’t breathe, do something,”
“Please help my husband,” etc. try to be a bit
of a pest. If the nurses do not at least elevate
the HOB be more dramatic and insistent in
your communication that your husband cannot
Submitted 2007 – Updated 2015
Labs
X-rays (Images)
12-Lead EKG
Other
Has been oriented to simulator
Understands guidelines /expectations
for scenario
Has accomplished all pre-simulation
requirements
All participants understand their
assigned roles
Has been given time frame
expectations
Report students will receive before
simulation:
Time:
Page 3
Minnesota Simulation in Healthcare Education Professionals (M-SHEP)
breathe. If it appears that the nurses are not
getting the message to raise the HOB – give
them a prompt, like “at home he sleeps on 2
pillows”
Critical Lab Values:
ABG – pH 7.30; PCO2 58; PO2 89; HCO3
30; O2 Sat 88% on RA
Physician Orders:
Admit to simulation unit with COPD
exacerbation and possible pneumonia.
BR with BRP with assistance
Soft, high protein diet
STAT CXR and ABG; Sputum for C&S – my
induce if necessary
O2 to keep O2 sats >90%. Start O2 after
ABGs drawn
CBC with diff; metabolic panel this AM
Acetaminophen 650 mg PO q4h PRN Not to
exceed 6 tabs/day
D5 0.45% NaCl @ 75 mL/hr
Ampicillin 500 mg IV q4h. Start after sputum
culture obtained.
Azmacort 2 puffs q6h
Atrovent 2 puffs q6h
Albuterol nebulizer 2.5mg q6h
You are assigned to care for Roger Elofson
who is a 68 year old male patient admitted at
0500 with an exacerbation of his COPD. It is
now 0700, and you are listening to change of
shift report.
Room 347-1, Roger Elofson, was admitted at
0500 this morning with emphysema. He has
had emphysema for the last 25 years. He uses
oxygen at home as needed. He uses an
albuterol nebulizer at home as needed, and
takes an Atrovent MDI every 6 hours. Mr.
Elofson had a bad night. He has been
confused and agitated. He is a lot more SOB
this AM. His lungs have decreased breath
sounds in all lung fields with a prolonged
expiratory phase. There is scattered wheezing
throughout with crackles in LLL.
0600 VS = 98.8, 102, 146/98. At 0700 O2 sat
87% on RA
Mr. Elofson has no admission orders. He did
bring a history and physical with him. He
was supposed to come to the hospital after
seeing his doctor yesterday afternoon, but he
waited because he hoped his breathing would
improve. He doesn’t know what his normal
O2 sat is. I was not able to do much of the
admission since he is so SOB. Sorry.
References, Evidence-Based Practice Guidelines, Protocols, or Algorithms
used for this scenario: (site source, author, year, and page)
http://www.webmd.com/lung/copd/tc/chronic-obstructive-pulmonary-disease-copdoverview
Submitted 2007 – Updated 2015
Page 4
Minnesota Simulation in Healthcare Education Professionals (M-SHEP)
Scenario Progression Outline
Timing
Manikin Actions
(approximate)
Nursing assistant
enters report room at
end of report saying
“You need to come
now – Mr. Elofson is
having trouble
breathing.”
Patient is stabilized.
Physician faxes orders
Manikin is flat in bed
VS: T 101.2oF P 128 R 40 BP
150/100 O2 Sat 88% on RA
Expected Interventions
May use the following
Cues:
Place HOB in semi-Fowler’s position
Yes: HR: 120; RR: 28; O2 sat: 85%;
Pt continues to feel SOB
No: RR: 40; O2 sat: 79%
Role member providing
cue:
Cue:
See Labs
Lung sounds wheezy throughout,
crackles in bases
O2 applied
Yes: HR: 110; RR: 22; O2 sat: 90%;
Pt’s respirations less labored; patient
states that breathing feels improved
No: wife continues to beg nurses that
something be done. Wife prompts that
patient uses O2 at home. Wheezing
becomes louder and respirations
become more labored.
Reassess VS and O2 sats
Auscultate lung sounds and perform a
respiratory assessment
Place patient on continuous pulse
oximetry
Call physician for orders
Initiate priority orders: ABGs and
sputum, CXR, inhaler, IV, labs,
antibiotic.
Calculate drip rate for 75 ml/hr
Submitted 2007 – Updated 2015
Role member providing
cue:
Cue:
Role member providing
cue:
Cue
Page 5
Minnesota Simulation in Healthcare Education Professionals (M-SHEP)
Scenario Progression Outline
Timing
Manikin Actions
Expected Interventions
(approximate)
May use the following
Cues:
.
