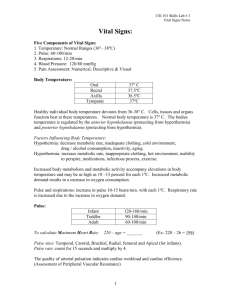
Interpreting Vital Signs
advertisement

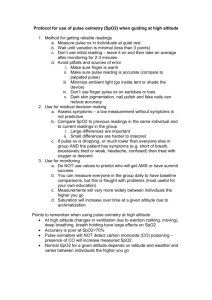
Interpreting Vital Signs Joseph J. Mistovich, MEd, NREMT-P William S. Krost, BSAS, EMT-P Daniel Limmer, AS, EMT-P © 2006 Assessing vital signs is a standard component of any patient assessment. The five vital signs to be obtained are respiration, pulse, skin, blood pressure and pupils. Baseline refers to the first set obtained on that patient. It is extremely important to cognitively process the baseline values, since trends in the patient's condition, such as improvement, stability or deterioration, are identified using this data. Some vital sign findings may present as abnormal and indicate a significant patient pathology, whereas, other findings that appear to be abnormal are indeed a normal response. Following is a discussion of some of these normal and abnormal findings that may assist you in more accurately interpreting vital sign data obtained from patients Respiration When assessing respiration, it is important to determine not only respiratory rate, but also tidal volume. Respiratory rate alone does not provide an indication of the adequacy of respiratory status. In order for a patient to be breathing adequately, he must have a respiratory rate that is adequate and an adequate tidal volume. Thus, it is two "adequates" (rate and tidal volume) that constitute adequate breathing. Only one "inadequate" establishes an inadequate ventilatory status and requires immediate intervention with positive pressure ventilation. Respiratory rate is determined by counting the number of respirations (one inhalation and one exhalation = one respiration) in one minute. On average, adult patients breathe between 12 and 20 times per minute. A respiratory rate outside of that average range may be considered abnormal. However, recognize that a patient can have a resting respiratory rate of less than 12 or greater than 20 and not be considered to have an abnormal respiratory rate. As an example, if a patient has a resting respiratory rate of 10 per minute and displays no evidence of respiratory distress or hypoxia; he is talking clearly and normally; and he is alert and oriented to person, place and time, a respiratory rate of 10/minute in this patient would clearly not be considered abnormal. On the other hand, elderly patients typically have higher resting respiratory rates due to decreases in tidal volumes. It would not necessarily be abnormal for an elderly patient to have a resting respiratory rate of 20-22/minute. Once again, consider the respiratory rate in conjunction with other physical findings to make a clinical judgment of normalcy. Tachypnea (faster than normal respiratory rate) usually indicates cellular hypoxia, acidosis or conditions that interfere with gas exchange, ventilation or perfusion, such as pulmonary edema, pneumonia and pulmonary embolism. As perfusion of cells with oxygenated blood begins to decrease, cells may be forced to convert from aerobic metabolism (metabolism of glucose with oxygen), where the byproduct of carbon dioxide and water is produced, to anaerobic metabolism (glucose metabolism without oxygen), where lactic acid is a primary byproduct. As the metabolic acid level increases within the body, the respiratory rate will increase in an attempt to reduce the acid load. Thus, you can expect tachypnea as an early sign in the shock patient with poor tissue perfusion. A patient who presents with tachypnea and exhibits no signs of distress, and has no evidence of any trauma that would explain the etiology of the tachypnea or any other overt clinical reason for the fast respiratory rate, would be described as having "quiet tachypnea." Quiet tachypnea is often a sign of metabolic acidosis. Tachypnea can be a normal response to pain. Thus, in a patient whom you suspect is experiencing peritonitis with severe abdominal pain, tachypnea may be a normal response associated with pain and anxiety and may not necessarily be an indication of a hypoxia state. In this situation, it would be prudent to obtain a pulse oximeter reading and look for any other clinical signs or symptoms of hypoxia. If none are found and the SpO2 is above 95% while the patient is breathing room air, you can suspect the tachypnea may be related to pain and anxiety and less to a hypoxic state. When obtaining pulse oximetry readings, it is important to document the reading based on the FiO2 (fraction of inspired oxygen) the patient is breathing. A patient breathing room air (21% oxygen) who has a SpO2 reading of 95% would not be of great concern; however, a patient who has been on a nonrebreather at 15 lpm for a period of time and has a SpO2 reading of 95% may be of great concern. You would have to suspect in the latter patient that when the nonrebreather mask is removed, the SpO2 reading will decrease well below 95%, reflecting poor blood oxygen content. Removing the nonrebreather mask in this patient would