specialised rheumatology services (all ages)
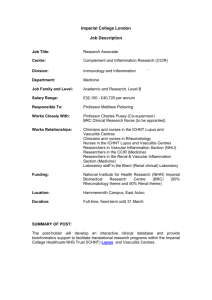
advertisement

Council3/Agenda Item 8/ii 2nd Mailing Dear Colleagues As part of the work we are doing with the National Commissioning Board we have been asked to identify units around Engalnd who provide an informal service where rheumatologists refer to other rheumatologists because of their recognised expertise in an area. We are hoping to bolster many of these services by recognition and support from the National Commissioning Board, and the development of clinical networks with specailist centres acting as hubs, and other centres as spokes. Much of the detail has yet to be negotiated. I would be grateful if you would check the provisional list at the end off the attached document for any services we have missed out in terms of adult rheumatology, either for rare genetic disorders, or for rare or severe manifestations of autoimmune rheumatic diseases. Would you please check this list for any centres we have missed out. I need this information by the 12th of October. I will be happy to take any questions on this at Council next week. 2nd Mailing Council3/Agenda Item 8/ii SPECIALISED RHEUMATOLOGY SERVICES (ALL AGES) INTERIM SCOPE Description of Service Rheumatology is a multidisciplinary branch of medicine that deals with the investigation, diagnosis and management of patients with arthritis and other musculoskeletal conditions. This incorporates over 200 disorders affecting joints, bones, muscles and soft tissues, including inflammatory arthritis and other systemic autoimmune disorders, vasculitis, soft tissue conditions, spinal pain and metabolic bone disease. A significant number of musculoskeletal conditions also affect other organ systems. In recent years it has been noted that chronic inflammatory conditions associate with increased cardiovascular morbidity mortality. Rheumatological conditions affect all age groups. Colleagues in paediatric rheumatology have worked separately on a scope that will include transitional care (adolescents moving from paediatric to adult services). Their conclusions are endorsed by the Specialised Rheumatology Services Group, and are not repeated here. The vast majority of rheumatology services will be commissioned through Clinical Commissioning Groups. However, there are three specialized areas of Rheumatology Practice that this scope defines where commissioning of specialist services directly through the National Commissioning Board offers an opportunity for 1. enhanced efficiency and effectiveness 2. High-quality patient experience and improved outcomes 3. The development of internationally competitive world-class centres of excellence in specialized clinical practice and research. These three specialised areas of specialised rheumatology are: 1. Paediatric and transitional care rheumatology 2. Inherited disorders of connective tissue 3. Autoimmune rheumatic disease and vasculitis. Existing models of specialized commissioning within these areas include the complex Ehlers-Danlos Syndrome (EDS) service and the Behcet’s syndrome Centres of Excellence (1). There are currently a number of nationally recognised centres of excellence in rheumatology that have informally operated as tertiary referral centres. These currently operate on an ad hoc and underresourced basis and National Commissioning will support the development of formal service specifications and policies that guide referrals to these centres (e.g. see the Behçet’s syndrome documentation (1). See also the attached document on “Improving NHS services for rare autoimmune disorders”, a review by an independent expert clinical group on rare autoimmune disorders that proposes the development of clinical networks, giving a useful vision of the nature of the specialist hub (2)). There are no diagnostic or coded procedures that are specific to specialised care for autoimmune disease and vasculitis. There are national specialist society guidelines and international guidelines on the management of most rheumatological conditions, but they do not help to differentiate between routine and specialist care. Most rheumatology activity (including specialised rheumatology) is conducted in out-patients, so that day case or in-patient activities do not help to differentiate between routine and specialised care. There are NICE technology appraisals on a variety of conventional and biological drugs used in common conditions in rheumatology, such as rheumatoid arthritis, psoriatic arthritis and ankylosing spondylitis, and Centres of Excellence will facilitate the optimal use of these