Pharm Study Guide for GI and Cardio
advertisement

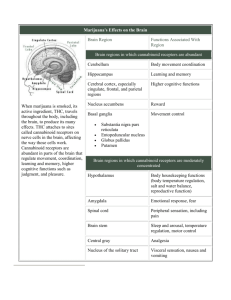
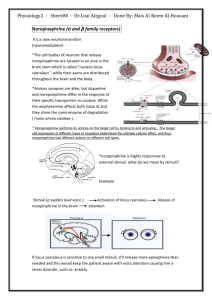
Pharm Study Guide for GI and Cardio GI Pharm I-III 1. Define the neuronal, paracrine, and endocrine regulators of gastric secretions (mucus and acid). a. Parietal cell is final common pathway for the secretion of acid (HCl) and represents a key site of pharmacological regulation. b. Gastrin – Endocrine - regulator both directly and indirectly. Gastrin is secreted into the blood by endocrine G cells of the stomach. Gastrin can directly stimulate the parietal cells to increase activity of the H+-K+-ATPase or indirectly by inducing the release of histamine from ECL cells. c. Neurocrine regulation of acid secretion by acetylcholine is mediated by both direct stimulation of the parietal cell and indirect stimulation of ECL cells resulting in the release of histamine. Histamine release from ECL cells onto neighboring parietal cells (paracrine regulation) stimulates H+-K+-ATPase activity. d. Gastric mucosal protection is mediated by several factors. The paracrine release of prostaglandins (PGE2) ↓’s or negatively regulates H+-K+-ATPase activity. Additionally, prostaglandins and acetylcholine promote the secretion of mucus and bicarbonate from gastric epithelial cells. Finally, the release of somatostatin into the blood by gastric D cells ↓’s acid secretion by inhibiting the release of gastrin from G cells, inhibiting the release of histamine from ECL cells, and inhibiting H+-K+-ATPase activity 2. Understand the therapeutic strategies to treat gastric ulcers and H. pylori infections. a. Treatment of H. pylori positive patients with ulcers utilizes agents to reduce acid production and eliminate the bacterial infection. Older therapeutic regimes used to eradicate H. pylori employed three agents, and was coined “triple therapy”. This strategy employed bismuth subsalicylate, tetracycline, and metronidazole. The modern “triple therapy” strategy utilizes a PPI, clarithromycin, and amoxicillin or metronidazole. The newer line of defense may be combined with the bismuth subsalicylate for “quadruple therapy”. (One acid reducer and 2 abxs) 3. Understand the mechanism of action, adverse effects, and therapeutic use of each of the agents used to treat acid-peptic disease. Antacids 1 Duration of Action Agent Rate of reactivity Sodium bicarbonate [NaHC03] Calcium carbonate [CaCO3] Magnesium hydroxide [Mg(OH)2] Common adverse effects Specific Adverse effects fast -metabolic alkalosis* -excessive NaCl absorption* -gas/bloating* moderate -acid rebound* -gas/bloating* -hypercalcemia (large doses) -hypophosphatemia (rare) -reduced drug bioavailability 1- 2 hrs. slow -enteric infection Aluminum hydroxide [Al(OH)2] -osmotic diarrhea* -hypermagnesemia (large doses over extend periods of time) -constipation* -aluminum toxicity (impaired renal function) -hypophosphatemia -bone resorption -hypercalcemia slow H2-receptor antagonist Agent Duration of action Common adverse effects cimetidine (Tagemet) (safe drugs) headache* ranitidine (Zantac) nizatidine (Axid) 10 hrs. or 6 hrs. OTC diarrhea fatigue, constipation, infection, drug kinetics, bradycardia (IV), hypotension (IV) famotidine (Pepcid) Adverse effects Cimetidine specific considerations: -CNS effects (confusion, hallucinations, agitation) -endocrine effects (inhibition of androgen receptors, inhibition of estradiol metabolism, increase prolactin levels) -inhibition hepatic CYP metabolism Proton Pump Inhibitors (PPIs) Agent Duration of action Omeprazole (Prilosec) Lansoprazole (Prevacid) Rabeprazole (Aciphex) Esomeprazole (Nexium) Pantoprazole (Protonix) Common adverse effects Adverse effects -Extremely safe 24 hours -Decreased drug bioavailability Takes 3-4 days of dosing to -Diarrhea, reach max effect headache, abdominal pain (1-5%) -Decreased nutrient absorption (Vitamin B12, Iron, Calcium, Zinc) -enteric & respiratory infection 2 Mucosal Protective Agents Agent Duration of action Sucralfate (Carafate) Misoprostol (Cytotec) Bismuth subsalicylate (Pepto-Bismol) 6 hours Common adverse effects Adverse effects Constipation, impaired drug absorption Caution w/ renal insufficient patients Cramping, diarrhea abortificient Blackening of stool and tongue High doses salicylate toxicity 4. Understand key regulatory receptors and their ligands of gastrointestinal motility. a. Prokinetic agents Gastrointestinal motility is dopamine 5-HT regulated by multiple D2 D2 5-HT4 5-HT4 5-HT4 neurotransmitters and ENS hormones. The receptors neurons that these