Toxicity Effects Following Ethanol and

Rachael DeVaux
Toxicity Effects Following Ethanol and Acetaminophen Ingestion
The relationship between alcohol and medication when paired together have become of very high interest in the health world as of late. Alcohol provides about 5 percent of daily energy intake in moderate drinkers, and significantly more in chronic alcohol abusers. It is important to be aware of the effects alcohol and medication, acetaminophen in particular, have on the body. Acetaminophen is an over the counter medication and commonly used to relieve pain and fevers. Overdosing from this medication alone is certainly possible, but with addition of alcohol, further consequences may arise to produce hepatotoxicity, given appropriate risk factors.
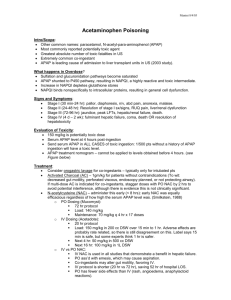
As stated above, negative effects are presented when alcohol and acetaminophen are combined, leading to severe hepatic injury. After taking therapeutic doses of acetaminophen without involvement of alcohol, generally no major health concerns ensue. However, in chronic alcohol abusers, an enzyme called cytochrome
P450 2E1 (CYP2E1) metabolizes a small segment of the additional acetaminophen to Nacetyl-p-benzoquinoneimine (NAPQI), a highly reactive substance in the metabolic process that is harmful to hepatic cells. Under normal conditions, this product is produced in small amounts, but when excessive alcohol is consumed, it is increased two or three fold (Dart et al., 2010). This is an issue because the increased NAPQI levels result in decreasing glutathione (GSH) concentrations. Glutathione, a natural antidote that detoxifies the liver, is usually seen in chronic alcohol abusers to be very low or even deficient. It has also been said that chronic alcoholism could increase acetaminophen toxicity either by short-lived induction of the CYP2E1 pathway or by decreasing the hepatic content of GSH (Schiødt, Lee et al, 2002).
A study by Thummel in 2000, took five men and five women volunteers to have completed a 6-hour intravenous infusion of either ethanol to reach a blood ethanol concentration of 100 mg/dL or infused 5% dextrose in water to test the levels of NAPQI
Rachael DeVaux following the procedure. Levels of NAPQI were measured immediately after ethanol was absent from the body. Simulation of consuming a standard 750mL bottle of wine, six 12ounce cans of beer, or 9 ounces of 80-proof liquor over a period of 6 hours was done, followed by ingesting 500mg of acetaminophen 8 hours after the end of infusion. The average NAPQI production was enhanced by 22% when given after an ethanol infusion, compared with after 5% dextrose in water infusion (Thummel, et al., 2000). This led to higher portions of the dose converting to NAPQI, and therefore lowering GSH levels to enhance liver toxicity. This study concluded that specific amounts of alcohol (750mL bottle of wine, six 12-ounce cans of beer, or 9 ounces of 80-proof liquor) added to the body, revealed a significant increase in risk for acetaminophen overdose.
The interaction between alcohol and acetaminophen are particularly complex. A study presented by Schmidt concluded that the time from overdose to treatment, chronic alcohol abuse, quantity of acetaminophen, and age are independent risk factors in the development of severe hepatotoxicity in patients with acetaminophen poisoning
(Schmidt, et al., 2002). It is speculated that abstaining from alcohol prior to acetaminophen use will reduce risk of liver failure. Timing of acetaminophen ingestion may be the most important prognostic factor when dealing with this issue. For alcohol abusers, the instance when NAPQI levels are highest and GSH lowest, indicate the period of highest risk for hepatic injury. Since humans demonstrate that alcohol ingestion induces CYP2E1 up to threefold, an effect lasting only several days after alcohol exposure has subsided, the period of highest risk for alcohol abusers is expected immediately after discontinuation of alcohol intake for newly abstinent abusers (Dart et al., 2010). Timing of alcohol consumption and acetaminophen ingestion is extremely variable from person to person, as demonstrated in the studies above. It is not only dependent on timing, but also depends on the amount of alcohol and acetaminophen consumed. It is distinguished in the study that risk of acetaminophen toxicity is highest
Rachael DeVaux when an alcohol abuser has left a significant amount of time between alcohol consumption and ingestion of pain medication, perhaps during a withdrawal period.
