Initial Credentialing Requirements
advertisement

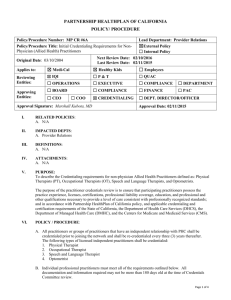
PARTNERSHIP HEALTHPLAN OF CALIFORNIA POLICY/ PROCEDURE Policy/Procedure Number: MP CR #4 Policy/Procedure Title: Initial Credentialing Requirements Lead Department: Provider Relations ☒External Policy ☐ Internal Policy Next Review Date: 08/10/2016 Last Review Date: 08/12/2015 Original Date: 11/01/1998 Applies to: ☒ Medi-Cal ☒ Healthy Kids ☐ Employees Reviewing Entities: ☒ IQI ☐P&T ☒ QUAC ☐ OPERATIONS ☐ EXECUTIVE ☐ COMPLIANCE ☐ DEPARTMENT ☐ BOARD ☐ COMPLIANCE ☐ FINANCE ☐ PAC ☒ CREDENTIALING ☐ DEPT. DIRECTOR/OFFICER Approving Entities: ☐ CEO ☐ COO Approval Signature: Marshall Kubota, MD Approval Date: 08/12/2015 I. RELATED POLICIES: A. N/A II. IMPACTED DEPTS: A. N/A III. DEFINITIONS: A. N/A IV. ATTACHMENTS: A. Addendum to CPPA "Notice to Practitioners of Credentialing Rights and Responsibilities." V. PURPOSE: A. To describe the Credentialing Requirements for Medical Doctor (M.D.), Doctor of Osteopathy (D.O.), Doctor of Podiatric Medicine (D.P.M.), Doctor of Chiropractic (D.C.), Doctor of Dental Surgery (DDS), Certified Acupuncturist B. The purpose of the practitioner credentials review is to ensure that participating practitioners possess the practice experience, licenses, certifications, privileges, professional liability coverage, education, and professional and other qualifications necessary to provide a level of care consistent with professionally recognized standards; and in accordance with Partnership HealthPlan of California policy, and applicable credentialing and certification requirements of the State of California, the Department of Health Care Services (DHCS), the Department of Managed Health Care (DMHC), and the Centers for Medicare and Medicaid Services (CMS). VI. POLICY / PROCEDURE: A. All practitioners or groups of practitioners that have an independent relationship with PHC shall be credentialed prior to joining the network and shall be re-credentialed every three (3) years thereafter. If a practitioner terminates with the Plan and later is reinstated the Plan will initially credential the practitioner if the break is 30 days or more. Primary Care Physicians and OB/GYN Specialist Physician must have had an office site audit, as defined in the Practitioner Facility Site Review Policy, prior to having credentials presented to the Credentialing Committee. Document1 Page 1 of 12 Policy/Procedure Number: MP CR #4 Lead Department: Provider Relations ☒ External Policy ☐ Internal Policy Next Review Date: 08/10/2016 Last Review Date: 08/12/2015 ☒ Healthy Kids ☐ Employees Policy/Procedure Title: Initial Credentialing Requirements Original Date: 11/01/1998 ☒ Medi-Cal Applies to: The following types of licensed independent practitioners shall be credentialed: 1. 2. 3. 4. 5. 6. Medical Doctor (M.D.) Doctor of Osteopathy (D.O.) Doctor of Podiatric Medicine (D.P.M.) Doctor of Chiropractic (D.C.) Doctor of Dental Surgery (DDS) Certified Acupuncturist B. Individual professional practitioners must meet all of the requirements outlined below. All documentation and information required may not be more than 180 days old at the time of Credentials Committee review. 1. Medical Doctor (M.D.) a. Must submit a completed signed California Participating Physician Application (CPPA) that includes disclosure of professional liability history and a current Curriculum Vitae (CV) that details the practitioner's work history. All confidential questions on the Attestation must be answered and any exceptions must be explained in writing by the applicant. A current release form must be signed and dated in order to begin the credentialing process. b. Must possess a current, valid, unencumbered, unrestricted, and nonprobationary license in the states where he or she provides services to PHC members. Exception to this requirement may be made for those applicants whose licensure action was related to substance abuse and who have demonstrated a minimum of six months of successful participation in a treatment or monitoring program; should this exception be entertained, the HealthPlan may request specific documentation from the applicant’s treating physician or program as we deem appropriate and to the extent permitted by law. Under existing federal law, licensed health professionals employed by a tribal health program are required to be exempt, if licensed in any state, from the licensing requirements of the state in which the tribal health program performs specified services. The tribal health professional's license must be in good standing as stated above. 