and other novel therapies in the diseases that they specialise in. The reasons for referral from a general to a specialist rheumatologist might be around diagnosis, which is often not straight forward, and management particularly of rare and / or severe manifestations that have failed to respond to conventional approaches Specialised centres are characterised by (1,2): recognised experts in their field, who regularly receive referrals from other rheumatology consultant colleagues, and treat high volumes of patients with rare or severe disorders, ensuring a sufficient level of specialism to deliver the best outcomes. multidisciplinary teams who can ensure that the patient’s care is not limited by the expertise available to them (consisting of specialised consultant rheumatologist, specialist nurse, rehabilitation therapist, physiotherapist, occupational therapist, dentist / orthodontist, Council3/Agenda Item 8/ii 2nd Mailing pharmacist, dietician, ophthalmologist, clinical psychologist / psychiatrist, podiatrist and orthotist). having protocols in place for rapid access for new and existing patients with structured referral pathways developed shared care guidelines and arrangements with referring services, ensuring support is delivered as close to the patients’ home as possible, but access to specialist expertise is maintained taking steps to audit their outcomes and share these data with colleagues in other centres, enabling the spread of good practice and appropriate benchmarking of quality, with robust clinical governance processes facilitating participation in clinical trials and research training and continuing professional development to support and up-skill local non specialist teams patient involvement in the development and evaluation of networks and access to information to facilitate informed decisions and partnership in decision making Although musculoskeletal disease services focus, naturally, on disease affecting joints, muscles and bones, many forms of 'arthritis' involve many organs and systems. Thus the specialist rheumatology teams also work closely with other specialties (often involving joint clinics) including: · orthopaedics (including liaison with the skeletal dysplasia network and metabolic bone disease specialists) · nephrology (including access to renal biopsy services) · dermatology · ophthalmology (for uveitis and other inflammatory eye diseases) · cardiology (including assessment of pulmonary hypertension. There are 7 nationally commissioned centres. 30% of pulmonary hypertension is associated with autoimmune rheumatic disease) · respiratory medicine (including comprehensive lung function testing) · ear, nose and throat (for assessment of upper airways for granulomatous and other inflammatory disease) · dentistry (for xerostomia and ulceration) · psychology / psychiatry. · gastroenterology They also have access to a panoply of tests to assist diagnosis and prognosis, including radiology (xrays, ultrasound, CT scans, MRI scans, PET scans, radioisotope scans, angiography, and other specialised procedures), appropriate biopsies and specialised pathology services, and genetic diagnostic services. Specialised rheumatology services come under the three main headings listed above: 1. Paediatric and transitional care rheumatology Note: Our colleagues in paediatric rheumatology have worked separately on a scope that will include transitional care (adolescents moving from paediatric to adult services). Their conclusions are endorsed by our group. We do not feel strongly whether paediatric rheumatology is included in our “All ages” group, or under Paediatric Medicine. We feel that Paediatric Rheumatology lends itself very favourably to funding from the NCB, ticking all the appropriate boxes. Transitional care is a much neglected area of the interface between paediatric and adult rheumatology, and if we have separate adult and paediatric scopes we feel that transitional rheumatology needs to be reflected in both. 2. Inherited disorders of connective tissue These very rare disorders, often developing in children or young adults, are not seen sufficiently commonly by individual hospital units for local expertise to develop. They require multidisciplinary input including genetics and the establishment of centres in England that would provide a more focused, rational delivery of co-ordinated clinical care for long-term follow-up of these chronic disorders. These diseases include Ehlers Danlos (excluding type III) which is already nationally commissioned, Marfans syndrome, skeletal and other dysplasias, osteogenesis imperfecta, Council3/Agenda Item 8/ii 2nd Mailing dysostoses, fibrous dysplasia, osteopetroses, and osteosclerosis. These conditions will link with other Group 3 services including; Assessment and provision of equipment for people with complex physical disability (all ages) Specialised rehabilitation services for both brain injury and complex disability (adults) Specialised paediatric orthopaedic surgery services Specialised orthopaedic services (adults) However, because they are often inherited diseases and can affect any connective tissue, interactions with genetic services, cardiology and ophthalmology will also be undertaken as appropriate. 