Knowing that about 60% of US adults consume alcohol occasionally, it raises concern about taking pain medication and alcohol collectively (Jalbert et al., 2008).
Acetaminophen, like many other medications available, may result in life-threatening outcomes when taken with alcohol. A review on the Concurrent Alcohol and Alcohol-
Interactive Prescription Drug Use in the US Population describes that physicians should screen for alcohol use prior and encourage patients to abstain from alcohol while taking the medication (Jalbert et al., 2008). It is essential that both pharmacists and physicians warn patients about the dangers of alcohol and medication use prior, to prevent alcoholdrug interaction. Currently, no alternative pain medications are safely recommended for heavy alcohol drinkers.
To conclude, alcohol is an important non-essential nutrient that is very common across people’s diets, providing substantial energy for moderate drinkers and increasingly more so in heavy drinkers. Though alcohol itself may cause effects in the body, it may furthermore enhance effects of acetaminophen to the point of hepatotoxicity when ingested together. A negative interaction between the two causes CYP2E1 to metabolize part of acetaminophen into NAPQI, a damaging metabolite to hepatic cells.
High levels of NAPQI concentration along with low levels of GSH lead to increased risk of hepatic injury, especially after alcohol intake has been discontinued. Another significant determinant of hepatotoxicity results from the amount and timing of alcohol consumed. Since risk visibly elevated with the addition of alcohol, it is strongly recommended not to intermix alcohol with acetaminophen. People should refrain from using alcohol while taking any type of medications, unless consulted with a physician, to eliminate any risks associated with overdose.
Rachael DeVaux
References
Dart, R. C., Green, J. L., Kuffner, E. K., Heard, K., Sproule, B., & Brands, B. (2010). The effects of paracetamol (acetaminophen) on hepatic tests in patients who chronically abuse alcohol - a randomized study. Alimentary Pharmacology &
Therapeutics , 32 (3), 478 –486. doi:10.1111/j.1365-2036.2010.04364.x http://proxy.library.oregonstate.edu/login?url=http://search.ebscohost.com/login.aspx?dir
ect=true&db=cmedm&AN=20491750&site=ehost-live
Schiødt, F. V., Lee, W. M., Bondesen, S., Ott, P., & Christensen, E. (2002). Influence of acute and chronic alcohol intake on the clinical course and outcome in acetaminophen overdose. Alimentary Pharmacology & Therapeutics , 16 (4), 707 –
715. http://proxy.library.oregonstate.edu/login?url=http://search.ebscohost.com/login.aspx?dir
ect=true&db=cmedm&AN=11929388&site=ehost-live
Thummel, K. E., Slattery, J. T., Ro, H., Chien, J. Y., Nelson, S. D., Lown, K. E., &
Watkins, P. B. (2000). Ethanol and production of the hepatotoxic metabolite of acetaminophen in healthy adults*. Clinical Pharmacology & Therapeutics , 67 (6),
591 –599. doi:10.1067/mcp.2000.106574 http://www.nature.com.ezproxy.proxy.library.oregonstate.edu/clpt/journal/v67/n6/full/clpt
200062a.html
Schmidt, L. E., Dalhoff, K., & Poulsen, H. E. (2002). Acute versus chronic alcohol consumption in acetaminophen-induced hepatotoxicity. Hepatology , 35 (4), 876 –
882. doi:10.1053/jhep.2002.32148 http://onlinelibrary.wiley.com.ezproxy.proxy.library.oregonstate.edu/doi/10.1053/jhep.200
2.32148/abstract
Jessica J. Jalbert, Brian J. Quilliam, & Kate L. Lapane. (2008). A Profile of Concurrent
Alcohol and Alcohol-Interactive Prescription Drug Use in the US Population.
Journal of General Internal Medicine , 23 (9), 6. doi:10.1007/s11606-008-0639-4 http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2518026/