neurotransmitters D2 D2 and hormones activate are Ach Ach excellent targets for M3 M3 MR AchE pharmacological regulation GI smooth muscle of gastrointestinal motility. Serotonin (5-HT) is a 5-HT4 Serotonin receptor-4 AchE Acetylcholinesterase common neurotransmitter of D2 Dompamine receptor-2 Muscarinic receptor-3 M3 the enteric nervous system (ENS) that stimulates MR Motilin receptor gastric motility through inducing the release of acetylcholine by neurons onto gastrointestinal smooth muscle. Additionally, serotonin plays a role in relaying sensory information from the gut to the CNS. Targeting serotonin receptors has had some therapeutic utility however its clinical usefulness and safety is under constant evaluation. Dopamine activates presynaptic receptors to ↓ the firing of ENS neurons, which serves to ↓ gastric motility. Antagonizing these receptors will therefore ↑ neuronal firing and GI motility. The parasympathetic and ENS neurotransmitter, acetylcholine (Ach) activates muscarinic receptors to induce contraction of gastrointestinal smooth muscle. The inactivation of acetylcholine is mediated in part through degradation by acetylcholinesterase (AchE). Therefore agonists to the M3 receptor and inhibitors of AchE will increase motility. Unlike the neurotransmitters 5-HT, Ach, and dopamine, motilin is a hormone. Motilin promotes gastric motility through activation of motilin receptors located on gastrointestinal smooth muscle. . 3 These receptors are sites of pharmacological intervention that can be regulated by several agonists and antagonists to promote the contraction of gastrointestinal smooth muscle, as indicated in the table. Agent Mechanism of Action Metoclopramide (Reglan) D2 antagonist Bethanechol (Urecholine) Neostigmine (Prostigmin) Erythromycin (Erythrocin) M3 agonist AchE inhibitor Motilin Receptor agonist Use Adverse effects - GERD - Impaired gastric emptying - dyspepsia - antiemetic - CNS (restlessness, drowsiness, insomnia, anxiety) - altered motor function (Parkinsonian symptoms) - GERD - gastroparesis Cholinergic side effects Non-obstructive: -urinary retention -abdominal distension Cholinergic side effects - gastroparesis Erythromycin mediated side effects 5. Understand the regulatory inputs that mediate an emetic response. a. An emetic response can be initiated by sensory stimulation, blood-borne emetics, or gastrointestinal irritants. The emetic response is ultimately mediated through the emetic center located in the medulla. Regulation of this response at the receptor level is under control of serotonin, dopamine, muscarinic, histamine, and neurokinin receptors. Simply antagonizing these receptors can block or blunt an emetic response. Pharmacologist's view of emetic stimuli. Myriad signaling pathways lead from the periphery to the emetic center. Stimulants of these pathways are noted in italics. These pathways involve specific neurotransmitters and their receptors (bold type). Receptors are shown for dopamine (D2), acetylcholine (muscarinic, M), histamine (H1), and 5hydroxytryptamine (5-HT3). Some of these receptors also may mediate signaling in the emetic center. Goodman & Gilman's The Pharmacological Basis of Therapeutics, 11th Edition 4 b. In addition to antagonizing these receptors, other central nervous system targets are useful in the suppression of an emetic response. These sites include GABAergic neurons, cannabinoid receptors throughout the CNS, glucocorticoid receptors, and opioid receptors at non-emetic center sites. The following agents are useful in the suppression of an emetic response : Agent Ondansetron (Zofran) Mechanism 5-HT3 antagonist Use Adverse effects - Chemotherapy - Postoperative - Postradiation - Headache - Dizziness - Constipation - Prolonged QT interval Scopolamine (Transderm Scop) M1 antagonist - Motion sickness - Antimuscarinic effects Metoclopramide (Octamide) D2 antagonist Chemo- & radiationtherapy induced nausea and vomiting -Extrapyramidal (Parkinsonian symptoms) - Motion sickness - Drowsiness - Chemotherapy - Fatigue - Dizziness - Diarrhea - CYP3A4 Interactions - Severe nausea & vomiting - Extrapyramidal - Drowsiness - Anticholinergic - Anxiety/Chemotherapy - Drowsiness - Chemotherapy -Dysphoria -Sedation -Increased appetite -Chemotherapy -Postoperative - Weight gain - water retention - other corticosteroid effects Dimenhydrinate (Dramamine) Aprepitant (Emend) Prochlorperazine (Compro) Lorazepam (Ativan) Nabilone (Cesamet) H1 antagonist NK1 antagonist M1 D2 H1 antagonist GABA agonist Cannabinoid agonist Dexamethasone Glucocorticoid