Induction for GP locums—how to get it right Authors
advertisement
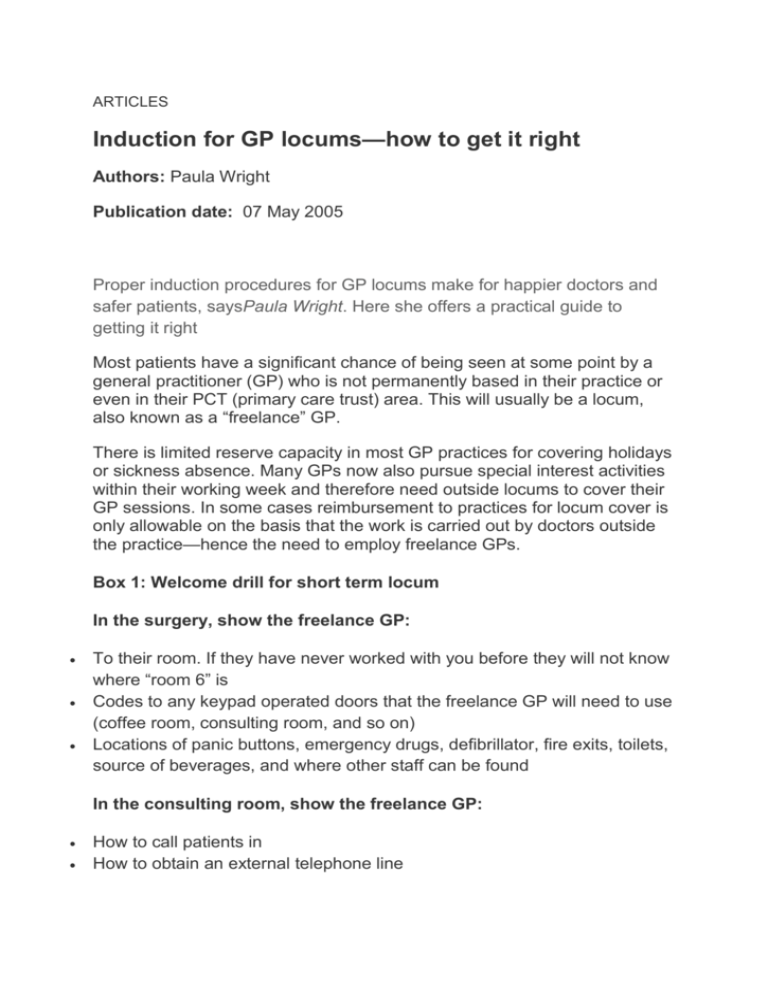
ARTICLES Induction for GP locums—how to get it right Authors: Paula Wright Publication date: 07 May 2005 Proper induction procedures for GP locums make for happier doctors and safer patients, saysPaula Wright. Here she offers a practical guide to getting it right Most patients have a significant chance of being seen at some point by a general practitioner (GP) who is not permanently based in their practice or even in their PCT (primary care trust) area. This will usually be a locum, also known as a “freelance” GP. There is limited reserve capacity in most GP practices for covering holidays or sickness absence. Many GPs now also pursue special interest activities within their working week and therefore need outside locums to cover their GP sessions. In some cases reimbursement to practices for locum cover is only allowable on the basis that the work is carried out by doctors outside the practice—hence the need to employ freelance GPs. Box 1: Welcome drill for short term locum In the surgery, show the freelance GP: To their room. If they have never worked with you before they will not know where “room 6” is Codes to any keypad operated doors that the freelance GP will need to use (coffee room, consulting room, and so on) Locations of panic buttons, emergency drugs, defibrillator, fire exits, toilets, source of beverages, and where other staff can be found In the consulting room, show the freelance GP: How to call patients in How to obtain an external telephone line How to log in to the computer (Windows and clinical system) and how to find the surgeries The practice directory of phone numbers (reception, secretary, consulting rooms, nurses and so on) How to use the practice intranet How to print a prescription (is there a “dummy”/“play” patient to test printer is correctly loaded?) Any non-phone messaging system that may be used within the practice, for example, internal practice email, especially where this is routinely used for communication between doctors and admin staff during surgeries. In the consulting room, show the freelance GP where to find: Stationery—sick notes, FP10 pad and computer script supplies, letterhead, envelopes, blood forms, x ray forms, etc. Referral forms (ideally in a file) Maps of any new estates that are not included in the commercially available A to Z (partners will often have local council maps of these) Essential equipment such as blood pressure machine, peak flow meter, speculums, gloves, swabs, MSU bottles Dictaphone and tape Different practices Practices vary widely in their approaches to handling workload and access, use of IT systems, team working, chronic disease management, and so on; they therefore need to have some means of helping freelance GPs to become rapidly acquainted with their systems. Patients are quickly unsettled by a consultation where a competent GP is struggling to find essential items of equipment or forms, or lacks important information about local services. Preventing mistakes Many adverse events involving patients are thought to be down to a combination of unsafe acts (“active failures”) and unsafe systems (“latent conditions”). [1] NHS inquiries into adverse events have consistently recommended that action is needed in communication (between individuals, departments, and organisations) and in staff training. Locum induction procedures and information fall under both of these categories. A robust induction for freelance GPs is a vital starting point for preventing adverse events. What is a good induction? There are two key elements to a good induction: A welcome drill An induction folder Induction Ideally, a GP registrar, salaried doctor, or long term locum should receive protected paid time for induction (ranging from two sessions to one week, depending on their needs). This is an essential investment that any practice must make to maintain standards and should be a part of any contractual arrangement for these doctors. Short term locums When the term of the locum is short (ie a few days), it is not cost effective either for practices or for freelance GPs to finance the amount of time mentioned above so it is crucial that induction systems are in place that can be administered efficiently and reliably. When first working in a new practice most freelance GPs usually plan to arrive 10-15 minutes before starting work in order to brief themselves and check that their room is adequately stocked. The practice should value this bonus unpaid time offered by the freelance GP by ensuring that there is always a member of staff free at this time to provide a short induction. This may be a time when surgery doors are still locked and phones are “off”, so managers should ensure freelance GPs are given a contact “bypass” phone number so they can get into the system when they arrive. This is also relevant where surgeries close at lunchtime. Welcome drill Sometimes there is one member of staff who is charged with welcoming the freelance GP, but a clear