Discussion - IME-USP - Universidade de São Paulo
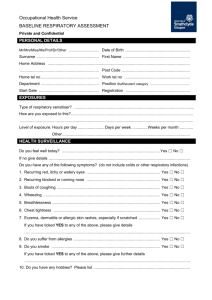
advertisement

Traffic air pollution effects on lung function: a study in outdoor workers with personal monitors in São Paulo, Brazil Authors Ubiratan Paula Santos¹ Maria Lucia Siqueira Bueno Garcia2 Alfésio Luís Ferreira Braga3,4 Paulo Afonso de André5 Claudia Sayuri Furukawa Oshiro2 Diogo Kogiso2 Beatriz Mangueira Saraiva-Romanholo2 Carmen D. Saldiva de André5,6 Julio M. Singer6 Paulo Hilário Nascimento Saldiva5 Affiliation ¹ MD, PhD, Pulmonary Division of Heart Institute (InCor) do Hospital das clínicas da Faculdade de Medicina da Universidade de São Paulo, Brazil 2 Laboratory of Experimental Therapeutics, Faculdade de Medicina da Universidade de São Paulo, Brazil 3 Environmental Epidemiology Study Group, Laboratory of Experimental Air Pollution, Faculdade de Medicina da Universidade de São Paulo, Brazil 4 Environmental Exposure and Risk Assessment Group, Collective Health Post- graduation Program, Catholic University of Santos, Brazil 5 Laboratory of Experimental Air Pollution, Department of Pathology, Faculdade de Medicina da Universidade de São Paulo, Brazil 6 Institute of Mathmatics and Statistics, Universidade de São Paulo, Brazil. Running title : Traffic Air Pollution and Lung Function Funding: Tecnology Science Ministry National Council of Tecnological and Scientific Development,(MCTI-CNPq, Edital 18/2006) Corresponding Author: Ubiratan de Paula Santos Divisão de Pneumologia do Instituto do Coração (InCor)-HCFMUSP Av Dr Eneas de Carvalho Aguiar 44, 5 andar, São Paulo, Brazil Cep: 05403-000 e-mail: pneubiratan@incor.usp.br All authors declare there are no competing interests 2 Abstract Background: chronic effects of outdoor air pollution on lung function in adults are still controversial, although some studies suggest a significant association. Objective: evaluate the chronic effect of exposure to different levels of traffic-generated PM2.5 on the lung function of outdoor workers in São Paulo, Brazil. Methods: in order to explore the effects of a wider range of exposures, three categories of workers were considered: taxi drivers and traffic controllers, expected to have a greater exposure, and Forest Institute rangers with an expected lower level of exposure. One hundred and one participants fulfilled the inclusion criteria. In an initial evaluation, anthropometric and clinical variables, asthma symptoms prevalence and the intake of fruits and vegetables per day were assessed. Participants were then scheduled to attend four visits (once a week for one month) in which they received a 24-hour personal PM2.5 sampler and have lung function tests, exhaled nitric oxide and exhaled CO measured in the following day. The volunteers were classified into three exposure groups according the tertiles of all individual measurements of PM2.5. The association between the spirometry variables and exposure was assessed by means of multiple robust regression models adjusted for age, waist circumference, time in job, daily work hours, diabetes or hypertension, environmental tobacco smoke, former smoking habits and number of fruit and vegetable servings per day. Results: workers with the highest level of exposure (> 39.6 g/m3) presented reductions on predicted FVC (-12.2%), FEV1 (9.1%), and increase in FEF2575/FVC (14.9%) without changes in FVC/FEV1 when compared to the lowest exposed group (< 25 g/m3). Conclusions: chronic exposure to vehicular traffic air pollution is associated with restrictive ventilatory effects. 3 Introduction Ambient air pollution has been linked to adverse health effects, especially on the cardiovascular and respiratory systems, with important impact on morbidity and mortality. A recent report (Lim et al. 2012) estimated that exposure to particulate matter (PM2.5) led to 3.2 million deaths in 2010. More recently the World Health Organization (World Health Organization 2014) ascribed 3.7 million deaths (6.7% of the total global deaths) to environmental pollution in 2012, with 40% attributed to cardiovascular diseases, 11% to chronic obstructive pulmonary diseases (COPD), 6% to lung cancer, and 3% to lower respiratory tract infections in children. In most cities, vehicular emissions represent the main source of atmospheric pollutants. Studies in different countries have revealed that both short and long-term exposure to traffic pollution are associated with increased morbidity and mortality from cardiopulmonary diseases (Brunekreef et al. 2009; Romieu et al. 2012). Chronic respiratory effects of air pollution have been associated to impairment of lung development in children and adolescents (Gauderman et al. 2004; Gauderman et al. 2007) and to increased incidence of asthma (McConnell et al. 2006). In adults, several studies (Andersen et al. 2011, Götschi et al. 2008, Kan et al. 2007) have evidenced lung function decline associated with chronic exposure, and suggested that the reduction in air pollution may improve lung function (Boogaard et al. 2013) or attenuate its decline with age (Downs et al. 2007). However, chronic effects of outdoor air pollution on lung function in adults is still controversial, although some studies suggest an effect even at low levels of pollutants (Adam et al. 2015; Schikowski et al. 2014). Acute effects of ambient levels of traffic pollution were observed in healthy adults (Rice