Initial Credentialing Requirements for Non
advertisement

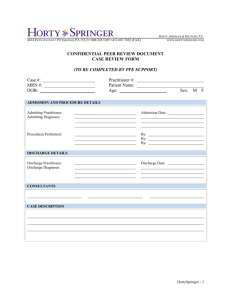
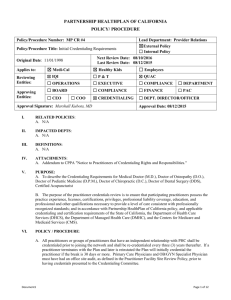
PARTNERSHIP HEALTHPLAN OF CALIFORNIA POLICY/ PROCEDURE Policy/Procedure Number: MP CR #6A Policy/Procedure Title: Initial Credentialing Requirements for NonPhysician (Allied Health) Practitioners Lead Department: Provider Relations ☒External Policy ☐ Internal Policy Next Review Date: 02/10/2016 Last Review Date: 02/11/2015 Original Date: 03/10/2004 Applies to: ☒ Medi-Cal ☒ Healthy Kids ☐ Employees Reviewing Entities: ☒ IQI ☐P&T ☐ QUAC ☐ OPERATIONS ☐ EXECUTIVE ☐ COMPLIANCE ☐ DEPARTMENT ☐ BOARD ☐ COMPLIANCE ☐ FINANCE ☐ PAC ☒ CREDENTIALING ☐ DEPT. DIRECTOR/OFFICER Approving Entities: ☐ CEO ☐ COO Approval Signature: Marshall Kubota, MD Approval Date: 02/11/2015 I. RELATED POLICIES: A. N/A II. IMPACTED DEPTS: A. Provider Relations III. DEFINITIONS: A. N/A IV. ATTACHMENTS: A. N/A V. PURPOSE: To describe the Credentialing requirements for non-physician Allied Health Practitioners defined as: Physical Therapists (PT), Occupational Therapists (OT), Speech and Language Therapists, and Optometrists. The purpose of the practitioner credentials review is to ensure that participating practitioners possess the practice experience, licenses, certifications, professional liability coverage, education, and professional and other qualifications necessary to provide a level of care consistent with professionally recognized standards; and in accordance with Partnership HealthPlan of California policy, and applicable credentialing and certification requirements of the State of California, the Department of Health Care Services (DHCS), the Department of Managed Health Care (DMHC), and the Centers for Medicare and Medicaid Services (CMS). VI. POLICY / PROCEDURE: A. All practitioners or groups of practitioners that have an independent relationship with PHC shall be credentialed prior to joining the network and shall be re-credentialed every three (3) years thereafter. The following types of licensed independent practitioners shall be credentialed: 1. Physical Therapist 2. Occupational Therapist 3. Speech and Language Therapist 4. Optometrist B. Individual professional practitioners must meet all of the requirements outlined below. All documentation and information required may not be more than 180 days old at the time of Credentials Committee review. Document1 Page 1 of 4 Policy/Procedure Number: MP CR #6A Lead Department: Provider Relations Policy/Procedure Title: Initial Credentialing Requirements for ☒ External Policy Non-Physician (Allied Health) Practitioners ☐ Internal Policy Next Review Date: 02/10/2016 Original Date: 03/10/2004 Last Review Date: 02/11/2015 ☒ Healthy Kids ☐ Employees Applies to: ☒ Medi-Cal The following credentialing requirements apply to Physical Therapists, Occupational Therapists, Speech and Language Therapist, and Optometrists: 1. Must submit a completed signed California Participating Physician Application (CPPA) that includes disclosure of professional liability history and a current Curriculum Vitae (CV) that details the practitioner's work history. All confidential questions on the Attestation must be answered and any exceptions must be explained in writing by the applicant. A current release form must be signed and dated in order to begin the credentialing process. 2. Must possess a current, valid, unencumbered, unrestricted, and nonprobationary license in the states where he or she provides services to PHC members. Exception to this requirement may be made for those applicants whose licensure action was related to substance abuse and who have demonstrated a minimum of six months of successful participation in a treatment or monitoring program; should this exception be entertained, the HealthPlan may request specific documentation from the applicant’s treating physician or program as we deem appropriate and to the extent permitted by law. Under existing federal law, licensed health professionals employed by a tribal health program are required to be exempt, if licensed in any state, from the licensing requirements of the state in which the tribal health program performs specified services. a. Practitioners that don’t meet criteria of an unencumbered, unrestricted, and non-probationary license will be presented to the Credentials Committee for consideration. Based on the review of the issues presented, the Credentials Committee will make recommendations to deny credentialing or approve credentialing. The Plan will routinely ask practitioners to send a letter to the Credentials Committee to give their narrative and explanation of the action against them and the activities the practitioner has taken as a result of restrictions placed on their medical license. Approval of credentialing would be based on specific requirements that could include but not limited to; required proctoring of practitioner, additional CME within a specified time frame, monitoring of practitioner’s restrictions by the health plan credentials staff and findings brought back to committee on a monthly or quarterly basis, and/or limiting the type of services provided by the practitioner to PHC members. This would apply to any practitioner with sanctions or limitations on their medical license from the license governing Board. b. The following criteria will be used by the Credentials Committee to evaluate the practitioner: 1) Assessment of risk of substandard care that might be provided to Plan members. 