precipitate a hypoxic state. A patient who presents with a SpO2 reading near or at 100% while on room air but is severely hypoxic is the carbon monoxide-poisoned patient. The pulse oximeter works by reading the color of hemoglobin. When oxygen is bonded to hemoglobin it turns the hemoglobin molecule red. Thus, the pulse oximeter compares oxygenated hemoglobin (red color) to unoxygenated hemoglobin to determine oxygen saturation. The result is a SpO2 percentage reading. Carbon monoxide (CO) has a high affinity for hemoglobin. When CO binds with hemoglobin, it turns the hemoglobin molecule a bright red color. Thus, the pulse oximeter is reading the hemoglobin as being highly saturated with oxygen when it is really bonded with high amounts of CO. The SpO2 reading will be extremely high even though the CO is producing severe cellular hypoxia. In this situation, the pulse oximeter reading will not match the patient's signs and symptoms of hypoxia. Bradypnea (slower than normal respiratory rate) may be an indication of head injury, stroke or toxic syndromes involving central nervous system depressants. Bradypnea may also be an ominous sign of respiratory failure or impending respiratory arrest. Pulse Pulse rate is simply determined by measuring the number of beats in one minute. This is typically translated into a heart rate; however, be cautious when making the assumption that the pulse always directly correlates with the heart rate. In some conditions, the heart contraction is not strong enough to produce a palpable pulse with each beat. A good example of this may be the patient who is experiencing a supraventricular tachycardia (SVT). Due to the excessively high heart rate, the ventricular diastolic filling time is drastically shortened, leading to a reduction in preload, stroke volume and cardiac output. This may result in contractions that are not producing palpable pulses. Thus, the EMS provider may document a heart rate based on the palpation of a peripheral pulse that is less than the actual heart rate. If possible, attach the patient to a continuous ECG monitor and compare the palpable pulse rate to the heart rate on the oscilloscope. If you are unable to apply a continuous ECG monitor, auscultate the apical pulse with a stethoscope and compare it to the peripheral pulse to determine if there is a discrepancy in the heart contraction and pulse wave production. Bradycardia is a lower than normal heart rate. Bradycardia may be due to medical or trauma conditions such as a cardiac conduction defect, central nervous system depressant drug use or overdose, Cushing's reflex in a head-injured patient, poisoning, or an ominous sign of severe hypoxia and impending respiratory and cardiac arrest. There are many other causes of bradycardia. Once again, it is important to consider the bradycardia in relation to the whole patient. Extremely fit athletes and individuals may have very low resting heart rates. They will not exhibit any evidence of hypoperfusion or hemodynamic instability as a result of the low resting heart rate, as will sick individuals with abnormally low heart rates. Assess the mental status, skin perfusion, work of breathing and blood pressure to gauge the patient's stability. Be aware that patients on beta blockers and calcium channel blockers may not respond with tachycardia when expected due to the blockade of the beta receptor sites and calcium ion movement, respectively. An example is a patient who takes atenolol (a beta blocker) who is involved in a traumatic incident and is hemorrhaging. The patient's skin is pale, cool and clammy; he is anxious and tachypneic; however, his heart rate remains less than 90 beats per minute. The heart rate does not match the typical shock presentation. Upon learning that the patient is taking a beta blocker, it is evident that a high heart rate is not to be expected in this case and should not be used as an effective gauge of the class of hemorrhage due to the beta receptor site blockade. It is important to note that elderly patients may present with an elevated resting heart rate that is 90 beats per minute. If you encounter a young or healthy individual who has experienced blunt trauma to the chest and has a sustained tachycardia even after you have him past the acute stress reaction phase, suspect a possible myocardial contusion. This is also true of a young or healthy individual with blunt trauma to the chest who presents with an irregular pulse. Like tachypnea, tachycardia may be associated with the body's response to pain. The quality of the pulse may provide some information about cardiac output. A strong peripheral pulse usually indicates good left ventricular filling and contractility. A weak and thready pulse is usually an indication of an increased systemic vascular resistance, poor left ventricular filling, or an ineffective left ventricular contractile force. Thus, pulse quality can provide an indication of the effectiveness of cardiac contraction