agonist (increase effectiveness of 5-HT antagonists) 6. Understand the mechanism of action, adverse effects, and therapeutic use of agents for the treatment of motility, emetic, and water flux disorders. (See Emetics suppressants above) 5 Laxatives Agent Mechanism of Action Bulk-forming Methylcellulose (Citrucel) Fiber Adds bulk and retains H20 Surfactant Glycerin (Colace) Coates and penetrates fecal material Use Adverse Effect - gas/bloating constipation minimize straining - nutrient malabsorption prior to surgical and endoscopic procedures - gas - electrolyte flux poor Osmotic Lactulose (Enulose) Change osmotic pressure Stimulant Senna (Ex-Lax) Stimulate ENS Serotonin Agonist Tegaserod (Zelnorm) Absorp. 5-HT4 agonist -GI irritation 10% chronic idiopathic constipation - GI - CV - note: not available for general use Chloride Channel Activator Lubiprostone (Amitiza) Prostaglandin Derivative poor chronic constipation - nausea/vomiting - diarrhea Antidiarrheals Agent Mechanism of Action Loperamide (Imodium) Diphenoxylate (Lomotil) diarrhea (IBS) Opioid agonist diarrhea Bismuth subsalicylate (Pepto-Bismol) -Inhibit PG synthesis (intestinal) - Absorb toxins Kaolin & Pectin (Kaopectate) - Add bulk, absorb toxins Cholestyramine (Prevalite) Use Bind bile acids and salts -non-specific diarrhea -travelers diarrhea diarrhea Impaired bile-salt absorption mediated diarrhea Octreotide (Sandostatin) Somatostatin receptor agonist Secretory diarrrhea Adverse effects Constipation (very safe) CNS effects, atropine effects Salicylate toxicity Constipation -Bloating, flatus, constipation -Fecal impaction -Impaired fat absorption -Impaired pancreatic secretion -Decreased GI motility (nausea, pain) -Decreased gall bladder contraction - Glucose homeostasis 6 7. Understand the pathophysiological differences between IBS and IBD. a. Irritable Bowel Syndrome (IBS) - Irritable bowel syndrome is an idiopathic chronic relapsing disorder characterized by abdominal discomfort (pain, bloating, distension, or cramps) in association with alterations in bowel habits (diarrhea, constipation, or both). - Since the cause of this disease is unknown, current therapeutic strategies are aimed at relieving symptoms, such as reducing pain and improving bowel function. Common approaches to treating IBS-associated pain include use of low doses of tricyclic antidepressants (desipramine and amitriptyline) or antispasmodics/antimuscarinic agents (dicyclomine and hyoscyamine). The use of tricyclic antidepressants results in impaired uptake of serotonin and other amines. This results in downregulation of serotonin receptors in the CNS which results in a blunted pain response from GI afferent fibers. The antimuscarinic agents block GI smooth muscle contraction and spastic activity that may contribute to the pain associated with IBS. Antidiarrheal agents are useful to treat IBS-associated diarrhea and conversely laxatives are used to treat IBS-associated constipation. More recent therapies have taken advantage of more direct serotonergic regulation of bowel motility and sensation. Activation of both 5-HT3 and 5-HT4 receptors stimulates motility. 5-HT3 receptors are also important in relaying sensory information, such as pain, to the CNS. Therefore antagonizing 5-HT3 receptors can be used to relieve pain and diarrhea, while stimulating 5-HT4 receptors can be used to relieve IBS-associated constipation. - Serotonin agonists and antagonists currently or recently used in the treatment of IBS are: Tegaserod (Zelnorm) and Alosetron (Lotrenex) b. Irritable Bowel Disease (IBD) - Inflammatory bowel disease (IBD) can be divided into two distinct diseases, ulcerative colitis and Crohn’s disease. Both diseases are characterized by inflammation of the GI tract. However the exact pathogenesis of each disease remains to be determined. Crohn’s disease can affect any part of the GI tract but is generally associated with the ileum. The site of origin for Crohn’s disease is the intestinal submucosa and eventually spreads to the mucosa and serosa and is often characterized by its pattern of skip lesions. Ulcerative colitis affects the large intestine and originates in the crypts of Lieberkühn. - The therapeutic strategies for the treatment of IBD are common strategies to suppress inflammation and include: 5-aminosalicyclic acid therapy, glucocorticoids, immunosuppressive agents, anti-TNF therapy. - The aminosalicylates work “topically” at the mucosal surface of the gastrointestinal tract. Absorption of the agents prior to delivery of drug to the inflamed tissue renders them ineffective. Therefore the agents have either been chemically modified or packaged to prevent absorption by the gut so as to more effectively reach the target tissue. The precise mechanism of action of these agents is not clearly defined. Possible mechanisms of action may include the inhibition of the inflammatory cytokines IL-1 and TNF-, scavenging of free radicals, inhibition of the transcription factor NF-B, and possibly the inhibition of COX. Key 5-ASA compounds and their targets are summarized below. 