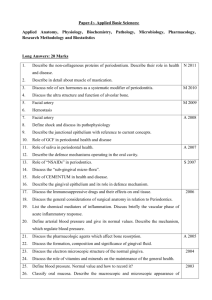
jcpe12371-sup-0004-AppendixS4
advertisement

Appendix 4. Radiographical, microbiological, or laboratory outcomes and authors' conclusion in human trials on HY as monotherapy or as adjunct to non-surgical and surgical periodontal treatment. Study (year) Radiographical, microbiological, and/or laboratory outcomes Non-surgical treatment Bevilacqua Significant reductions of calprotectin and myeloperoxidase in GCF were found after one week and an (2012) increase at 45 days in both groups. GCF volume decreased significantly. No inter-group differences were detected. Chauhan At 1- and 3-month intervals, a significant improvement in TLC and DLC counts was observed among (2013) the experimental groups as compared to control group. Eick (2013) Six months after SRP, the counts of T.d. were significantly reduced in both groups, as were those of C.r. in the test group only. P.i. and P.g. increased in the control group. Engström A bone loss (measured on radiographs) of 0.25 and 0.75 mm in the test and control group after 12 (2001) months was recorded (N.S.). Immune responses evaluated by IgG, C3, PgE2 content in GCF showed no differences during the 12 months and in all groups, the microflora (Prevotella spp., P.g., or A.a) showed a stable microecology. Gontiya (2012) None of the control or experiment sites showed absent or intense inflammatory infiltrate. About 33.3 and 71.4% of control and test sites showed slight inflammatory infiltrate, the remaining sites showed moderate infiltrate (N.S.). Johannsen (2009) Koshal (2007) - Mesa (2002) Pilloni (2011) Xu (2004) Fawzy ElSayed (2012) Authors’ conclusion NAE Subgingival application of HY following ultrasonic mechanical instrumentation is beneficial for improving periodontal parameters. NR Primary outcome of this study revealed that HY- and CHX-gel used as an adjunct to SRP can significantly improve the benefits of SRP. The adjunctive application of HY may have positive effects on PD reduction and may prevent recolonization by periodontopathogens. No statistical difference was found on radiographs in the non-surgical group, where a decrease in bone height was found for both groups after scaling. Probing depth reduction after SRP, was as expected. HY in contact with bone and soft tissues had no influence on the immune system in this study. NR NR NAE NR NR HY gel treatment induced a significant reduction in the proliferation index of the gingival epithelium. The reduction in the inflammatory infiltrate and in the proliferation of fibroblasts was not significant. - NR No difference between test and control sites was seen in the tested microorganisms (A.a., P.g., P.i., T.f., T.d.). NR Surgical treatment Briguglio (2013) Engström (2001) Adverse effects Bone height was increased in the test group approximately by 0.5 mm and reduced in the control group by approximately 0.4 mm (P <0.05) after 12 months. Immune responses evaluated by IgG, C3, PgE2 content in GCF showed no differences during the 12 months and in all groups, the microflora (Prevotella spp., P.g., or A.a) showed a stable microecology. - NAE Subgingival placement of 0.2% HY gel along with SRP provided a significant improvement in gingival parameters. However, no additional benefit was found in periodontal parameters. Histologically, experimental sites showed reduced inflammatory infiltrate, but it was not statistically significant. The local application of HY gel in conjunction with SRP may have a beneficial effect on periodontal health in patients with chronic periodontitis. Results have demonstrated highly significant improvements in the clinical variables of BoP and PD in the sites that received the HY compared to the placebo sites that had not received the active gel. It was concluded that highly significant improvements in healing after non-surgical therapy can be achieved by a single topical application of HY immediately after root surface debridement. High molecular-weight HY gel reduces cell proliferation in epithelial cells such as fibroblasts and lymphocytes, abates the inflammatory process, and improves the periodontal lesion in patients with chronic periodontitis. It appears that an esterified gel form of HY has shown an effect in reducing the gingival inflammation when used as an adjunct to mechanical home plaque control and that it could be successfully used to improve the periodontal clinical indexes. No clinical or microbiological improvement was achieved by the adjunctive use of HY gel compared to SRP alone. Only GCF rate was affected by the use of HY in terms of a more rapid reduction of GCF rate in the test sites. NR The treatment of intrabony defects with HY offered an additional benefit in terms of CAL gain, PD reduction, and predictability compared to treatment with OFD. NR The observed difference in bone height between test and control sites after 12 months was less than 1 mm, which was only detectable on radiographs. PD reduction was as expected. HY in contact with bone and soft tissues had no influence on the immune system in this study. NR HY gel application in conjunction with periodontal surgery appears to result in significant improvement of CAL and in a reduction in gingival recession. HY gel application appears to improve the clinical outcome of MWF surgery. A.a. - Aggregatibacter actinomycetemcomitans, BoP - bleeding on probing, C3 - complement factor 3, CHX - chlorhexidine, C.r. - Campylobacter rectus, DLC - differential leukocyte count, GCF - gingival crevicular fluid, HY - hyaluronan, IgG immuneglobulin G, NAE - no adverse effects, NR - not reported, N.S. - not significant, PD - probing pocket depth, PgE2 - prostaglanind E2, P.g. - Porphyromonas gingivalis, P.i. - Prevotella intermedia, P.i. - Prevotella intermedia, SRP - scaling & root planing, T.f. - Tannerella forsythia, T.d. - Treponema denticola, TLC - total leukocyte count