and blood volume. Pulsus alternans, also known as mechanical alternans or pressure alternans, is identified by a variation in pulse strength from contraction to contraction. The amplitude (strength) of the pulse varies from beat to beat, even though the rhythm remains regular. One pulse wave may be strong and the next may be weak, followed again by a strong pulse. The pulse amplitude basically alternates between strong and weak. This is usually an indication of severe left ventricular dysfunction and is important to report to the receiving facility. If you notice a change in amplitude while taking a pulse, continue to assess the pulse while watching the respirations. If you notice a decrease in the pulse amplitude (it weakens or becomes absent) during inspiration, it may be an indication of pulsus paradoxus. This may be a subtle finding that is hard to detect in the field; however, it is a significant finding that may indicate severe increases in intrathoracic pressure (severe acute asthma attack and obstructive lung disease), or other conditions such as pericardial tamponade, adhesive pericarditis, advanced congestive heart failure and hypovolemia. EMS personnel are frequently taught that pulse location (radial, brachial, femoral or carotid) correlates with the estimated systolic blood pressure. It is postulated that a systolic blood pressure of 80-90 mmHg is needed to produce radial pulses, a systolic blood pressure of 70 mmHg is needed to produce femoral and brachial pulses, and a systolic blood pressure of 60 mmHg is needed to produce carotid pulses. Be careful when interpreting this finding. One article found that trauma patients with a radial pulse had a mean systolic blood pressure (SBP) of 72.5 mmHg; 83% of the trauma patients with a radial pulse had a SBP of less than 80 mmHg. Trauma patients with a femoral and carotid pulse had a mean SBP of 66.4 mmHg; 83% of the trauma patients with a femoral or carotid pulse had a SBP less than 70 mmHg. It is necessary to have a SBP of 60 mmHg to produce a carotid pulse. Skin Assess the patient's skin color, temperature and condition. Abnormal skin color may include pallor, cyanosis, flushing or redness, mottling or jaundice. Cyanosis is a late sign of hypoxia or poor perfusion states. Redness or flushing is typically a result of peripheral vasodilation. Pallor is an early sign of hypoxia and is also seen in poor perfusion states. Mottling occurs when blood stagnates in an area of poor perfusion and becomes deoxygenated. Jaundice, a yellow coloring of the skin and sclera, is a sign of hepatic failure. Abnormal skin temperatures may be cool, cold or hot. When assessing the skin, be sure to take into account the ambient temperature. Hot skin temperature may be an indication of a significantly increased body core temperature. Peripheral vasoconstriction will cause the warm red blood in the skin to be shunted to the core of the body, resulting in cool skin temperature. Cold skin usually occurs as a result of a significant decrease in the body's core temperature. The moisture and dryness of the skin refers to condition. Skin is normally dry to touch. Moist skin may be a result of discharge of the sympathetic nervous system and from the alpha properties' stimulation of the sweat glands from circulating epinephrine and norepinephrine. Both hormones will also cause vasoconstriction, leading to cool, pale, clammy skin. Extremely dry skin may occur as a result of dehydration. Skin turgor is tested to determine the presence of dehydration. Turgor is actually the speed at which the pinched or lifted fold of skin returns to its normal place. A decrease in turgor is an indication of dehydration. One of the best places to assess for skin turgor is on the chest over the sternum. Elderly patients undergo changes in the structure of the skin that make it less elastic. With the loss of recoil, the skin will stay tented when pinched. Thus, skin turgor is not a good test to assess the dehydration status of elderly patients. Suspect dehydration if the oral mucosa is dry, the tongue is furrowed and there is a lack of tear formation. Capillary refill is a useful test of hydration status in pediatric patients. The best place to test for capillary refill in children is on the forearm or over the patella (kneecap). Blood Pressure Auscultation of blood pressure can potentially provide more information than palpation. An auscultated blood pressure provides both a systolic and diastolic value. Both are reported in even numbers in increments of 2 mmHg. The normal range for a systolic blood pressure is 100 to 140 mmHg and 60 to 90 mmHg for diastolic. Systolic blood pressure is a measure of left ventricular function. It is important to note that a diastolic blood pressure represents more than just the relaxed phase of the cardiac cycle. Diastole is a direct measure of the degree of vessel constriction or vascular resistance. If a patient is compensating for either an abnormally high or abnormally