3. Autoimmune rheumatic disease and vasculitis Autoimmune rheumatic diseases and vasculitis cover a spectrum of disease severity ranging from mild and self-limiting disease to severe, handicapping, or life-threatening manifestations. As detailed above, many of these patients will be looked after by general rheumatologists, either independently or as part of a hub and spoke model with the specialist centres of excellence to drive high-quality care and research into these rare conditions. Our proposed method to identify and capture the specialised elements of these diseases and conditions is by using consultant to consultant referrals where: 1. The referring and receiving consultants are both Rheumatologists 2. The receiving hospital is on the list below, and 3. The referring and receiving hospitals are different The diseases are: Autoimmune rheumatic disorders Systemic lupus erythematosus (SLE) Antiphospholipid syndrome (APL) Systemic sclerosis Sjogrens syndrome Inflammatory muscle disease (myositis) Overlap syndromes Relapsing polychondritis Myositis/ inflammatory muscle disease Vasculitides, including: Giant cell arteritis (and polymyalgia rheumatica) Rheumatoid vasculitis Wegener’s granulomatosis Polyarteritis nodosa and micropolyarteritis Churg Strauss vasculitis Behcet’s disease (already accepted for specialist commissioning) Takayasu’s arteritis Henoch Schonlein purpura Cryoglobulinaemia Other rare inflammatory disorders Eosinophilic fasciitis Familial Mediterranean fever and other periodic syndromes Relapsing polychondritis Identifying activity for autoimmune rheumatic diseases and vasculitis Specialist Activity in recognised centres would be identified as follows: Within the Specialist centre: Council3/Agenda Item 8/ii 2nd Mailing Audits of all referrals from other consultant rheumatologists (diagnosis, reason for referral) In patient / outpatient / day case - all activity involving specialist MDT Interventions performed by the team that could identify specialist activity, e.g. use of unlicensed or novel therapies, intravenous immunoglobulin, plasma exchange Recruitment to condition-specific clinical and research databases A Preliminary list of specialist centres for autoimmune rheumatic diseases and vasculitis London UCLH (SLE & APS, myositis, Sjogren’s, vasculitis) London RFH (scleroderma) London Barts & RLH (Sjogren’s, Behcet’s) London UMDS Kings (myositis) London Guys & St Thomas’s (SLE & APS, Sjogren’s) London Kings College Hospital (myositis) Oxford (vasculitis, myositis) Cambridge (vasculitis & Sjogren’s) Bath & Bristol (scleroderma, SLE & APS) Southampton (SLE & APS) Birmingham (SLE & APS, Sjogren’s, vasculitis, Behcets, myositis) Leeds (SLE & APS, Sjogren’s, vasculitis, scleroderma, Behcets) Liverpool (Behcets, SLE & APS, Sjogren’s) Sheffield (Sjogren’s, SLE & APS) Manchester (scleroderma, SLE & APS, myositis) Newcastle (Sjogren’s, SLE & APS) Nottingham/Derby/Mansfield (SLE & APS, Sjogren’s, vasculitis) Ipswich & Norwich (vasculitis) Swindon (Sjogren’s) London Imperial (Behcet’s, vasculitis, SLE & APS) Southend (vasculitis, Sjogren’s) Blackburn (SLE & APS) These conditions have well established patient support groups actively championing greater awareness and research into these conditions: Council3/Agenda Item 8/ii 2nd Mailing www.lupusuk.org.uk/ www.hughes-syndrome.org/ www.raynauds.org.uk/ www.sclerodermasociety.co.uk www.bssa.uk.net/ www.myositis.org.uk/ www.behcets.org.uk www.vasculitis-uk.org Provisional costings: This would need to be formally costed but based on the assumption of an additional 1-2 consultant posts/centre, clinical nurse and administrative support = circa £350K/centre/year = £7 million/year = £35 million/5 years References 1. Behçet’s syndrome society. National commissioning and designation for Behçet’s syndrome centres of excellence. 2012 2. Improving NHS services for rare autoimmune diseases. A review by the independent expert clinical group on rare autoimmune diseases. October 2011.