2) The completeness and forthrightness of the provider’s narrative and explanation of the probation, restriction or other encumberment on their medical license. Verification is done via internet with appropriate California Board. This information is into the credentials database. The verification document is filed in the practitioner’s credential file. 3. Practitioners must be free of any sanctions or limitations on their license from the California State Licensure Boards. This will be done at the time the license is verified. Document1 Page 2 of 4 Policy/Procedure Number: MP CR #6A Lead Department: Provider Relations Policy/Procedure Title: Initial Credentialing Requirements for ☒ External Policy Non-Physician (Allied Health) Practitioners ☐ Internal Policy Next Review Date: 02/10/2016 Original Date: 03/10/2004 Last Review Date: 02/11/2015 ☒ Healthy Kids ☐ Employees Applies to: ☒ Medi-Cal 4. Must have professional liability coverage in the amount of $1,000,000 per incident and $3,000,000 in aggregate. Practitioner must submit a current copy of malpractice coverage. The copy is retained in practitioner’s credentials file. Information is entered into credentialing database 5. Must possess and submit a copy of a current unrestricted DEA Certificate in order to prescribe controlled substances (if applicable). 6. Primary source verification of the highest level of learning. Primary source verification may be obtained in writing; by electronic access to information; by page copies of compendiums/directories; and/or by telephone communication. Oral and electronic verifications shall bear the signature/initials and date of the staff person who verifies the information. If practitioner is Board Certified, primary source verification of residency program is not required. If practitioner is not Board Certified PHC will verify residency. a. Physical Therapists’ Education and Training 1) Direct verification with MBOC issued license; or, 2) Confirmation from professional school attended. b. Occupational Therapists’ Education and Training 1) Direct verification with American Board of Occupational Therapy; or 2) Confirmation from professional school attended. c. Speech and Language Therapists’ Education and Training 1) Direct verification with MBOC issued license; or, 2) Confirmation from school attended. d. Optometrists Education and Training 1) Confirmation from Optometry Board; or 2) Confirmation from optometry school attended 7. Practitioners must be free of Medicare/Medi-Cal sanctions. This is done through a query of the National Practitioner Data Bank/Healthcare Integrity and Protection Data Bank (NPDB/HIPDB). 8. A query from the NPDB/HIPDB via internet is documented and added to the practitioner file. If information is found the NPDB/HIPDB search, a brief summary will be documented in the database to assist the Chief Medical Officer or physician designee in review of data. The hard copy print-out is filed in the practitioner’s credential file. 9. Verification of Medi-Cal status (and/or employer Medi-Cal status) through query of PHC Provider Master File (PMF) database. This database is updated monthly through data submission from the Department of Health Services (DHS) to PHC. 10. Verification of Medicare participation through query of Medicare website www.medicare.gov and/or other reporting agencies. Verify that Provider has not opted out of Medicare. C. The process for identifying issues in the credentialing, re-credentialing process is identified in the PHC Review Standards for Credentials, Re-credentials Policy MP CR#5. Document1 Page 3 of 4 Policy/Procedure Number: MP CR #6A Lead Department: Provider Relations Policy/Procedure Title: Initial Credentialing Requirements for ☒ External Policy Non-Physician (Allied Health) Practitioners ☐ Internal Policy Next Review Date: 02/10/2016 Original Date: 03/10/2004 Last Review Date: 02/11/2015 ☒ Healthy Kids ☐ Employees Applies to: ☒ Medi-Cal D. Practitioners are notified in writing when presented with a credentialing application that they have a right to be informed of the status of their application upon request a right to review any portion of their personal credentials file related to information submitted in support of their credentialing application, and they have the right to correct any identified erroneous information, provided the information is not peer review protected. (See Addendum to Application “Notice of Practitioners of Credentialing Rights/Responsibilities). E. The Credentials Committee shall review and evaluate the credentialing application and supporting documentation to determine if the practitioner meets the credentialing criteria regarding approval or denial. The practitioner will be informed of the Credentials Committee decision within 30 days. The Partnership HealthPlan of California Board of Commissions retains ultimate responsibility for final decisions on all appeals related to practitioner credentialing activities. F. If the Credentialing Committee does not approve a practitioner for credentialing, the practitioner will be notified of the decision in writing. The practitioner may appeal the decision using the process as identified in Credentialing Appeal, Peer Review and Fair Hearing Process policy. G. If a practitioner’s credentialing profile is denied base upon deficiencies in the practitioner’s professional competence, conduct or quality of care, PHC shall submit any and all required reports to the National Practitioner Data Bank and the State Medical Board as outlined in MP CR#9A, Reporting to the Medical Board of California and the National Practitioner Data Bank. H. The Provider Relations Department is responsible for confidentiality of all practitioner information. Access to practitioner information verified and/or stored in an electronic database is confidential and accessed only by personnel with a unique password. The credentials files and all relevant credentialing and re-credentialing information are maintained as high level secured documents. Confidentially is maintained via file storage in locked cabinets and access limited to the Chief Medical Officer or physician designee / Health Services Director, Provider Relations Department Personnel, and the Quality Improvement Personnel. VII. REFERENCES: A. - NCQA VIII. DISTRIBUTION: A. - PHC Provider Manual IX. POSITION RESPONSIBLE FOR IMPLEMENTING PROCEDURE: Credentialing Supervisor X. REVISION DATES: 03/10/2004, 11/10/2004, 11/09/2005, 07/12/2006, 07/11/2007, 07/09/2008, 09/04/2008, 08/08/2009, 07/14/2010, 07/13/2011, 08/08/2012, 10/09/2013, 08/13/2014 PREVIOUSLY APPLIED TO: N/A Document1 Page 4 of 4