low blood pressure, they may vasoconstrict or vasodilate, respectively, and the diastolic blood pressure value will reflect the change. This may provide an indication of how well a patient is compensating for changes in cardiac output. A pulse pressure is determined by subtracting diastolic blood pressure from systolic blood pressure. A normal pulse pressure is often noted as 30 to 40 mmHg. More specifically, a narrow pulse pressure is one that is less than 25% of the systolic blood pressure. A narrow pulse pressure may be an indication of a decreasing cardiac output and an increasing peripheral vascular resistance associated with systemic vasoconstriction. A wide pulse pressure is greater than 50% of the systolic blood pressure. A wide pulse pressure may be seen in brain-injured patients exhibiting Cushing's reflex where the systolic blood pressure drastically increases to maintain cerebral perfusion, but the diastolic remains normal or low. If fluid or blood loss is suspected in the medical patient, you may perform the "tilt test" or test for orthostatic vital signs. You are actually testing for postural hypotension. To do so, place the patient in a supine position for approximately two minutes or more. Assess the blood pressure and heart rate. Move the patient into a standing position. This allows for 7 to 8 ml/kg of blood to be transferred to the lower extremities due to gravity. After two minutes, reassess the blood pressure and heart rate with the patient in the standing position. A patient with a volume deficit will experience a decrease in preload, stroke volume and cardiac output. Clinically, this will present as a decrease in systolic blood pressure and an increase in heart rate. If the systolic blood pressure decreases greater than 20 mmHg or the heart rate increases by greater than 20 to 30 beats per minute from the supine to standing vital signs, the patient is said to have orthostatic vital signs or postural hypotension. The increase in heart rate has been found to be a more sensitive indicator of volume depletion. Be cautious when interpreting a decrease in systolic blood pressure when performing the orthostatic tilt test, especially on elderly patients. Approximately 10% of persons younger than age 65 and 11%30% older than 65 who have a normal blood volume will exhibit a decrease in systolic blood pressure of 20 mmHg or greater when moved from a supine to standing position. Thus, an increased heart rate of greater than 20 beats per minute becomes a better predictive indicator of volume depletion when performing this test. If a sudden drop of greater than 10 mmHg in the systolic reading is found when assessing blood pressure, note the phase of respiration when the drop is occurring. If a drop of greater than 10 mmHg of pressure is noted during the inspiratory phase of respiration, it may be an indication of pulsus paradoxus, which can be seen in cardiac tamponade, pericardial effusion, constrictive pericarditis, pulmonary embolism, cardiogenic shock, bronchial asthma or tension pneumothorax. Another indication of pulsus paradoxus seen on physical examination is engorgement of the jugular veins on inspiration. This is known as Kussmaul's sign. When assessing a patient complaining of chest pain or midscapular pain, measure the blood pressure in both upper arms and compare the systolic readings. If there is a difference of 10 to 20 mmHg in the systolic blood pressure between both extremities, it may be an indication of an aortic dissection. ACE inhibitors are drugs that cause blood vessels to dilate, thereby reducing the vascular resistance, which results in a decrease in blood pressure. This lower vascular resistance reduces the myocardial workload and can improve the function of a weakened heart. In the patient who presents with a low blood pressure, consider the possibility of ACE inhibitor use. Pupils Assess the pupils for size, equality and reactivity. Pupil signs may provide some evidence as to the integrity of the brainstem. Pupils may also provide a clue as to whether the coma patient has a structural lesion or if the condition is of a metabolic etiology. Pupils that are unequal, fixed and dilated in a comatose patient indicate a structural etiology or space-occupying lesion. If the coma or altered mental status is due to a metabolic cause such as hypoxia, drug overdose or hypoglycemia, the pupils will remain equal and reactive to light; however, they may respond more sluggishly. When encountering a patient with an unknown etiology of coma, pupil signs may provide a clue as to the cause. Conclusion Abnormal findings in the vital signs may provide clear indications of certain conditions. It is important to understand what is considered to be truly normal and abnormal. It is evident that some abnormal findings in one patient age group may be normal in another. Anytime an abnormal vital sign is identified, process it cognitively and consider it in relation to the whole patient assessment.