et al. 2013; 4 Zuurbier et al. 2011), but the small number of studies and limitations in their designs maintains this subject still controversial (Health Effects Institute 2010). Outdoor workers in urban areas are more exposed to the mix of pollutants generated from automotive fleet. Indeed, in the urban scenario, there is a gradient of exposure related to the site where these professionals develop their activities (closer or farther from high traffic roads). Also, different categories of workers demand different physical activities and the healthy worker effect cannot be assumed to be present in all of them (Choudhary and Tarlo 2014). Our objective is to evaluate the chronic effect of exposure to different levels of trafficgenerated PM2.5 on the lung function of outdoor workers in the city of São Paulo. Methods This is an observational study approved by Ethics on Research Committee (CAPPesq) from Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo, number 0565/07. All participants signed an informed consent. Participants In order to explore the effects of a wider range of exposures, three categories of workers were selected. Two of them – taxi drivers and traffic controllers – were expected to have a greater exposure, whereas the third, workers of the Forest Institute rangers, were presumably submitted to lower levels of exposure, since they spent part of their daily life in a park in the outskirts of São Paulo. The inclusion criteria were: a) working on streets and/or avenues (traffic controllers or taxi drivers) or parks (Forest Institute in São Paulo) for, at least, two years; b) male; c) age between 18 to 65 years and d) nonsmoker or former smoker for over than one year (with air-exhaled carbon monoxide less than 6 ppm, measured in each of the clinical evaluations). 5 Taxi drivers were informed about the study and invited to a meeting through advertisements inserted in their union paper. Eighty two workers attended the first presentation, 64 attended a meeting for clinical evaluation and 57 fulfilled the inclusion criteria and were admitted to the study. Three hundred traffic controllers attended 6 meetings in the Traffic Engineering Company, 149 volunteered, 75 fulfilled the inclusion criteria and 26 remained to the end of the study. These participants work in the expanded central region of São Paulo. Forest Institute rangers (working in a park in the outskirts of the city) were recruited after a project presentation meeting at their institution, responsible for monitoring and preserving biodiversity in the State of São Paulo. Fifty workers attended the meeting, 23 fulfilled the inclusion criteria and showed up to the clinical evaluation, and 22 remained in the study. Study Design In the period from 2008 to 2012, each participant was followed at specified intervals within a month, and exposure and effect indicators were measured repeatedly with the objective of better evaluate the level of exposure and lung function during this short period. Participants were submitted to an initial evaluation that included recording of demographic characteristics, confirmation of the non-smoker condition, occupational, cardiorespiratory risks and clinical examination. After the initial evaluation, participants were scheduled, in pairs, to attend four visits (once a week for one month) in the Heart Institute of Faculdade de Medicina da Universidade de São Paulo. In each visit, they were submitted to a clinical evaluation to assess the occurrence of complications between the assessments, to have exhaled CO and exhaled NO measurements as well as to perform pulmonary function tests. 6 At 7:00 am on the eve of each clinical evaluation, each individual received a portable lightweight battery operated sampler installed in a shoulder bag to be carried during all day and kept nearby during sleeping period or baths, in order to record real 24 hours environmental exposure during. In the following day, before the clinical evaluation and the pulmonary function test, the monitor was withdrawn. All participants answered a structured food frequency questionnaire to evaluate the frequency of usual food consumption (Fisberg et al. 2008). The intake of fruit and vegetables, sources of antioxidant elements, was recorded as the number of servings per day. Anthropometric measures Weight in light clothes was measured to the nearest 100 g (Tanita scale) and height to the nearest 0.1 cm was measured barefoot with head in the horizontal Frankfort plane, using a Seca 208 stadiometer. Waist circumference midway between the lateral lower ribs and the iliac crest, and hip circumference at the widest part over the greater trochanters were measured according to standard protocols (World Health Organization 1989). Respiratory Symptoms and Lung Function All participants answered a questionnaire on asthma symptoms prevalence in the preceding 12 months (European Community Respiratory Health Survey 1996; Ribeiro et al. 2007). Spirometry was performed in the morning, with a KoKo spirometer (Pulmonary Data Services Instrumentation Inc., Louisville, USA), according to ATS/ERS recommendations (Miller et al. 2005a; Miller et al. 2005b), during morning periods. Three manoeuvres were carried out and the best one was chosen and analysed according to the ATS/ERS criteria (Pellegrino et al. 2005). The predicted values were 7 computed according the reference values