checklist should be available for other staff members to follow when this person is away. This checklist should be reviewed periodically with input from GPs and practice manager. (See box 1 for drill aimed at a short term locum.) Saying something like, “If you need anything just ask” should not be a lazy replacement for actually checking the room with the freelance GP until they are satisfied that they have everything they need to work. It will be inefficient and irritating to the staff, freelance GPs, and patients to have a surgery punctuated by phone call requests for missing items, which could clearly have been foreseen to be required at the outset. This will also help surgeries run to time. The locum induction file This file provides essential information about how the practice works, what services are available and how different team members refer to each other (see box 2). The National Association of Sessional GPs (www.nasgp.org.uk/) has a model induction folder which can be completed by each practice, and there is also a “Locum Welcome” template document on the website for the North-East Employed and Locum GP group (www.nelg.org.uk) developed by the author. Exemplary practices will already have a comprehensive file with all internal protocols, referral and other information, and may not even need to prepare such a folder for new doctors. Whatever the original purpose of the folder it needs to be properly indexed so items can be found easily and regularly updated. For practices with more sophisticated IT systems, standard forms and protocols may be found on the practice or PCT intranet and may be demonstrated to the freelance GP as part of the welcome drill, thus obviating the need for maintaining photocopied stocks of forms in all doctors' rooms and the induction folder. Conclusion As well as ensuring a consistent level of service, proper induction makes being at work a more satisfying experience, and indeed the two are linked. Freelance GPs soon learn to avoid badly organised practices that do not support them. Practices have much to gain from routinely asking freelance GPs for feedback about their experience working there. In this way they can be alerted to problems that give rise to risk before adverse events occur. Box 2: Items to include in the induction folder Telephone numbers: internal extensions and external numbers (for example, social worker, child protection, Macmillan nurses, etc) Referral forms and guidelines relating to local services including fast track services How to organise investigations (routine and urgent): Within the practice—Are there specific forms to complete, or are they just requested by patients at reception? Is an appointment needed or are they done on spec by nurses? Bloods, ECG, pregnancy test, paeds, urines, spirometry Outside the practice—Are forms required? Is there a walk-in service, or is an appointment needed? X rays, USS, pregnancy scans, cardiac echo, echo, carotid, etc. How are different services accessed (book in reception, dictate letter, or form) and are they available within the practice (for example, counselling, IUDs, depo contraception, implants, minor surgery, smoking cessation, midwife, chiropody, physiotherapy, district nurse, health visitors)? How are laboratory and other results actioned or labelled for action—electronically or on paper? Are EMIS “practice notes” used? How are new drugs or diagnoses in hospital letters incorporated into records? Information about local community or hospital services that are innovative and peculiar to the area—direct booking of hospital appointments by patient, “falls” clinic, headache clinic, psychosexual clinic. Information on how patients are added to disease registers and around use of READ coding with respect to the new general medical service contract. Practice procedures/protocols: Repeat prescribing protocol Appointments (does the practice have “advanced access” and if so how are follow ups arranged?) Internal messaging, etc Who to report adverse or significant events to Referral letters—is there a practice log for these to ensure they are not missed and how are they prioritised? There are now a number of quality frameworks that can influence the adoption of induction procedures by practices. Interestingly, the quality team development framework of the Royal College of General Practitioners (www.rcgp.org.uk/), and the new general medical services' (nGMS) quality and outcomes framework, for example, do not include locum induction as a standard. In what has become a “points mean prizes” world, induction files and procedures will not be taken seriously until they become a requirement under the nGMS quality and outcomes framework. ■ References 1. Department of Health. An organisation with a memory. Report of an expert group on learning from adverse events in the NHS. London: The Stationery Office, 2000.http://www.dh.gov.uk/assetRoot/04/06/50/86/04065086.pdf (acc essed 29 Oct 2004). Paula Wright portfolio freelance general practitioner Newcastle upon Tyne pfwright@doctors.org.uk Cite this as BMJ Careers ; doi: