Dining and Dementia - Common Sense Caregiving
advertisement
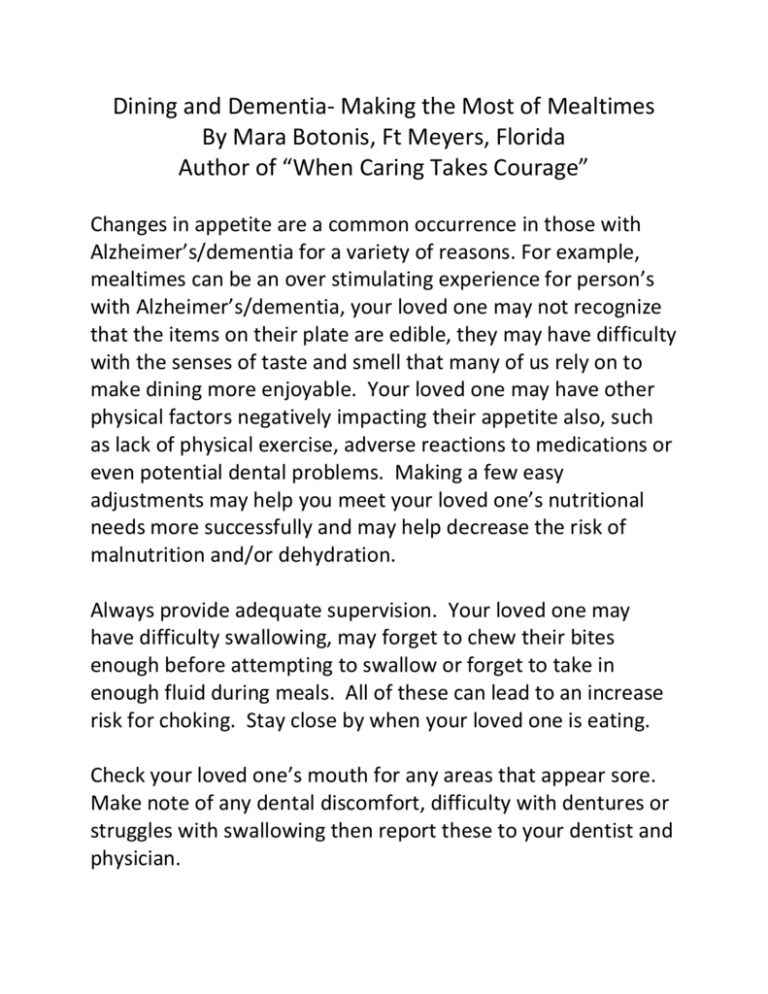
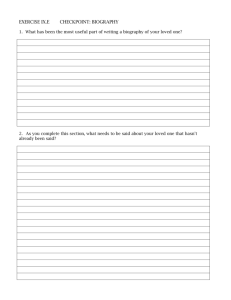
Dining and Dementia- Making the Most of Mealtimes By Mara Botonis, Ft Meyers, Florida Author of “When Caring Takes Courage” Changes in appetite are a common occurrence in those with Alzheimer’s/dementia for a variety of reasons. For example, mealtimes can be an over stimulating experience for person’s with Alzheimer’s/dementia, your loved one may not recognize that the items on their plate are edible, they may have difficulty with the senses of taste and smell that many of us rely on to make dining more enjoyable. Your loved one may have other physical factors negatively impacting their appetite also, such as lack of physical exercise, adverse reactions to medications or even potential dental problems. Making a few easy adjustments may help you meet your loved one’s nutritional needs more successfully and may help decrease the risk of malnutrition and/or dehydration. Always provide adequate supervision. Your loved one may have difficulty swallowing, may forget to chew their bites enough before attempting to swallow or forget to take in enough fluid during meals. All of these can lead to an increase risk for choking. Stay close by when your loved one is eating. Check your loved one’s mouth for any areas that appear sore. Make note of any dental discomfort, difficulty with dentures or struggles with swallowing then report these to your dentist and physician. Contact your loved one’s primary care physician and let them know about their decreased appetite. Be sure to have ready a list of all current medication and any vitamin supplements that your loved one is taking for the doctor to review. Track intake and changes in weight and/or appetite weekly if you suspect significant changes in weight. Communicate any weight changes of over 5 pounds per month to your family physician. Don’t ask your loved one if they are hungry. They may not remember when the last time was that they ate, that the stomachache they are feeling is actually hunger or that their dry mouth indicates thirst. Simply serve your loved one a small portion of favorite foods and beverages several times throughout the day. Work to pack as much nutrition as possible into the foods that your loved one is eating. Consuming smaller amounts means that you’ll need to be thoughtful in ensuring the calories they do consume are as nutritious as possible. Keep in mind that they still need a balanced diet. Consult your family physician for any caloric guidelines and goals for daily intake of fresh fruits and vegetables, lean proteins, whole grains and low fat dairy. Try to limit excess sugar, gluten, grains, salt and fats which are not only showing to be unhealthful, but also may exacerbate certain behaviors associated with Alzheimer’s/dementia. Use contrasting linens and dishes: Changes in depth and visual perception are also a part of the disease process that can make “seeing” food on the plate difficult. Minimize busy patterns and instead opt for a solid colored plate with a contrasting colored place mat to help food items stand out. Finger foods: Decreases in attention span and ability to sit still for long periods of time may prevent your loved one from staying at the table long enough to get adequate nutritional intake. Try serving finger sandwiches, fruit and veggie slices, cheese and crackers, and other foods that can be consumed away from the table, “on the go” and without having to use silverware. Offer fluids frequently: To decrease the risk of dehydration offer water, juices and higher water content snacks like fruit, popsicles and Jell-O to supplement water consumption. Clear liquid can be difficult to see in a clear glass, so adding orange or lemon slices can make it easier for your loved one to identify water in their cup and make it look more appealing. Prepare the plate: Before serving your loved one, take care to cut up meats and larger food items and add any condiments (spices, gravies or sauces) that your loved one enjoys. Eliminate the need for them to perform multiple, sequential steps to consume their meal. Use adaptive equipment. Consider using scooped plates with higher rims around the perimeter and sectioned plates or bowls to make it easier to get the food out. Large-handled silverware, “Sippy” cups with lids and foods served in edible containers (pita’s, cones, and sandwiches) that can go with your loved one and be consumed on the move are another helpful option for those who can no longer use silverware. Create a routine: Try to offer meals around the same time each day, in the same place and join your loved one at the table. Meal times can be more successful when they are also a social experience and joining with your loved one in partaking of a small meal or a snack can encourage them to eat. Your loved one may also eat more by “mirroring” you as you offer them visual cues or demonstrate eating yourself. Decrease the distractions: Mealtimes can be stimulating enough with all of the sights, sounds, smells, tastes and textures to experience. Be mindful of noise levels and impact of additional stimulation from other people, pets, or media such as television or certain kinds of music. Try to create a quiet, relaxing environment for mealtimes. Allow twice as much time for meals and then double that. If you know that you have an early morning doctor’s appointment tomorrow morning, make a quiche ahead of time that you can just reheat quickly or put together a yogurt and fruit parfait the night before. Spend less time making the breakfast so your loved one has more time to eat it making things less hectic for you both. Make mealtime an enjoyable experience. Keep abreast of new studies being conducted that are researching the impact diet and nutrition choices have on overall symptoms, brain health and behavior for persons living with Alzheimer’s/dementia. Learn more simple solutions for common caregiver challenges in Mara’s new book, “When Caring Takes Courage: A Compassionate, Interactive Guide for Alzheimer’s and Dementia Caregivers” or visit her page on Facebook: Biography Based Care.