recommended for the Brazilian population (Duarte et al. 2007; Pereira et al. 2007). Exhaled Nitric Oxide (NOex) Exhaled nitric oxide (NOex) was collected before each clinical evaluation, according to ATS standardization. Briefly, exhaled air was trapped in sealed balloons collected by a Siever Kit (Sievers Instruments Inc., Boulder, CO, USA) with a 0.3 m biologic filter HEPA (TROX Technik Ltda, SP, Brasil) and measured by chemiluminescence (Sievers apparatus NOA 280) . Before measurement, the NOex analyzer was tested daily by a filtering apparatus of ambient air (standardized mixture to transform NO into NO2 in 45ppb, the physiologic pattern, White Martins gases industriais AS, São Paulo SP, Brasil). The range of NOex among three measurements did not exceed 10% (American Thoracic Society 1999; American Thoracic Society Workshop 2006). PM2.5 concentration The sampler, designed by the Harvard School of Public Health, operates at a flow rate of 4 lpm through an impaction plate to obtain a PM2.5 cutoff. A silicone catheter connects the air inlet positioned at the volunteer shoulder to the sampler inflow. A vacuum pump powered by a rechargeable Li-Ion battery, model WR-5000 Aircheck from SKC, that incorporates a flow control and a chronometer, provides the necessary continuous air flow during the 24-hour sampling period. A polycarbonate membrane, a Whatman filter with a diameter of 37 mm and 0.8 pore size (part number 110809), installed inside the sampler after the impaction plate retains the particulate matter sampled. This membrane was weighed before and after the sampling process in an accurate 1 microgram Mettler Toledo scale, model UMX2, following a laboratorial protocol developed to control temperature and humidity (Miranda et al. 2012), estimating the total mass of particulate matter collected. The volume of air sampled is 8 obtained considering the 4 lpm pump flow and the sampling period recorded by the pump chronometer. The average daily concentration of PM2.5 was obtained dividing total mass by total air volume sampled. Statistical Analysis The tertiles of all individual measurements of PM2.5 were computed and the volunteers were classified according to them in three exposure groups: low, when all measures were lower than the first tertile, high, when all measures were higher than the second tertile and intermediate, otherwise. After defining the exposure groups, the analysis was based on the averages of the within-individual spirometry variables and baseline covariates. The means of the baseline and spirometry variables for the different groups of exposure were compared by a one-way analysis of variance. When residual diagnostic tools suggested coarse deviations from the model assumptions, the analysis was complemented by a Kruskal-Wallis test. To assess the association between passive smoking, respiratory symptoms, hypertension and/or diabetes and exposure to air pollution the likelihood ratio tests were considered. The association between spirometry variables and exposure, adjusted for age, waist circumference, time in job, daily work hours, diabetes or hypertension, environmental tobacco smoke, previous smoking habits and number of fruit and vegetable servings per day was assessed by means of multiple robust regression models based on MM-estimators (Yohai 1987) . The models were fitted via the lmrob function in the R software package (R Development Core Team 2013). 9 Results From the 83 traffic-exposed participants (taxi drivers and traffic controllers) four were excluded due to inconsistencies in the pulmonary function measurements. All 22 Forest Institute workers were included in the analyses. Participants who attended only one evaluation session were excluded resulting in a sample size of 101. 345 measures of PM2.5 and 359 pulmonary function tests were completed during the study period. Figure 1 presents the distribution of individual PM2.5 measurements. Particulate matter measurements smaller than 25 g/m3 were observed in the group of traffic controllers and taxi drivers, while some forest rangers were exposed to concentrations above this value. The observed values of the PM2.5 tertiles were 25 g/m3 and 39.6 g/m3. The mean concentration of PM2.5 was 17.8 g/m3 (standard deviation= 3.5 g/m3) in the low exposure group, 36.6 g/m3 (standard deviation= 10.8 g/m3) in the medium exposure group and 67.4 g/m3 (standard deviation= 14.1 g/m3) in the high exposure group. Table 1 presents demographic and clinical characterization according to exposure groups. The three groups of exposure are quite similar in terms of age, waist circumference and body mass index (BMI). On average, participants in the low exposure group have worked in the same function for a longer period and have less work shifts than those in the other groups. Table 2 presents descriptive statistics for symptoms, exhaled nitric oxide (NOex) and lung function data. Participants in the high exposure group tend to present smaller FEV1 values and higher FEF25-75 when compared to those in the other groups. The prevalence of respiratory symptoms was higher in the medium exposure group, although prevalence of wheezing was similar in the three groups. In general, we observed a decrease of FVC% and FEV1% from the low exposure to the high exposure group, 10 although without statistical significance. On the other hand, a significant increase of