1) Practitioners that don’t meet criteria of an unencumbered, unrestricted, and nonprobationary license will be presented to the Credentials Committee for consideration. Based on the review of the issues presented, the Credentials Committee will make recommendations to deny credentialing or approve credentialing. The Plan will routinely ask practitioners to send a letter to the Credentials Committee to give their narrative and explanation of the action against them and the activities the practitioner has taken as a result of restrictions placed on their medical license. Approval of credentialing would be based on specific requirements that could include but not limited to; required proctoring of practitioner, additional CME within a specified time frame, monitoring of practitioner’s restrictions by the health plan credentials staff and findings brought back to committee on a monthly or quarterly basis, and/or limiting the type of services provided by the practitioner to PHC members. This would apply to any practitioner with sanctions or limitations on their medical license from the license governing Board. Document1 Page 2 of 12 Policy/Procedure Number: MP CR #4 Lead Department: Provider Relations ☒ External Policy ☐ Internal Policy Next Review Date: 08/10/2016 Last Review Date: 08/12/2015 ☒ Healthy Kids ☐ Employees Policy/Procedure Title: Initial Credentialing Requirements Original Date: 11/01/1998 Applies to: ☒ Medi-Cal 2) The following criteria will be used by the Credentials Committee to evaluate the practitioner. a) Assessment of risk of substandard care that might be provided to Plan members b) The completeness and forthrightness of the provider’s narrative and explanation of the probation, restriction or other encumberment on their medical license. c. Physician must be free of any sanctions or limitations on their license from the California State Medical Licensure Board. Under existing federal law, licensed health professionals employed by a tribal health program are required to be exempt, if licensed in any state, from the licensing requirements of the state in which the tribal health program performs specified services. The tribal health professional's license must be in good standing as stated above. d. Must have professional liability coverage in the amount of $1,000,000 per incident and $3,000,000 in aggregate. e. Must possess and submit a copy of a current, unrestricted DEA Certificate in order to prescribe controlled substances. f. Primary source verification of Medical school and residency program is required. Primary source verification of Medical school is verified by the Medical Board of California (MBOC) prior to issuing a license. PHC may also verify physician data by searching the AMA Physician Profile via a secure website. If practitioner is Board Certified, primary source verification of residency program is not required. If practitioner is not Board Certified PHC will verify residency. g. Privileges at a JCAHO or HFAP accredited or Medicare verified hospital, primary admitting facility without restrictions. h. Practitioners that do not have hospital privileges must have an agreement with a physician or group. The practitioner must furnish PHC with written verification of this agreement. Documents are placed in practitioner’s paper file. i. For Practitioners that attest to being Board Certified, Board Certification is verified through ABMS. j. Practitioners must be free of Medicare/Medi-Cal sanctions. This is done through a query of the National Practitioner Data Bank/Healthcare Integrity and Protection Data Bank (NPDB/HIPDB). k. A query and documentation is obtained from the NPDB/HIPDB. l. Verification of Medi-Cal status through query of PHC Provider Master File (PMF) database. This database is updated monthly through data submission from the Department of Health Services (DHS) to PHC. m. Verification of Medicare participation through query of Medicare website, www.medicare.gov and/or other reporting agencies. Verify that Provider has not opted out of Medicare. Document1 Page 3 of 12 Policy/Procedure Number: MP CR #4 Lead Department: Provider Relations ☒ External Policy ☐ Internal Policy Next Review Date: 08/10/2016 Last Review Date: 08/12/2015 ☒ Healthy Kids ☐ Employees Policy/Procedure Title: Initial Credentialing Requirements Original Date: 11/01/1998 Applies to: ☒ Medi-Cal 2. Doctor of Osteopathy (D.O.) a. Must submit a completed signed California Participating Physician Application (CPPA) that include disclosure of professional liability history and a current Curriculum Vitae (CV) that details the practitioners work history. All confidential questions on the Attestation must be answered and any exceptions must be explained in writing by the applicant. A current release form must be signed and dated in order to begin the credentialing process. b. Must possess a current, valid, unencumbered, unrestricted, and nonprobationary license in the states where he or she provides services to PHC members. Exception to this requirement may be made for those applicants whose licensure action was related to substance abuse and who have demonstrated a minimum of six months of successful participation in a treatment or monitoring program; should this exception be entertained, the HealthPlan may request specific documentation from the applicant’s treating physician or program as we deem appropriate and to the extent permitted by law. 1) Practitioners that don’t meet criteria of an unencumbered, unrestricted, and nonprobationary license will be presented to the Credentials Committee for consideration. Based on the review of the issues presented, the Credentials