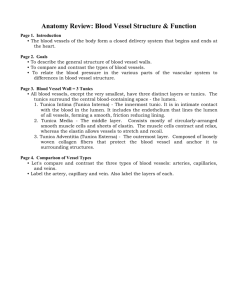
Blood Vessels
advertisement

CARDIOVASCULAR SYSTEM: Blood Vessels Chapter 21 Remember: Blood is Heart is the Blood vessels are the “pipes” transport blood, permit exchange of nutrients, hormones etc. Types of Vessels Arteries: Arterioles: smaller diameter <.5 mm Capillaries & Sinusoids: Venules: Veins: Structure of Vessel Walls: Lumen = 1. Tunica intima: 2. Tunica media: 3. Tunica externa or adventitia: Internal elastic lamina (membrane): External elastic lamina (membrane): Differences between Arteries and Veins: 1. Artery walls are thicker smooth muscle contracts or relaxes vasoconstriction vasodilation 2. Arterial lumens are smaller 3. Arteries are subject to higher pressure arterial recoil: aneurysm: 1 4. Arteries carry blood away from the heart 5. Veins usually have valves Comparison of vessel wall for arteries & veins: ARTERIES: ELASTIC ARTERIES: •larger arteries closer to the heart (Aorta, LCC, L Subclavian, Brachiocephalic) •composed of tunics •tunica media contains more •large •arterial pulse: stretch/recoil of arteries MUSCULAR ARTERIES: • most arteries of the body • tunica media contains • some are important pressure points ARTERIOLES: •diameter <.5 mm •small lumen •thick tunica media mostly smooth muscle cells •regulate blood flow through vasoconstriction & vasodilation resistance vessels CAPILLARIES: •most numerous •extremely •consist of • site of exchange – slowest flowing blood •Continuous & Fenestrated Capillaries continuous: fenestrated: Capillary Beds: Consists of 2 types of vessels: 1.) vascular shunt 2.) true capillaries 2 metarteriole: (proximal end) at the beginning of direct channel from arteriole to venule precapillary sphincter: at entrance to each capillary - open/close to control blood flow through capillary bed – autoregulation vascular shunt( thoroughfare channel): true capillaries SINUSOIDS: •capillary like vessel – small space VENULES: •drain blood from capillaries •small lumen VEINS: (Reservoirs or Capacitance vessels) • Medium & large veins • Consists of same 3 layers as arteries but tunica media is •Some veins contain valves -prevent -mostly formed in Varicose veins •can be hereditary •found in individuals •if severe are removed and alternate venous pathways take over. Hemorrhoids: Distribution of Blood Heart, arteries and capillaries contain 30-35% of blood volume Veins contain 65-70% termed capacitance vessels because can easily stretch under low pressure 3 Physiology of Circulation: (p. 720 table 21-1) Blood flow: Fastest flowing blood Slowest flowing blood Blood Pressure: arterial blood pressure: venous pressure: circulatory pressure or MAP: capillary hydrostatic pressure: forces molecules out of capillaries Total Peripheral Resistance: Sources of Resistance: 1. Vascular Resistance – friction b/w blood and vessel wall a. Blood Viscosity: b. Blood Vessel Length: c. Blood Vessel Diameter d. Turbulence: increases R creates noise – (bruit) that can be heard with stethoscope Relationship between Blood Flow, Blood Pressure, & Peripheral Resistance: F = ∆P R F= Flow P= Pressure R= Resistance R inversely proportional to r4 If R increases –what happens to F? Why might this be beneficial? If R increases and you need to maintain F, how does the body compensate? Arterial Blood Pressure: Systolic Blood Pressure (SBP): SBP in aorta: 120 mmHg - in pulmonary artery 15 mmHg 4 Diastolic Blood Pressure (DBP) Pulse Pressure (PP): SBP - DBP Mean Arterial Pressure (MAP)= DBP + PP/3 Factors Aiding Venous Return: Venous pressure is very low Muscular pump/compression: skeletal muscle contractions move blood Respiratory pump: Boyle’s Law: V inversely related to P (V↓ = P↑) during inspiration: diaphragm contracts, therefore thoracic cavity volume > abdominal cavity volume -Pressure in vena cava decreases and pressure in abdominal