FEF25-75% without a decrease of FEV1/FVC was observed. In Table 3 we highlight the adverse effects on spirometry parameters observed in the PM2.5 high and medium exposure groups when compared to the low exposure group. In order to verify the robustness of the observed findings, we performed a sensitivity analysis, progressively adding more explanatory variables to check how the estimates were affected across different model specifications. Because only 86 participants filled out the food consumption questionnaire and there is no statistical significant differences among the mean intake of fruit and vegetables in the three exposure groups, this variable was not included. The estimates for FVC, FEV1, and FEF25-75% remained reasonably stable for the different sets of explanatory variables considered. In the high exposure group smaller FVC and FEV1 values were observed. Also, in the same group, FEF25-75% values were higher with no statistically significant differences detected for FEV1/FVC. Discussion This study suggests that individuals chronically exposed to ambient levels of traffic pollution present significant alterations in pulmonary function. Moreover, the results indicate that exposure to ambient traffic pollution vary markedly across individuals, and, being more evident in individuals with high exposure. The observed findings were robust and remained reasonably stable for the different sets of explanatory variables considered. Reductions in FVC and FEV1 were not accompanied by a reduction in FEV1/FVC, but an increase in FEF25-75% was observed suggesting a restrictive lung effect. A similar effect, with reduced FVC and FEV1, but no reduction of FEV1/FVC has been observed after exposure to ozone probably due to change in airways hysteresis compared with the parenchymal hysteresis (Kjaergaard et al. 2004). 11 A strength of this study is the more precise characterization of the differences in personal exposure to ambient pollution obtained via personal monitoring (24 hours PM2.5). Exposure to PM2.5 measured by personal equipment seems to be more appropriate to assess daily experience of exposure including work shift, time in commuting and at home. In fact, our results reinforce the concept that urban dwellers may experience a considerable variation of exposure, depending on their habits and work characteristics, since the difference between the means of the PM 2.5 in the high and low exposure groups is almost 50 µg/m3. More than 75% of the participants (classified in the medium level) were exposed to a mean concentration of 36.6 μg/m3, exceeding the recommended daily concentration of 25 μg/m3 suggested by WHO (World Health Organization 2006). Considering such a scenario the detection of significant differences among the groups is indeed impressive. Most probably our results underestimate the effects of air pollution on lung function, since there is not a group without chronic exposure, since all participants live in São Paulo, a city known to have high levels of air pollution. Most of the studies that have focused on chronic (Götschi et al. 2008; Sava and Carlsten 2012; Schikowski et al. 2005) and acute (Sava and Carlsten 2012; Strak et al. 2012) effects of air pollution on pulmonary function suggest a reduction of this outcome and most of them reported evidences of obstructive pulmonary disorder (Andersen et al. 2011; Schikowski et al. 2005), although this topic is still controversial (Schikowski et al. 2014). A recently published study (ESCAPE), designed to evaluate the chronic effect of air pollution on pulmonary function, suggested an association between exposure to NO2 and PM10 but not to PM2.5, along with reduced FEV1 and FVC, mainly in obese individuals (Adam et al. 2015). 12 A longitudinal study carried out in Germany with women living near major roads detected a significant association between exposure to PM10 and reduction of FVC, FVE1 and of FEV1/FVC (Schikowski et al. 2005). A study carried out with 1391 nonsmokers followed up by 16 years (Abbey et al. 1998) detected a decrease of 7.2% in FEV1 among those with higher levels of exposure, as well as a significant decrease in FEV1/FVC. A similar obstructive effect on children exposed to traffic-generated pollutants was reported in a study realized in Munich (Wjst et al. 1993). While the effects of exposure to pollutants generated by burned biomass on lung function are better established (Eisner et al. 2010; Regalado et al. 2006), this does not seem to occur with the effects of exposure to urban pollutants. A detailed analysis (Health Effects Institute 2010) involving studies from different continents concludes that the evidence is still insufficient, even though it points out that chronic exposure suggests effects on adolescents and young people, similarly to that suggested by others authors (Kelly and Fussell 2011). A study conducted in the Netherlands, comparing transportation modes (bus, car, and bicycle), suggests that exposure to PM10 is associated with the reduction in PEF and increased resistance of airways. An association between exposure to soot and increase in FEF25-75% has also been reported (Zuurbier et al. 2011). In a statement on risk factors for Chronic Obstructive Pulmonary Diseases (Eisner et al. 2010) The American Thoracic Society considers that there are enough evidences to state that air pollution reduces lung function. The results