CoSTaR Amiodarone vs Lidocaine Dec 15 2014
advertisement
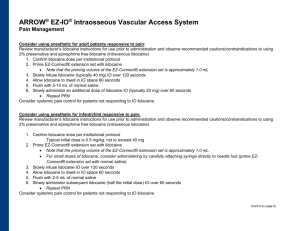
PICO Question : For infants and children with shock-refractory ventricular fibrillation (VF) or pulseless ventricular tachycardia (pVT) (P), does amiodarone (I), when compared to lidocaine (C), improve survival at hospital discharge, return of spontaneous circulation (ROSC), termination of arrhythmia, recurrence of VF or risk of complications (O). Introduction We identified 3 relevant articles in the literature addressing the above issue. One was in pediatrics and was an observational retrospective cohort study with patients in VF or pVT who received lidocaine, amiodarone or both. The relevant outcomes studied in this paper were ROSC and survival to hospital discharge. The other two were RCTs in adults. One was incessant, but pulsatile, VT and the other was ventricular fibrillation in adults. The outcomes studied in these papers were termination of arrhythmia, and survival to discharge, respectively. Quality of Evidence We found no randomized studies in pediatrics and two randomized studies in adults in comparison of amiodarone and lidocaine in the setting of pulseless VT or VF. For the critical outcome of survival to discharge, we found one randomized controlled trial in adults and one observational cohort study in pediatrics, both of very low quality. The observational study with no control group and a sample size less than 400, showed 21.6% (37/171) survival to discharge in amiodarone group and 25.8% (76/295) in the lidocaine group. The randomized controlled trial was in adult population and had a sample size less than 400. Survival to discharge was seen in 22.8% (41/180) in the amiodarone group and 12.0% (20/167) in the lidocaine group. For the important outcome of ROSC, the pediatric observational study demonstrated 50.9% (87/171) ROSC in the amiodarone group and 62.4%(184/295) in the lidocaine group. (OR 2.02, 1.36-3.03). This observational study was of very low quality, as there was no control group and a small sample size. For the important outcome of termination of arrhythmia, one randomized controlled study in adults of very low quality studied this outcome. The study was in adults, had a small sample size and had low patient enrollment. They showed 48.3% (14/29) termination on arrhythmia in the amiodarone group and 10.3% (3/29) in the lidocaine group. Gap analysis The major limitation in this analysis is the lack of RCTs of good quality in pediatrics, comparing amiodarone and lidocaine directly in the setting of pVT or VF. All of the representative data from the papers included is of low quality. The pediatric study is an observational study that found lidocaine to be superior to amiodarone. However, in the very low quality RCTs, although in adults, amiodarone was found to be superior to lidocaine. Given the very low quality of the data available, and the discrepancy of potentially superior agent between studies, no recommendation can be made between these drugs. Treatment Recommendations The confidence in effect estimates is so low that the panel feels a recommendation to change current practice is too speculative. We suggest that either amiodarone or lidocaine can be used in the setting of pVT/VF in infants and children. References 1. Valdes, SO, Donoghue, AJ, Hoyme, DB, Hammond, R, Berg, MD, Berg, RA, and Samson, RA. Outcomes associated with amiodarone and lidocaine in the treatment of in-hospital pediatric cardiac arrest with pulseless ventricular tachycardia or ventricular fibrillation. Resuscitation 2014;85:381-386. 2. Somberg, JC, Bailin, SJ, Haffajee, CI, Paladino, WP, Kerin, NZ, Bridges, D, Timar, S, Molar, J, and the Amio-Aqueous Investigators. Intravenous lidocaine versus intravenous amiodarone in a new aqueous formulation for incessant ventricular tachycardia. Am J Cardiol 2002; 90:853-859. 3. Dorian, P, Cass, D, Schwartz, B, Cooper, R, Gelaznikas, R, and Barr, A. Amiodarone as compared with lidocaine for shock-resistant ventricular fibrillation. NEJM 2002; 346(12): 884-890.