High Altitude Medicine
advertisement

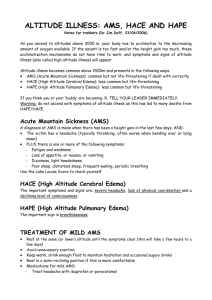
High Altitude Medicine Definition Pathophysiology High altitude: >1500m (4900ft) Mod high altitude: 2000 – 3500m (6600-11500ft) Very high altitude: 3500-5500m (11500-18000ft) Extreme altitude: >5500m Sea level: ppO2 760, piO2 150 1000m: ppO2 670, piO2 140 2000m: ppO2 600, piO2 120 5500m: ppO2 380, piO2 70 8848m (Mt Everest): ppO2 240, piO2 40 Acute mountain sickness (AMS): occurs at >2500m; usually self limited High altitude cerebral oedema (HACE(: a continuum of AMS; progression of neurological symptoms in setting of AMS; can be fatal High altitude pulmonary oedema (HAPE): a continuum of AMS; can be fatal (cause of most deaths); begins >3500m Chronic mountain sickness (CMS): after prolonged exposure; headaches, insomnia, lethargy, Hct >60%, Hb >20 Others: snow blindness, retinal haemorrhage, thromboembolism, retinopathy, immunosuppression, hypothermia, epistaxis Acclimitisation: physiological adaptation to hypoxia which improves systemic O2 delivery; risk AMS/HACE; most people can acclimitise up to 5500m, but differing capability between individuals Respiratory (primary response): periodic breathing >3000m (max at 1/52), tachypnoea respiratory alkalosis HCO3 diuresis continued RR (acetazolamide helps with this); lung volume, pulmonary capillary blood volume ( diffusing capacity); pulmonary HTN; Typical ABG at 8848m = pO2 28, pCO2 7 CV: max HR, pulmonary artery pressure, SV, BP, central blood volume due to peripheral vasoconstriction ( diuresis plasma volume, hyperosmolality, haemoconcentration); CO Haematological: RBC (over days – wks; has no effect on initial climitisation), erythropoietin (within 2hrs) Other: vascularity of tissues, tissues ability to use O2, cerebral blood flow, 2,3,DPG shift curve to R (but respiratory alkalosis shifts curve to L) High altitude illness: Hypoxia occurs with rapid ascent; exercise tolerance 9% for each 1000m; relative hypoventilation, impaired gas exchange, fluid retention and redistribution, sympathetic drive AMS: cytotoxic and vasogenic cerebral oedema, neurotransmitter dysfunction cerebral oedema and ICP HACE HAPE: due to exaggerated pressor response to altitude and hypoxia non-cardiogenic pulmonary oedema (hydrostatic; possible due to impaired Na-driven clearance of alveolar fluid), high pulmonary artery pressure Epidemiology High altitude illness: occurs in 25% sea level dwellers to ascent rapidly to >2400m AMS: 30% incidence at >3500m; 50-60% incidence at >4000m HACE: occurs in 1-2% AMS at >4500m; fatal in 1-2/7 if not treated HAPE: preceded by AMS in 50%, by HACE in 14%; 15% at 4000m, 0.1% at 2500-3000m Risk Factors AMS: PMH same, individual susceptibility, obesity, CV/RS disease. NOT related to age / physical fitness rate of ascent (especially >300m/day), altitude, time at altitude, degree of physical exertion, previous recent exposure, sleeping altitude HAPE: as above; also cold temp, pre-existing respiratory infection Assessment AMS: onset within 24 hours of arrival at altitude (usually 1-6 hours); headache, fatigue out of proportion, insomnia, anorexia, N+V, SOB, oliguira; no physical findings (except maybe evidence of fluid retention) HACE: progresses over 1-3/7; consider if >3000m and altered LOC, impaired mental capacity ( visual acuity / attention span / short term memory / decision making), marked truncal ataxia, 3rd + 6th nerve palsy; can progress to coma within 24 hours of onset of ataxia HAPE: consider alternate diagnosis; onset 2-4/7 after arrival at altitude; non-productive cough ( pink, frothy sputum), SOB; tachycardia, tachypnoea, cyanosis, crepitations (RML 1st, exercise induced), patchy opacities on CXR (often more in RML); ECG (RVH, RAD, RBBB); severe hypoxia HACE, coma, death Do not go higher in presence of symptoms; avoid ETOH and sedatives; carbohydrates may help arterial oxygenation ( resp quotient, alveolar pO2; risk of AMS by 30%); rest Mild/mod AMS: halt ascent; rest; O2 and consider drugs as below; hydration, analgesia; usually settles over 2-3/7 as acclimitisation occurs; or consider descent by up to 300m/day with rest day every 2-3/7 Management Prevention Prognosis Severe / HACE / HAPE: O2: (1-2L/min until symptoms resolve; aim SaO2 >90%; in HAPE, if SOB improves with this, can observe at altitude until recovery) Descent (immediately if change in LOC / ataxia / pulmonary oedema; otherwise descend if O2 not helping; by >300m in AMS, by >500-1000m / evacuate in HAPE, ASAP >1000m / until improvement / evacuate in HACE) Hyperbaric Oxygen: if unable to descend / temporising measure; Gamow bag simulates 600m descent, requires scavenger etc… Dexamethasone: in AMS / HACE; 8mg STAT 4mg Q6h PO/IM/IV ASAP; onset 4hrs, max effect 12-24hrs; ?duration of treatment; as effective as acetazolamide Acetazolamide: consider if not already used as prophylaxis in AMS / HACE; 250mg BD PO; symptoms within 24hrs in 75%; stop once symptoms resolve (or continue if plan to re-ascend); contra-indicated in sulphur drug allergy; use as prophylaxis for HAPE, but not treat; cause HCO3 diuresis so allow more hyperventilation Nifedipine: in HAPE; 10mg SL STAT 20-30mg SR BD/TDS; drug of choice if O2 / descent not available; pulmonary artery pressure; used as prophylaxis and treatment of HAPE Symptomatic treatment: analgesia, antiemetics, beta-agonists; CPAP in HAPE Diuretics (eg. Frusemide, mannitol): only if generalised oedema present; avoid loop diuretics in HAPE as most are dehydrated Avoid flying directly to high altitude; limit activity for 24 hours after arrival; graded, slow ascent; when >3000m, ascent <300m/day; rest day every 1000m / every 2-3/7; avoid ETOH; eat carbohydrates; avoid over-exertion; avoid night sedation Acetazolamide: drug of choice; CA inhibitor (causes HCO3 diuresis and metabolic acidosis, CSF formation, ventilatory drive, maintains O2 during sleep; 125-250mg BD, commence at least 1/7 prior to ascent, continue until descent begun Dexamethasone: not as effective as acetazolamide; 4mg PO BD, but more side effects; use if acetazolamide contra-indicated or if rapid effect needed (eg. Rescue workers) Nifedipine: for prevention HAPE; 20mg SR BD/TDS Salmeterol: for prevention HAPE AMS: Most respond rapidly to treatment, with complete recovery HACE: recovery may be prolonged HAPE: most recover in 2-3/7