of this study are in agreement with results from other studies (Kalappanavar et al. 2012; Kan et al. 2007) in the sense that air pollution is associated to a reductions in FVC and FEV1 without a reduction in FEV1/FVC, suggesting lung volume reduction 13 with restrictive ventilatory disorder, although a possible inflammatory effect of ozone cannot be ruled out (Goodman et al. 2014; Schelegle et al. 2007). Few studies also showed increased levels of FEF25-75%. Gupta et al. (2011) considered two groups of 100 non-smoking policemen, one of them consisting of traffic policemen and the other consisting of policemen who were never worked exposed to vehicular pollution, and suggested decreases in lung function as well as higher prevalence of respiratory symptoms in the exposed group. However, they did not use predicted values to compare the groups and did not show FEF25-75 and FEV1/FVC values, complicating a comparison with our results. The lower prevalence of asthma-suggestive respiratory symptoms in the high exposure group in our study is in agreement with the results of their lung function test that showed a restrictive functional pattern. We also detected a significant increase in FEF25-75% without a corresponding reduction in FEV1/FVC suggesting a restrictive disorder with probable increase in the elastic recoil. This can be attributed to a characteristic of fine particles which tend to deposit in the small airways causing wall inflammation, thickening, and remodelling, as suggested by studies using lungs from autopsies in São Paulo, Brazil (Saieg et al. 2011) and in Fresno County, California, USA (Pinkerton et al. 2000). A study carried out in India with 300 children living in an industrial area and 300 children living in a green zone estimated a prevalence of restrictive ventilatory disorders of 20,3% and 6,0%, respectively, supporting the hypothesis that exposure to air pollution may be associated with lung function impairment (Kalappanavar et al. 2012). These findings are also consistent with a study involving 230 children in Mexico city and 19 in the city of Tlaxcala; the authors detected 60% of interstitial markings in children of Mexico City in contrast with 0% in city of Tlaxcala, where the PM and ozone levels are lower(Calderon-Garciduenas et al. 2006). An interesting recently 14 published study, comparing pulmonary function of Indian and UK-Indian children suggests that children living in rural areas in India have lower values of FVC and FEV1, without reduction of FEV1/FVC, suggesting an association between nutritional and environmental effects and restrictive disorders, since exposure to biomass in rural areas of the country is usual (Sonnappa et al. 2015). In one of the few studies reporting values of FEF25-75% , a restrictive pattern of lung function disorder very similar to that observed in our study was observed in traffic controllers in India (Patil et al. 2013). However, in addition to the methodological problems of the study, this effect is still controversial given that a previous study conducted in India three years before, showed reductions in FVC and FEV1 among nonsmoking participants. When the analysis took only smokers of exposed and unexposed to traffic groups into account smaller values of FEF25-75% and maximum voluntary ventilation among the traffic exposed participants was observed, suggesting a mixed ventilatory disorder (Pal et al. 2010). It is already known that part of the people exposed to tobacco smoke develop interstitial lung disease (Morse and Rosas 2014; Vassallo and Ryu 2012), also limiting the interpretation of such results. Waking up with respiratory symptoms was more frequently present in participants classified in the medium and high exposed groups. Wheezing, asthma, nasal allergy were rare and similar among participants of the three groups. Low perception of respiratory symptoms has been far studied in literature, mainly in asthma patients. Lack of illness severity perception is associated to worse outcome and prognosis. Furthermore, the need for education and follow up by symptoms and signs monitoring by peak flow meter and lung function which present more sensibility and specificity (Kaptein et al. 2008; Koinis-Mitchell et al. 2009). We conjecture that asthma patients who may present severe clinical signs during exacerbations may have low perception of 15 their symptoms and it is plausible to assume that exposed individuals may also be less perceptive of respiratory symptoms due to small fluctuations of ambient air pollution. This hypothesis supports the need of more specific tools to check adverse effects on respiratory symptoms secondary to air pollutants. Although NOex is considered as a good and not invasive method to check for respiratory inflammation (Choi et al. 2006; Ricciardolo et al. 2004), in our study its levels were similar among groups independently of the pollutant exposure levels. This may be caused by the sensibility in detecting low levels of respiratory inflammation. Accordingly, another study conducted by our group suggested that air pollution was related to respiratory inflammation in street traffic controllers in São Paulo suggesting that NOex is a marker of airway inflammation and of decrease the pH of the exhaled condensate breath (Lima et al. 2013). Differently from this study, the authors compared indoor and outdoor workers measuring the NO in the condensate breath which may have improved the sensibility of their results. In conclusion, this study suggests that adult individuals chronically exposed to higher concentration of PM2.5 vehicular air pollution showed significant reductions in FVC, FEV1 and PEF, without a concomitant reduction of FEV1/FVC, as well as an increase of FEF25-75%, suggesting that the exposure to fine particles is associated, predominantly, with ventilatory restrictive impairment. 