Role member providing
cue:
Cue:
Submitted 2007 – Updated 2015
Page 6
Minnesota Simulation in Healthcare Education Professionals (M-SHEP)
Debriefing / Guided Reflection Questions for this Simulation
Link to Participant Outcomes and Professional Standards
(i.e. QSEN, NLN {Nursing}, National EMS Standards {EMS}, etc.)
1. What went well?
2. What could have gone better?
3. Nurse: How did you feel when faced with a patient that could not breathe, and a wife who
was very troubled with his condition?
4. Observers: Give feedback to the nurses as to what you saw as possible alternatives to the
assessments and interventions you observed.
5. Wife: How did it feel to have a loved one experiencing difficulty breathing?
6. Review discussion questions (Questions above)
a. The answer is A. The patient is manifesting signs and symptoms consistent with
COPD. Patients with COPD experience some degree of hypoxia. Options B and C
are not appropriate at this time. Option D is not the best position for a patient with
COPD
b. The answer is A. Hypoxemia provides the stimulus for the respiratory drive in
patients with COPD. Increased O2 levels may depress the respiratory drive.
Options B and C are expected findings. Option D does not require immediate
follow up
c. The answer is A. Increasing anxiousness and restlessness are signs indicating
hypoxemia. Options B, C, and D are expected findings for a patient with an
exacerbation of COPD.
7. What is the reason this patient is receiving an inhaler and nebulizer?
8. Discuss pharmacologic treatment of COPD
a. Beta agonist (bronchodilator) ex. Albuterol/Ventolin
b. Anticholonergic (bronchodilator) ex. Ipratropium/Atrovent
c. Inhaled corticosteroid used to reduce frequency of exacerbations in patients in
later stages of COPD. Ex. Triamcinolone/Azmacort; beclomethasone/Vanceril
d. Usually given in above order, then swish after inhalation
9. Are Mr. Elofson’s lung sounds abnormal for a patient with emphysema? (decreased LS
throughout with prolonged expiratory phase, scattered wheezing)
a. The decreased breath sounds and prolonged expiratory phase are not abnormal d/t
the pathophysiology of COPD – air trapping. Scattered wheezing may or may not
be abnormal – depends on the severity of the disease, and other symptoms
present.
10. What kind of information does the nurse need to know before calling a physician for
orders?
a. Current state of the patient – airway patency, VS, O2 sat, current LOC,
respiratory status, quality of respirations, lung sounds, allergies
i. What is the rationale for giving this patient a soft high protein diet?
1. Patients with COPD have decreased energy levels, and eating
consumes much of their available energy. COPD patients need
high quality calories such as protein so that they have enough
Submitted 2007 – Updated 2015
Page 7
Minnesota Simulation in Healthcare Education Professionals (M-SHEP)
nutrients to meet their needs, despite limited food intake. A soft
diet is easier to eat, again saving energy.
11. Which of 0730 VS are of concern? (101.2, 128, 40, 150/100)
a. HR, RR, BP. HR and BP are concerning because they are taxing cardiac reserves.
We don’t know this patient’s cardiac status, but these values are too high. RR is
concerning because of its high rate – again will compromise gas exchange. T may
be concerning if it is causing the patient difficulty
12. ABGs = pH 7.30; PCO2 58; PO2 89; HCO3 30. O2 sat 88% RA. What acid/base
imbalance is represented by these blood gases? Is this abnormal for this patient? Give
rationale. What is the relationship of the HCO3 to the rest of the blood gases?
a. The imbalance is respiratory acidosis. This is not unusual for a patient with
COPD, due to air trapping and disintegration of the alveoli which impedes gas
exchange. The HCO3 is slightly elevated because there is some attempt at
compensation. The O2 sat is difficult to evaluate, as there is not baseline data
available. However, a patient with COPD should never be denied necessary O2
based on blood gas values.
Complexity – Simple to Complex
Suggestions for changing the complexity of this scenario to adapt to different
levels of learners:
Submitted 2007 – Updated 2015
Page 8
Minnesota Simulation in Healthcare Education Professionals (M-SHEP)
SIMULATION SCENARIO
COPD – Respiratory Distress
Student Copy
LEARNING OBJECTIVES
1.
2.
3.
4.
Prioritize the care for a patient with COPD (emphysema)
Apply assessment findings to the pathophysiology of COPD (emphysema)
Accurately calculate an IV drip rate
Administer a medication via a secondary IV set-up
SUPPLIES NEEDED
Medical-Surgical text
Nursing drug reference
PATIENT DATA
You are assigned to care for Roger Elofson is a 68 year old male patient admitted at 0500 with
an exacerbation of his COPD. It is now 0700, and you are listening to change of shift report.
REFERENCES
http://www.webmd.com/lung/copd/tc/chronic-obstructive-pulmonary-disease-copd-overview
Submitted 2007 – Updated 2015
Page 9