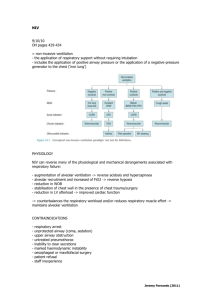
Advanced Ventilation Management: BiPAP, CPAP, AC, and
advertisement

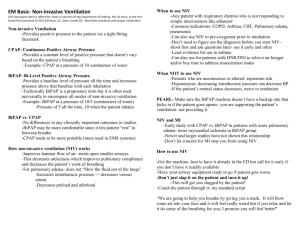
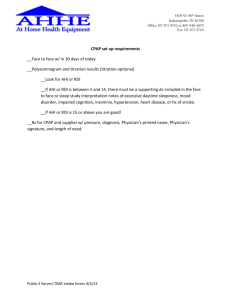
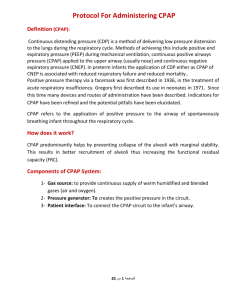
Procedural Skills for Medical Students Advanced Ventilation management: Bi-Level Positive Airway Pressure (BiPAP), Continuous Positive Airway Pressure (CPAP), Assist Control (AC), and Synchronized Intermittent Mandatory Ventilation (SIMV) Objectives: 1. Learners should be able to verbalize the physiologic differences in delivery of respiratory support between BiPAP and CPAP. 2. Learners should be able to verbalize the difference between AC and SIMV. 3. Learners will understand the basic settings of mechanical ventilation in AC and SIMV mode and normal ranges of these settings in adults. Material to review prior to lab: review CPAP versus BiPAP and Ventilator Management BiPAP: Indications 1. Exacerbations of COPD associated with hypercapnia. 2. Cardiogenic pulmonary edema associated with hypercapnia and/or unresponsive to CPAP alone. 3. Respiratory distress and pulmonary infiltrates in immunosuppressed patients. 4. Acute or chronic hypercapnic respiratory failure due to chest wall deformity or neuromuscular disease. 5. Decompensated obstructive sleep apnea with hypercapnia. Contraindications 1. A reduced level of consciousness, which results in an unprotected airway (GCS < 10) 2. Neurotrauma associated with raised intracranial pressure or fractured base of skull 3. Recent upper gastrointestinal surgery 4. Burns or trauma affecting the face 5. Bowel obstruction and/or vomiting 6. Severe confusion/agitation 7. Patient failure to clear respiratory secretions CPAP: Indications 1. To improve ventilation and oxygenation 2. To avoid intubation 3. Patients with congestive heart failure (CHF) with acute pulmonary edema 4. In near drowning patients 5. Severe respiratory distress 1 Procedural Skills for Medical Students Contraindications 1. Respiratory or cardiac arrest 2. Agonal respirations 3. Severely depressed level of consciousness 4. Pneumothorax 5. Inability to maintain airway patency 6. Major trauma, especially head injury with increased ICP or significant chest trauma 7. Facial anomalies or trauma (e.g., burns, fractures) 8. Vomiting 9. History of COPD 10. History of Pulmonary Fibrosis 11. Decreased LOC 12. Claustrophobia or unable to tolerate mask Mechanical Ventilation: Indications 1. Inability to protect one’s airway 2. Hypoxic respiratory failure 3. Hypercapnic respiratory failure 4. Cardiac arrest Contraindications 1. Advanced directives specifying no intubation or resuscitation Equipment: HPS, mechanical ventilator, BiPAP equipment, CPAP equipment Instructional Procedure & Endpoints: BiPAP 1. Learners will be oriented to HPS and equipment in ASTEC. 2. ASTEC staff will discuss the physiology of BiPAP, demonstrate placement and settings for BiPAP. 3. Learners will verbalize one indication for BiPAP. CPAP 1. Learners will be oriented to HPS and equipment in ASTEC. 2. ASTEC staff will discuss the physiology of CPAP, demonstrate placement and settings for CPAP. 3. Learners will verbalize one indication for CPAP. Assist Control 1. Learners will be oriented to trainer and equipment in ASTEC. 2. ASTEC staff will discuss the settings and physiology of assist control mechanical ventilation. 3. Learners will verbalize correctly 3 out of 5 initial vent settings of AC. 2 Procedural Skills for Medical Students SIMV 1. Learners will be oriented to trainer and equipment in ASTEC. 2. ASTEC staff will discuss the settings and physiology of synchronized intermittent mandatory ventilation. 3. Learners will verbalize correctly 3 out of 5 initial vent settings of SIMV. References: Amitai, A. (2011). Methods of ventilator support. Medscape. Retrieved from http://emedicine.medscape.com/article/810126-overview#aw2aab6b4 Esherick, J. (2011). Mechanical ventilation. In J.L. Pfenninger, & G.C. Fowler (Eds.), Procedures for Primary Care, 3rd Ed (1415-1420). Philadelphia: Elsevier Mosby. Martin, L. (2011). Non-invasive positive pressure therapy: CPAP, BiPAP, ASV. What are they, and when do you use them? Retrieved from http://www.lakesidepress.com/CPAP/CPAP.htm#table 3