16 References Abbey DE, Burchette RJ, Knutsen SF, McDonnell WF, Lebowitz MD, Enright PL. 1998. Long-term particulate and other air pollutants and lung function in nonsmokers. Am J Respir Crit Care Med 158(1): 289-298. Adam M, Schikowski T, Carsin AE, Cai Y, Jacquemin B, Sanchez M, et al. 2015. Adult lung function and long-term air pollution exposure. ESCAPE: a multicentre cohort study and meta-analysis. Eur Respir J 45(1): 38-50. American Thoracic Society. 1999. Recommendations for standardized procedures for the on-line and off-line measurement of exhaled lower respiratory nitric oxide and nasal nitric oxide in adults and children-1999. This official statement of the American Thoracic Society was adopted by the ATS Board of Directors, July 1999. Am J Respir Crit Care Med 160(6): 2104-2117. American Thoracic Society Workshop. 2006. ATS Workshop Proceedings: Exhaled nitric oxide and nitric oxide oxidative metabolism in exhaled breath condensate: Executive summary. Am J Respir Crit Care Med 173(7): 811-813. Andersen ZJ, Hvidberg M, Jensen SS, Ketzel M, Loft S, Sorensen M, et al. 2011. Chronic obstructive pulmonary disease and long-term exposure to traffic-related air pollution: a cohort study. Am J Respir Crit Care Med 183(4): 455-461. Boogaard H, Fischer PH, Janssen NA, Kos GP, Weijers EP, Cassee FR, et al. 2013. Respiratory effects of a reduction in outdoor air pollution concentrations. Epidemiology 24(5): 753-761. Brunekreef B, Beelen R, Hoek G, Schouten L, Bausch-Goldbohm S, Fischer P, et al. 2009. Effects of long-term exposure to traffic-related air pollution on respiratory and cardiovascular mortality in the Netherlands: the NLCS-AIR study. Res Rep Health Eff Inst(139): 5-71; discussion 73-89. 17 Calderon-Garciduenas L, Mora-Tiscareno A, Fordham LA, Chung CJ, Valencia-Salazar G, Flores-Gomez S, et al. 2006. Lung radiology and pulmonary function of children chronically exposed to air pollution. Environ Health Perspect 114(9): 1432-1437. Choi J, Hoffman LA, Rodway GW, Sethi JM. 2006. Markers of lung disease in exhaled breath: nitric oxide. Biol Res Nurs 7(4): 241-255. Choudhary H, Tarlo SM. 2014. Airway effects of traffic-related air pollution on outdoor workers. Curr Opin Allergy Clin Immunol 14(2): 106-112. de Miranda RM, de Fatima Andrade M, Fornaro A, Astolfo R, de Andre PA, Saldiva P. 2012. Urban air pollution: a representative survey of PM(2.5) mass concentrations in six Brazilian cities. Air Qual Atmos Health 5(1): 63-77. Downs SH, Schindler C, Liu LJ, Keidel D, Bayer-Oglesby L, Brutsche MH, et al. 2007. Reduced exposure to PM10 and attenuated age-related decline in lung function. N Engl J Med 357(23): 2338-2347. Duarte AA, Pereira CA, Rodrigues SC. 2007. Validation of new brazilian predicted values for forced spirometry in caucasians and comparison with predicted values obtained using other reference equations. J Bras Pneumol 33(5): 527-535. Eisner MD, Anthonisen N, Coultas D, Kuenzli N, Perez-Padilla R, Postma D, et al. 2010. An official American Thoracic Society public policy statement: Novel risk factors and the global burden of chronic obstructive pulmonary disease. Am J Respir Crit Care Med 182(5): 693-718. European Community Respiratory Health Survey. 1996. Variations in the prevalence of respiratory symptoms, self-reported asthma attacks, and use of asthma medication in the European Community Respiratory Health Survey (ECRHS). Eur Respir J 9(4): 687-695. 18 Fisberg RM, Colucci AC, Morimoto JM, Marchioni DM. 2008. [Food frequency questionnaire for adults from a population-based study]. Rev Saude Publica 42(3): 550554. Gauderman WJ, Avol E, Gilliland F, Vora H, Thomas D, Berhane K, et al. 2004. The effect of air pollution on lung development from 10 to 18 years of age. N Engl J Med 351(11): 1057-1067. Gauderman WJ, Vora H, McConnell R, Berhane K, Gilliland F, Thomas D, et al. 2007. Effect of exposure to traffic on lung development from 10 to 18 years of age: a cohort study. Lancet 369(9561): 571-577. Goodman JE, Prueitt RL, Chandalia J, Sax SN. 2014. Evaluation of adverse human lung function effects in controlled ozone exposure studies. J Appl Toxicol 34(5): 516-524. Götschi T, Heinrich J, Sunyer J, Kunzli N. 2008. Long-term effects of ambient air pollution on lung function: a review. Epidemiology 19(5): 690-701. Gupta S, Mittal S, Kumar A, Singh KD. 2011. Respiratory effects of air pollutants among nonsmoking traffic policemen of Patiala, India. Lung India 28(4): 253-257. Health Effects Institute. 2010. Traffic-Related Air Pollution: A Critical Review of the Literature on Emissions, Exposure, and Health Effects. HEI special Report 17. Boston, MA. Kalappanavar NK, Vinodkumar CS, Gouli C, Sanjay D, Nagendra K, Basavarajappa KG, et al. 2012. Carbon particles in airway macrophage as a surrogate marker in the early detection of lung diseases. Int J Occup Environ Med 3(2): 68-75. Kan H, Heiss G, Rose KM, Whitsel E, Lurmann F, London SJ. 2007. Traffic exposure and lung function in adults: the Atherosclerosis Risk in Communities study. Thorax 62(10): 873-879. 