Committee will make recommendations to deny credentialing or approve credentialing. The Plan will routinely ask practitioners to send a letter to the Credentials Committee to give their narrative and explanation of the action against them and the activities the practitioner has taken as a result of restrictions placed on their medical license. Approval of credentialing would be based on specific requirements that could include but not limited to; required proctoring of practitioner, additional CME within a specified time frame, monitoring of practitioner’s restrictions by the health plan credentials staff and findings brought back to committee on a monthly or quarterly basis, and/or limiting the type of services provided by the practitioner to PHC members. This would apply to any practitioner with sanctions or limitations on their medical license from the license governing Board. 2) The following criteria will be used by the Credentials Committee to evaluate the practitioner. a) Assessment of risk of substandard care that might be provided to Plan members b) The completeness and forthrightness of the provider’s narrative and explanation of the probation, restriction or other encumberment on their medical license. c. The Osteopathic physician must be free of any sanctions or limitations on their license from the Osteopathic Medical Board of California. Under existing federal law, licensed health professionals employed by a tribal health program are required to be exempt, if licensed in any state, from the licensing requirements of the state in which the tribal health program performs specified services. The tribal health professional's license must be in good standing as stated above. d. Must have professional liability coverage in the amount of $1,000,000 per incident and $3,000,000 in aggregate. e. Document1 Must possess and submit a copy of a current, unrestricted DEA Certificate in order to prescribe controlled substances. Page 4 of 12 Policy/Procedure Number: MP CR #4 Lead Department: Provider Relations ☒ External Policy ☐ Internal Policy Next Review Date: 08/10/2016 Last Review Date: 08/12/2015 ☒ Healthy Kids ☐ Employees Policy/Procedure Title: Initial Credentialing Requirements Original Date: 11/01/1998 Applies to: ☒ Medi-Cal f. Primary source verification of Medical school and residency is verified by the Osteopathic Medical Board of California prior to issuing a license. g. Privileges at a JCAHO or HFAP accredited or Medicare verified hospital, primary admitting facility without restrictions. h. Practitioners that do not have hospital privileges must have an agreement with a physician or group. The practitioner must furnish PHC with written verification of this agreement. Documents are placed in practitioner’s paper file. i. For Practitioners that attest to being Board Certified, Board Certification is verified through the Osteopathic Board. j. Practitioners must be free of Medicare/Medi-Cal sanctions. This is done through a query of the National Practitioner Data Bank/Healthcare Integrity and Protection Data Bank (NPDB/HIPDB). k. A query and documentation is obtained from the NPDB/HIPDB. l. Verification of Medi-Cal status through query of PHC Provider Master File (PMF) database. This database is updated monthly through data submission from the Department of Health Services (DHS) to PHC. m. Verification of Medicare participation through query of Medicare website, www.medicare.gov and/or other reporting agency. Verify that Provider has not opted out of Medicare. 3. Doctor of Podiatric Medicine (D.P.M.) a. Must submit a completed signed California Participating Physician Application (CPPA) that includes disclosure of professional liability history and a current Curriculum Vitae (CV) that details the practitioner's work history. All confidential questions on the Attestation must be answered and any exceptions must be explained in writing by the applicant. A current release form must be signed and dated in order to begin the credentialing process. b. Must possess a current, valid, unencumbered, unrestricted, and nonprobationary license in the states where he or she provides services to PHC members. Exception to this requirement may be made for those applicants whose licensure action was related to substance abuse and who have demonstrated a minimum of six months of successful participation in a treatment or monitoring program; should this exception be entertained, the HealthPlan may request specific documentation from the applicant’s treating physician or program as we deem appropriate and to the extent permitted by law. 1) Document1 Practitioners that don’t meet criteria of an unencumbered, unrestricted, and nonprobationary license will be presented to the Credentials Committee for consideration. Based on the review of the issues presented, the Credentials Committee will make recommendations to deny credentialing or approve credentialing. The Plan will routinely ask practitioners to send a letter to the Credentials Committee to give their narrative and explanation of the action against them and the activities the practitioner has taken as a