7 Aminosalicylates: 5-aminosalicylic acid (5-ASA) Agent Administration Target Modification colon Azo bond linked (N N) MesalaminePentasa Throughout the intestine Time release microgranules MesalamineAsacol ileum/proximal colon pH sensitive resin Rectum/sigmoid colon High concentrations Sulfasalazine Balsalazide Olsalazine MesalamineRowasa & Canasa oral Enema or suppository 8. Understand how serotonin regulates motility and the sensation of pain in the gastrointestinal tract. a. Serotonin (5-HT) is a common neurotransmitter of the enteric nervous system (ENS) that stimulates gastric motility through inducing the release of acetylcholine by neurons onto gastrointestinal smooth muscle. Additionally, serotonin plays a role in relaying sensory information from the gut to the CNS. Targeting serotonin receptors has had some therapeutic utility however its clinical usefulness and safety is under constant evaluation. 9. Understand the therapeutic strategies for the treatment of both diarrhea- and constipationpredominant IBS. a. targeting serotonin receptors to modulate GI function holds significant theoretical promise. Tegaserod is a 5HT4 receptor agonist that was first approved for the treatment of irritable bowel syndrome (IBS)-constipation predominant and chronic idiopathic constipation b. The antimuscarinic agents block GI smooth muscle contraction and spastic activity that may contribute to the pain associated with IBS. Antidiarrheal agents are useful to treat IBSassociated diarrhea and conversely laxatives are used to treat IBS-associated constipation. More recent therapies have taken advantage of more direct serotonergic regulation of bowel motility and sensation. Activation of both 5-HT3 and 5-HT4 receptors stimulates motility. 5-HT3 receptors are also important in relaying sensory information, such as pain, to the CNS. Therefore antagonizing 5-HT3 receptors can be used to relieve pain and diarrhea, while stimulating 5-HT4 receptors can be used to relieve IBS-associated constipation. - Serotonin agonists and antagonists currently or recently used in the treatment of IBS are: Tegaserod (Zelnorm) and Alosetron (Lotrenex) 8 10. Understand the 5 key therapeutic strategies in the treatment of IBD. 11. Understand the mechanism of action, adverse effects, and therapeutic use of the agents used for the treatment of IBS and IBD. Glucocorticoids Agent Administration Prednisone 1. Prednisolone Hydrocortisone Mechanism IV, oral , suppository 2. 3. 4. Suppression of inflammatory cytokines (TNF, IL-1) Suppression of chemokines (IL-8) Suppression of adhesion molecules Suppression of signal transduction molecules that mediate cytokine and chemokine activities (NOS, PLA2, COX2, NF-B) Budesonide 9 Antimetabolites (CA chemotherapeutic agents) Agent Administration 6-mercaptopurine azathioprine IM, SC, and orally methotrexate Mechanism Inhibition of purine synthesis resulting in decreased DNA synthesis and repair leading to decreased cell proliferation Inhibits DHFR resulting in impaired cellular proliferation. Antibiotics – metronidazole, cirprofloxin, and clarithromycin Probiotics Important agents in treating IBD Agent Use Sulfasalazine (Azulfidine ) Ulcerative colitis Adverse effects Nausea, GI upset, headacehe, arthralgia, myalgia, bone marrow suppression, malaise (40%) Very safe Mesalamine Ulcerative colitis (Pentasa) Prednisone (Predone) * Moderate to severe active IBD Glucocorticoid adverse effects Azathioprine (Azasan) Maintenance of remission Nausea, vomiting, bone marrow of IBD (onset 17 weeks) suppression. Methotrexate (Rheumatrex) Maintenance of remission Low dose side effects uncommon, of Crohn’s but include bone marrow depression (onset 8-12weeks) Infliximab (Remicade) Moderate to severe IBD infection Inflixamab is a mouse/human chimeric immunoglobulin that binds and sequesters TNF. The TNFantibody complex cannot bind to the TNF receptor and stimulate the production of inflammatory cytokines thus inhibiting an inflammatory response. 12. Review and understand attached case studies. 10