19 Kaptein AA, Hughes BM, Scharloo M, Fischer MJ, Snoei L, Weinman J, et al. 2008. Illness perceptions about asthma are determinants of outcome. J Asthma 45(6): 459464. Kelly FJ, Fussell JC. 2011. Air pollution and airway disease. Clin Exp Allergy 41(8): 1059-1071. Kjaergaard SK, Pedersen OF, Miller MR, Rasmussen TR, Hansen JC, Molhave L. 2004. Ozone exposure decreases the effect of a deep inhalation on forced expiratory flow in normal subjects. J Appl Physiol (1985) 96(5): 1651-1657. Koinis-Mitchell D, McQuaid EL, Seifer R, Kopel SJ, Nassau JH, Klein RB, et al. 2009. Symptom perception in children with asthma: cognitive and psychological factors. Health Psychol 28(2): 226-237. Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. 2012. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet 380(9859): 2224-2260. Lima TM, Kazama CM, Koczulla AR, Hiemstra PS, Macchione M, Fernandes AL, et al. 2013. pH in exhaled breath condensate and nasal lavage as a biomarker of air pollution-related inflammation in street traffic-controllers and office-workers. Clinics (Sao Paulo) 68(12): 1488-1494. McConnell R, Berhane K, Yao L, Jerrett M, Lurmann F, Gilliland F, et al. 2006. Traffic, susceptibility, and childhood asthma. Environ Health Perspect 114(5): 766-772. Miller MR, Crapo R, Hankinson J, Brusasco V, Burgos F, Casaburi R, et al. 2005a. General considerations for lung function testing. Eur Respir J 26(1): 153-161. Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. 2005b. Standardisation of spirometry. Eur Respir J 26(2): 319-338. 20 Morse D, Rosas IO. 2014. Tobacco smoke-induced lung fibrosis and emphysema. Annu Rev Physiol 76: 493-513. Pal P, John RA, Dutta TK, Pal GK. 2010. Pulmonary function test in traffic police personnel in Pondicherry. Indian J Physiol Pharmacol 54(4): 329-336. Patil PJ, Thakare GV, Patil SP. 2013. Comparative study of lung function test of policemen in traffic control with those in general duty. Physiol Pharm Pharmacol 3: 162-166. Pellegrino R, Viegi G, Brusasco V, Crapo RO, Burgos F, Casaburi R, et al. 2005. Interpretative strategies for lung function tests. Eur Respir J 26(5): 948-968. Pereira CA, Sato T, Rodrigues SC. 2007. New reference values for forced spirometry in white adults in Brazil. J Bras Pneumol 33(4): 397-406. Pinkerton KE, Green FH, Saiki C, Vallyathan V, Plopper CG, Gopal V, et al. 2000. Distribution of particulate matter and tissue remodeling in the human lung. Environ Health Perspect 108(11): 1063-1069. R Development Core Team. 2013. R: A language and environment for statistical computing. Regalado J, Perez-Padilla R, Sansores R, Paramo Ramirez JI, Brauer M, Pare P, et al. 2006. The effect of biomass burning on respiratory symptoms and lung function in rural Mexican women. Am J Respir Crit Care Med 174(8): 901-905. Ribeiro M, Angelini L, Robles-Ribeiro PG, Stelmach R, Santos Ude P, Terra-Filho M. 2007. Validation of the Brazilian-Portuguese version of the European Community Respiratory Health Survey in asthma patients. J Asthma 44(5): 371-375. Ricciardolo FL, Sterk PJ, Gaston B, Folkerts G. 2004. Nitric oxide in health and disease of the respiratory system. Physiol Rev 84(3): 731-765. 21 Rice MB, Ljungman PL, Wilker EH, Gold DR, Schwartz JD, Koutrakis P, et al. 2013. Short-term exposure to air pollution and lung function in the Framingham Heart Study. Am J Respir Crit Care Med 188(11): 1351-1357. Romieu I, Gouveia N, Cifuentes LA, de Leon AP, Junger W, Vera J, et al. 2012. Multicity study of air pollution and mortality in Latin America (the ESCALA study). Res Rep Health Eff Inst(171): 5-86. Saieg MA, Cury PM, Godleski JJ, Stearns R, Duarte LG, D'Agostino L, et al. 2011. Differential elemental distribution of retained particles along the respiratory tract. Inhal Toxicol 23(8): 459-467. Sava F, Carlsten C. 2012. Respiratory health effects of ambient air pollution: an update. Clin Chest Med 33(4): 759-769. Schelegle ES, Walby WF, Adams WC. 2007. Time course of ozone-induced changes in breathing pattern in healthy exercising humans. J Appl Physiol (1985) 102(2): 688-697. Schikowski T, Mills IC, Anderson HR, Cohen A, Hansell A, Kauffmann F, et al. 2014. Ambient air pollution: a cause of COPD? Eur Respir J 43(1): 250-263. Schikowski T, Sugiri D, Ranft U, Gehring U, Heinrich J, Wichmann HE, et al. 2005. Long-term air pollution exposure and living close to busy roads are associated with COPD in women. Respir Res 6: 152. Sonnappa S, Lum S, Kirkby J, Bonner R, Wade A, Subramanya V, et al. 2015. Disparities in Pulmonary Function in Healthy Children across the Indian Urban-Rural Continuum. Am J Respir Crit Care Med 191(1): 79-86. Strak M, Janssen NA, Godri KJ, Gosens I, Mudway IS, Cassee FR, et al. 2012. Respiratory health effects of airborne particulate matter: the role of particle size, composition, and oxidative potential-the RAPTES project. Environ Health Perspect 120(8): 1183-1189. 22 Vassallo R, Ryu JH. 2012. Smoking-related interstitial lung diseases. Clin Chest Med 33(1): 165-178. Wjst M, Reitmeir P, Dold S, Wulff A, Nicolai T, von Loeffelholz-Colberg EF, et al. 1993. Road traffic and adverse effects on respiratory health in children. BMJ 307(6904): 596-600. World Health Organization. 1989. Measuring obesity: classification and description of anthropometric data. WHO (Nutr UD, EUR./ICP/NUT 125). Copenhagen. World Health Organization. 2006. WHO Air quality guidelines for particulate matter, ozone, nitrogen dioxide and sulfur dioxide. Copenhagen: World health Organization Regional Office for Europe. World Health Organization. 2014. Mortality from ambient air pollution.http://www.who.int/gho/phe/outdoor_air_pollution/burden_text/en/ [accessed 2014]. Yohai VJ. 1987. High Breakdown-Point and High Efficiency Robust Estimates for Regression. Ann Statist 15(2): 642-656. Zuurbier M, Hoek G, Oldenwening M, Meliefste K, van den Hazel P, Brunekreef B. 2011. Respiratory effects of commuters' exposure to air pollution in traffic. Epidemiology 22(2): 219-227. 23 TABLE 1. Baseline characteristics of participants according to exposure groups (N= 101) Variables Age (years) BMI (kg/m2) Waist circumference (cm) Time of work (years) Work shift (hours) Exhaled Carbon Monoxide (ppm) ETS(2) (N (%)) at home (N(%)) at work (N(%)) Hypertension and/or diabetes (N (%)) Haemoglobin (g/dL) Haematocrit (%) White blood cells (N/mm3) Total Colesterol (mg/dL) HDL LDL Albumin (g/dL) Fasting blood glucose (mg/dL) Exposure groups Medium Low (N=15) (N=76) 46.6 (±8.4) 48.4 (±9.0) 26.4 (±3.7) 28.9 (±4.4) 94.9 (±8.8) 102.5 (±12.7) 16.5 (±7.8) 10.3 (±8.2) 9.3 (±2.4) 11.3 (±3.5) 2.5 (±2.9) 2.6 (±3.1) 7 (46.7) 39 (51,3) 1 (6.7) 5 (6.6) 6 (40.0) 41 (54.0) High (N=10) 49.3 (±12.4) 28.4 (±3.7) 101.3 (±10.4) 11.9 (±11.4) 12.6 (±3.5) 1.5 (±2.0) 4 (40.0) 2 (20.0) 5 (50.0) p 0.730 (1) 0.117 (1) 0.098 (1) 0.041 (1) 0.040 (1) 0.525 (1) 0.775 (3) 0.430 (4) 0.610 (4) 5 (33.3%) 24 (31.6%) 3 (30.0%) 0.984 (4) 15.3 (±0.9) 44.4 (±2.9) 6217 (±1685) 200.1 (±39.6) 47.4 (±8.3) 130.3 (±37.6) 4.7 (±0.2) 96.0 (±9.7) 15.1 (±0.9) 44.7 (±2.4) 6765 (±1634) 212.1 (±34.2) 46.2 (±12.7) 136.5 (±31.6) 4.7 (±0.2) 101.4 (±23.4) 14.8 (±0.6) 43.9 (±1.3) 7052 (±2539) 201.8 (±34.9) 42.9 (±8.3) 132.8 (±32.2) 4.8 (±0.3) 106.3 (±21.7) 0.463 (1) 0.587 (1) 0.469 (1) 0.384 (1) 0.662 (1) 0.774 (1) 0.623 (1) 0.510 (1) Intake of fruits and vegetables (portions)(5) 5.7 (±3.6) 6.3 (±3.1) 5.7 (±3.3) ANOVA ; (2) Enviromental Tobaco Smoke; (3) Chi-Squared test; (4) LikelihoodRatio test; (5) Low: N=8, Medium: N=68, High: N=8. Results expressed as mean (± standard deviation) or number (percentage). 24 0.774 (1) TABLE 2. Prevalence of respiratory symptoms and median (interquartile range) of exhaled nitric oxide (NOex) and spirometric parameters of participants according to exposure groups (N=101) Exposure groups Medium Low (N=15) (N=76) Respiratory Symptoms Q1. Wheeze Q1.1.Wheeze with breathless Q1.2. Wheeze without a cold Q2. Waking with tightness in the chest Q3. Waking with breathless Q4. Waking with cough Q5. Attack of asthma Q6. Treatment for asthma Q7. Nasal allergy Q5 or Q6 - Asthma diagnose High (N=10) p 2 (13.3%) 1 (6.7%) 0 (0.0%) 12 (15.8%) 7 (9.2%) 10 (13.2%) 1 (10.0%) 0.867 (1) 1 (10.0%) 0.940 (1) 1 (10. 0%) 0.146 (1) 0 (0.0%) 0 (0.0%) 0 (0.0%) 0 (0.0%) 0 (0.0%) 2 (13.3%) 0 (0.0%) 12 (15.8%) 11 (14.5%) 17 (22.4%) 3 (4.0%) 2 (2.6%) 21 (27.6%) 5 (6.6%) 4 (40.0%) 0 (0.0%) 0 (0.0%) 1 (10.0%) 0 (0.0%) 3 (30.0%) 1 (10.0%) NOex 19.5 (15.7) 20.7 (10.5) 22.1 (10.1) 0.845 (3) Lung function parameters FVC (%) (2) FEV1 (%) (2) FEV1/FVC (%) 94.0 (13.0) 91.5 (11.3) 77.5 (10.9) 0.014 (1) 0.035 (1) 0.005 (1) 0.388 (1) 0.562 (1) 0.445 (1) 0.343 (1) 83.5 (17.2) 0.076 (3) 82.2 (19.2) 0.143 (3) 80.3 (6.8) 0.997 (3) 120.2 (2) FEF25-75/FVC (%) 102.5 (17.1) 104.8 (18.3) (22.5) 0.041 (3) PEF (%) (2) 79.9 (30.0) 74.9 (18.5) 72.6 (26.7) 0.386 (3) (1) Likelihood- Ratio test; (2) Percentage of predict value; (3) Kruskal-Wallis test. 94.9 (16.4) 91.2 (13.8) 79.6 (7.3) 25 Table 3. Effects of PM2.5 on lung function in different stages of the regression model fitting: high exposure – low exposure and medium exposure – low exposure Model 1 Model 2 Model 3 Model 4 Exposure groups compared Medium -Low High - Low effect -0.13 -12.96 std error 2.71 3.88 FEV1 (%)(1) Medium -Low High - Low 0.94 -10.12 3.35 5.03 0.780 0.047 1.77 -9.36 3.47 4.52 0.611 1.76 0.041 -8.41 3.50 5.04 0.617 0.099 1.16 -9.10 3.33 5.10 0.729 0.078 FEV/FVC (%) Medium -Low High - Low 1.51 1.42 2.39 2.51 0.529 0.573 1.76 1.46 3.02 3.09 0.561 0.638 1.86 1.97 3.29 3.28 0.572 0.550 1.96 1.97 3.31 3.35 0.557 0.558 Medium -Low High - Low 1.74 18.43 3.09 5.78 0.574 0.002 -0.83 15.57 3.66 5.93 0.821 -0.80 0.010 14.99 3.79 5.93 0.833 -0.91 0.013 14.86 3.86 6.08 0.814 0.017 FVC (%)(1) FEF25-75/FVC (%)(1) PEF (%)(1) p effect 0.960 1.01 0.001 -11.01 std error p effect std error p effect std error p 2.97 0.730 0.81 3.18 0.800 -0.24 3.01 0.938 3.98 0.007 -10.76 4.09 0.010 -12.19 3.98 0.003 Medium -Low -4.45 5.53 0.423 -1.48 5.77 0.799 -1.76 5.82 0.763 -1.84 5.66 0.746 High - Low -6.87 7.34 0.351 -3.58 7.43 0.631 -4.34 7.99 0.588 -4.41 7.97 0.581 (1) Percentage of predict value Predictors included in the models Model 1: Exposure groups Model 2: Exposure groups + age + waist circumference + time of work + work shift Model 3: Exposure groups + age + waist circumference + time of work + work shift + ETS at home + former smoker Model 4: Exposure groups + age + waist circumference + time of work + work shift + ETS at home + former smoker + DM or HAS 26 Figure 1. Distribution of individual personal PM2.5 measurements during the study period in the group of traffic controllers and taxi drivers, and in the group of forest workers 27