result of restrictions placed on their medical license. Approval of credentialing would be based Page 5 of 12 Policy/Procedure Number: MP CR #4 Lead Department: Provider Relations ☒ External Policy ☐ Internal Policy Next Review Date: 08/10/2016 Last Review Date: 08/12/2015 ☒ Healthy Kids ☐ Employees Policy/Procedure Title: Initial Credentialing Requirements Original Date: 11/01/1998 Applies to: ☒ Medi-Cal on specific requirements that could include but not limited to; required proctoring of practitioner, additional CME within a specified time frame, monitoring of practitioner’s restrictions by the health plan credentials staff and findings brought back to committee on a monthly or quarterly basis, and/or limiting the type of services provided by the practitioner to PHC members. This would apply to any practitioner with sanctions or limitations on their medical license from the license governing Board. 2) The following criteria will be used by the Credentials Committee to evaluate the practitioner. a) Assessment of risk of substandard care that might be provided to Plan members b) The completeness and forthrightness of the provider’s narrative and explanation of the probation, restriction or other encumberment on their medical license. c. Podiatrist must be free of any sanctions or limitations on license from the Board of Podiatric Medicine of California. Under existing federal law, licensed health professionals employed by a tribal health program are required to be exempt, if licensed in any state, from the licensing requirements of the state in which the tribal health program performs specified services. The tribal health professional's license must be in good standing as stated above. d. Must have professional liability coverage in the amount of $1,000,000 per incident and $3,000,000 in aggregate. e. Must possess and submit a copy of a current, unrestricted DEA Certificate in order to prescribe controlled substances. f. Primary source verification of Medical school and residency is verified by the Board of Podiatric Medicine prior to issuing a license. g. Privileges at a JCAHO or HFAP accredited or Medicare verified hospital, primary admitting facility without restrictions. h. Practitioners that do not have hospital privileges must have an agreement with a physician or group. The practitioner must furnish PHC with written verification of this agreement. Documents are placed in practitioner’s paper file. i. For practitioners that attest to being Board Certified, Board Certification is verified through the Board of Podiatric Medicine of California. j. Practitioner must be free of Medicare/Medi-Cal sanctions. This is done through a query of the National Practitioner Data Bank/Healthcare Integrity and Protection Data Bank (NPDB/HIPDB). k. A query and documentation is obtained from the NPDB/HIPDB. Document1 Page 6 of 12 Policy/Procedure Number: MP CR #4 Lead Department: Provider Relations ☒ External Policy ☐ Internal Policy Next Review Date: 08/10/2016 Last Review Date: 08/12/2015 ☒ Healthy Kids ☐ Employees Policy/Procedure Title: Initial Credentialing Requirements Original Date: 11/01/1998 ☒ Medi-Cal Applies to: l. Verification of Medi-Cal status through query of PHC Provider Master File (PMF) database. This database is updated monthly through data submission from the Department of Health Services (DHS) to PHC. m. Verification of Medicare participation through query of Medicare website, www.medicare.gov and/or other reporting agencies. Verify that Provider has not opted out of Medicare. 4. Doctor of Chiropractic (D.C.) a. Must submit a completed signed California Participating Physician Application (CPPA) that includes disclosure of professional liability history and a current Curriculum Vitae (CV) that details the practitioners work history. All confidential questions on the Attestation must be answered and any exceptions must be explained in writing by the applicant. A current release form must be signed and dated in order to begin the credentialing process. b. Must possess a current, valid, unencumbered, unrestricted, and nonprobationary license in the states where he or she provides services to PHC members. Exception to this requirement may be made for those applicants whose licensure action was related to substance abuse and who have demonstrated a minimum of six months of successful participation in a treatment or monitoring program; should this exception be entertained, the HealthPlan may request specific documentation from the applicant’s treating physician or program as we deem appropriate and to the extent permitted by law. Practitioners that don’t meet criteria of an unencumbered, unrestricted, and nonprobationary license will be presented to the Credentials Committee for consideration. Based on the review of the issues presented, the Credentials Committee will make recommendations to deny credentialing or approve credentialing. The Plan will routinely ask practitioners to send a letter to the Credentials Committee to give their narrative and explanation of the action against them and the activities the practitioner has taken as a result of restrictions placed on their medical license. Approval of credentialing would be based on specific requirements that could include but not limited to; required proctoring of practitioner, additional CME within a specified time frame, monitoring of practitioner’s restrictions by the health plan credentials staff and findings brought back to committee on a monthly or quarterly basis, and/or limiting the type of services provided by the practitioner to PHC members. This would apply to any practitioner with sanctions or limitations on their medical license from the license governing Board. 2) The following criteria will be used by the Credentials Committee to evaluate the practitioner. a) Assessment of risk of substandard care that might be provided to Plan members b) The completeness and forthrightness of the provider’s narrative and explanation of the probation, restriction or other encumberment on their medical license. 1) c. Document1 Chiropractor must be free of any sanctions or limitations on the license from the California State Chiropractic Board. Under existing federal law, licensed health professionals employed by a tribal health program are required to be exempt, if licensed in any state, from the licensing requirements of the state in which the tribal health program performs specified services. The tribal health professional's license must be in good standing as stated above. Page 7 of 12 Policy/Procedure Number: MP CR #4 Lead Department: Provider Relations ☒ External Policy ☐ Internal Policy Next Review Date: 08/10/2016 Last Review Date: 08/12/2015 ☒ Healthy Kids ☐ Employees Policy/Procedure Title: Initial Credentialing Requirements Original Date: 11/01/1998 Applies to: ☒ Medi-Cal d. Must have professional liability coverage in the amount of $1,000,000 per incident and $3,000,000 in aggregate. e. Primary source verification of Chiropractic school is verified by the California Chiropractic Board prior to issuing a license. f. Practitioner must be free of Medicare/Medi-Cal sanctions. This is done through a query of the National Practitioner Data Bank/Healthcare Integrity and Protection Data Bank (NPDB/HIPDB). g. A query and documentation is obtained from the (NPDB/HIPDB). h. Verification of Medi-Cal status through query of PHC Provider Master File (PMF) database. This database is updated monthly through data submission from the Department of Health Services (DHS) to PHC. i. Verification of Medicare participation through query of Medicare website, www.medicare.gov and/or other reporting agencies. Verify that Provider has not opted out of Medicare. 5. Doctor of Dental Surgery (DDS) a. Must submit a completed signed California Participating Physician Application (CPPA) that include disclosure of professional liability history and a current Curriculum Vitae (CV) that details the practitioners work history. All confidential questions on the Attestation must be answered and any exceptions must be explained in writing by the applicant. A current release form must be signed and dated in order to begin the credentialing process. b. Must possess a current, valid, unencumbered, unrestricted, and nonprobationary license in the states where he or she provides services to PHC members. Exception to this requirement may be made for those applicants whose licensure action was related to substance abuse and who have demonstrated a minimum of six months of successful participation in a treatment or monitoring program; should this exception be entertained, the HealthPlan may request specific documentation from the applicant’s treating physician or program as we deem appropriate and to the extent permitted by law. 1) Practitioners that don’t meet criteria of an unencumbered, unrestricted, and nonprobationary license will be presented to the Credentials Committee for consideration. Based on the review of the issues presented, the Credentials Committee will make recommendations to deny credentialing or approve credentialing. The Plan will routinely ask practitioners to send a letter to the Credentials Committee to give their narrative and explanation of the action against them and the activities the practitioner has taken as a result of restrictions placed on their medical license. Approval of credentialing would be based on specific requirements that could include but not limited to; required proctoring of practitioner, additional CME within a specified time frame, monitoring of practitioner’s restrictions by the health plan credentials staff and findings brought back to committee on a monthly or quarterly basis, and/or limiting the type of services provided by the practitioner to PHC members. This would apply to any practitioner with sanctions or limitations on their medical license from the license governing Board. Document1 Page 8 of 12 Policy/Procedure Number: MP CR #4 Lead Department: Provider Relations ☒ External Policy ☐ Internal Policy Next Review Date: 08/10/2016 Last Review Date: 08/12/2015 ☒ Healthy Kids ☐ Employees Policy/Procedure Title: Initial Credentialing Requirements Original Date: 11/01/1998 Applies to: ☒ Medi-Cal 2) The following criteria will be used by the Credentials Committee to evaluate the practitioner. a) Assessment of risk of substandard care that might be provided to Plan members b) The completeness and forthrightness of the provider’s narrative and explanation of the probation, restriction or other encumberment on their medical license. c. The Dentist must be free of any sanctions or limitations on their license from the Dental Board of California. Under existing federal law, licensed health professionals employed by a tribal health program are required to be exempt, if licensed in any state, from the licensing requirements of the state in which the tribal health program performs specified services. The tribal health professional's license must be in good standing as stated above. d. Must have professional liability coverage in the amount of $1,000,000 per incident and $3,000,000 in aggregate. e. Must possess and submit a copy of a current, unrestricted DEA Certificate in order to prescribe controlled substances. f. Primary source verification of Dental school and residency is verified by the Dental Board of California prior to issuing a license. g. Privileges at a JCAHO or HFAP accredited or Medicare verified hospital, primary admitting facility without restrictions. h. Practitioners that do not have hospital privileges must have an agreement with a physician or group. The practitioner must furnish PHC with written verification of this agreement. Documents are placed in practitioner’s paper file. i. For practitioners that attest to being Board Certified, Board Certification is verified through the American Board of Oral/Maxiofacial Surgery. j. Practitioner must be free of Medicare/Medi-Cal and or Denti-Cal sanctions. This is done through a query of the National Practitioner Data Bank/Healthcare Integrity and Protection Data Bank (NPDP/HIPDB). k. A query and documentation is obtained from the NPDB/HIPDB. l. Verification of Medi-Cal status through query of PHC Provider Master File (PMF) database. This database is updated monthly through data submission from the Department of Health Services (DHS) to PHC. m. Verification of Medicare participation through query of Medicare website, www.medicare.gov and/or other reporting agencies. Verify that Provider has not opted out of Medicare. 6. Certified Acupuncturist (non-physician) a. Document1 Must submit a completed signed California Participating Physician Application (CPPA) that include disclosure of professional liability history and a current Curriculum Vitae (CV) that details the practitioners work history. All confidential questions on the Attestation must be Page 9 of 12 Policy/Procedure Number: MP CR #4 Lead Department: Provider Relations ☒ External Policy ☐ Internal Policy Next Review Date: 08/10/2016 Last Review Date: 08/12/2015 ☒ Healthy Kids ☐ Employees Policy/Procedure Title: Initial Credentialing Requirements Original Date: 11/01/1998 Applies to: ☒ Medi-Cal answered and any exceptions must be explained in writing by the applicant. A current release form must be signed and dated in order to begin the credentialing process. b. Must possess a current, valid, unencumbered, unrestricted, and nonprobationary license in the states where he or she provides services to PHC members. Exception to this requirement may be made for those applicants whose licensure action was related to substance abuse and who have demonstrated a minimum of six months of successful participation in a treatment or monitoring program; should this exception be entertained, the HealthPlan may request specific documentation from the applicant’s treating physician or program as we deem appropriate and to the extent permitted by law. Practitioners that don’t meet criteria of an unencumbered, unrestricted, and nonprobationary license will be presented to the Credentials Committee for consideration. Based on the review of the issues presented, the Credentials Committee will make recommendations to deny credentialing or approve credentialing. The Plan will routinely ask practitioners to send a letter to the Credentials Committee to give their narrative and explanation of the action against them and the activities the practitioner has taken as a result of restrictions placed on their medical license. Approval of credentialing would be based on specific requirements that could include but not limited to; required proctoring of practitioner, additional CME within a specified time frame, monitoring of practitioner’s restrictions by the health plan credentials staff and findings brought back to committee on a monthly or quarterly basis, and/or limiting the type of services provided by the practitioner to PHC members. This would apply to any practitioner with sanctions or limitations on their medical license from the license governing Board. 2) The following criteria will be used by the Credentials Committee to evaluate the practitioner. a) Assessment of risk of substandard care that might be provided to Plan members b) The completeness and forthrightness of the provider’s narrative and explanation of the probation, restriction or other encumberment on their medical license. 1) c. The acupuncturist must be free of any sanctions or limitations on their license from the California State Acupuncture Board. Under existing federal law, licensed health professionals employed by a tribal health program are required to be exempt, if licensed in any state, from the licensing requirements of the state in which the tribal health program performs specified services. The tribal health professional's license must be in good standing as stated above. d. Must have professional liability coverage in the amount of $1,000,000 per incident and $3,000,000 in aggregate. Document1 e. Primary source verification of completion of acupuncture school is verified by the State of California Acupuncture Board prior to issuing a license. f. Practitioners must be free of Medicare/Medi-Cal sanctions. This is done through a query of the National Practitioner Data Bank/Healthcare Integrity and Protection Data Bank (NPDB/HIPDB). Page 10 of 12 Policy/Procedure Number: MP CR #4 Lead Department: Provider Relations ☒ External Policy ☐ Internal Policy Next Review Date: 08/10/2016 Last Review Date: 08/12/2015 ☒ Healthy Kids ☐ Employees Policy/Procedure Title: Initial Credentialing Requirements Original Date: 11/01/1998 Applies to: ☒ Medi-Cal g. A query and documentation is obtained from the NPDB/HIPDB. h. Verification of Medi-Cal status through query of PHC Provider Master File (PMF) database. This database is updated monthly through data submission from the Department of Health Services (DHS) to PHC. i. Physicians providing acupuncture: In order for a physician to perform acupuncture services for PHC members the physician must submit documentation of at least 200 hours of formal training in the field of acupuncture and meet all the PHC credentialing requirements for Medical Doctor (M.D.) or Doctor of Osteopathy (D.O.) C. The process for identifying issues in the credentialing, re-credentialing process is identified in the PHC Review Standards for Credentials, Re-credentials Policy MP CR#5. D. Practitioners are notified in writing when presented with a credentialing application that they have a right to be informed of the status of their application upon request, a right to review any portion of their personal credentials file related to information submitted in support of their credentialing application, and they have the right to correct any identified erroneous information, provided the information is not peer review protected. (See Addendum to CPPA “Notice of Practitioners of Credentialing Rights/Responsibilities.) E. The Credentials Committee shall review and evaluate the credentialing application and supporting documentation to determine if the practitioner meets the credentialing criteria regarding approval or denial. F. If the Credentialing Committee does not approve a practitioner for credentialing, the practitioner will be notified of the decision in writing. The practitioner may appeal the decision using the process as identified in Fair Hearing Process for Adverse Decisions policy. The Partnership HealthPlan of California of Commissioners retains ultimate responsibility for final decisions on all appeals related to practitioner credentialing activities. G. If a practitioner's credentialing profile is denied base upon deficiencies in the practitioner’s professional competence, conduct or quality of care, PHC shall submit any and all required reports to the National Practitioner Data Bank and the State Medical Board as outlined in MP CR#9A, Reporting to the Medical Board of California and the National Practitioner Data Bank. H. Upon approval the practitioner is notified of the decision in writing within 30 days. The new practitioner information is added to the member practitioner directories to include Board Certification and Specialty consistent with the information obtained during the credentialing process. I. Document1 The credentials files and all relevant credentialing and re-credentialing information are maintained as high level secured documents. Confidentiality is maintained via file storage in locked cabinets and access limited to the Chief Medical Officer, Health Services Director, Provider Relations Department Personnel, and the Quality Improvement Personnel. Practitioner information stored in an electronic database is confidential and secure, accessible only by personnel with unique passwords. Page 11 of 12 Policy/Procedure Number: MP CR #4 Lead Department: Provider Relations ☒ External Policy ☐ Internal Policy Next Review Date: 08/10/2016 Last Review Date: 08/12/2015 ☒ Healthy Kids ☐ Employees Policy/Procedure Title: Initial Credentialing Requirements Original Date: 11/01/1998 Applies to: ☒ Medi-Cal VII. REFERENCES: A. - NCQA VIII. DISTRIBUTION: A. PHC Provider Manual IX. POSITION RESPONSIBLE FOR IMPLEMENTING PROCEDURE: Credentialing Supervisor X. REVISION DATES: 2/1/2011, 12/13/2000, 7/11/2001, 9/11/2002, 3/12/2003, 3/10/2004, 9/8/2004, 11/10/2004, 11/9/2005, 7/12/2006, 7/11/2007, 7/8/2008, 9/4/2008, 7/8/2009, 7/14/2010, 7/13/2011, 8/8/2012, 10/9/2013, 8/13/2014, 2/11/2015 PREVIOUSLY APPLIED TO: N/A Document1 Page 12 of 12