cavity increases so blood flows from abdominal cavity into IVC during expiration: diaphragm relaxes, therefore thoracic cavity volume < abdominal cavity volume -Pressure in thorax increases to push blood from IVC into RA note: abdominal pressure drops & blood flows into IVC from lower extremities Capillary Pressure and Exchange Capillaries are the exchange vessels between blood and tissue cells Very thin walls for diffusion Filtration: Hydrostatic Pressure: Osmotic Pressure: blood colloid osmotic pressure (BCOP) or oncotic pressure 5 CHP = 35 mmHg at arterial end and mmHg at venule end COP or BCOP = 25 mmHg dependent on Net Filtration Pressure (NFP): When HP > OP When OP > HP However, the net pressure of fluid leaving at the arterial end is of fluid entering the capillary at the venous end. more than the net pressure Fluid is lost to the interstitial space daily Imbalances b/w HP and OP cause edema Factors affecting CHP: Factors affecting COP: Cardiovascular Regulation: Tissue Perfusion is dependent on Q, R and BP Want active tissues to receive more blood Autoregulation: Vasodilation or vasoconstriction to control blood flow and blood pressure 1. Local vasodilators/constrictors: relax/constrict precapillary sphincter Vasodilators: Decreased tissue O2 or increased CO2 Lactic acid Nitric oxide (NO) Increased K or H ions in interstitial fluid Increased local temperature Vasoconstrictors: PGs and thromboxanes Myogenic Controls Vascular smooth muscle contracts when stretched - so stretching causes automatic vasoconstriction When low pressure in vessel decreases stretch, vessel vasodilates 6 Blood Pressure Regulation: 1.) Short-term Regulation: controls HR, contractility, or blood vessel diameter 2.) Long- term Regulation: controls BV via renal mechanisms Nervous System (Neural) Controls: vasomotor center control vasoconstriction (NE): most arterioles in body vasodilation (only in skeletal muscles and brain arterioles release NO) all arterioles have vasomotor tone - always partially constricted NE can either cause more or less constriction of smooth muscle Reflex Control of Cardiovascular Function Baroreceptor Reflex: Baroreceptors: monitor stretch Found in the carotid and aortic sinuses BP depends on cardiac output (CO = HR X SV) If BP increases they send info to BOTH the vasomotor and cardiac centers Which would try to lower BP by HR and arterioles If BP decreases how would the vasomotor and cardiac centers respond? Note: sympathetic activation also triggers release of Epi & NE from adrenal medulla Atrial baroreceptors – monitor stretch in right atrium blood entering right atrium = amount blood pumped out of aorta when activated – increase cardiac output Valsalva maneuver: exhaling forcefully against a closed glottis increases intrathoracic pressure which compresses aorta and vena cavae decreases venous return = drop in BP and CO 7 Chemoreceptor Reflex Chemoreceptors found in carotid and aortic bodies Respond to blood CO2, pH and O2 levels in blood and CSF when there is a ↓blood O2, pH or ↑CO2 they are excited and ↑BP vasomotor center: cardiac center: Higher Brain Centers: Emotions Chemical Controls – Hormones and Cardiovascular Regulation – mainly long-term regulation Hormone Adrenal Medulla Hormones Site of Release Mechanism Antidiuretic Hormone (ADH) Angiotensin II (renin) Aldosterone Atrial natriuretic factor (ANF) or peptide (ANP) EPO Cardiovascular response to exercise: HR: increased HR, increased venous return BP: increases - SBP more than DBP SV: CO: 5 L/min up to 30 L/min regular exercise lowers cholesterol, lowers resting HR, improves mood 8 Blood Flow through Organs 1. Brain: receives 750 ml/min of blood 2. Heart: receives 250 ml/min at rest 3. Skin: varies from 250 ml/min to 2500 ml/min 4. Kidneys: 1200 ml/min Clinical Stuff 1. Atherosclerosis & Arteriosclerosis Atherosclerosis: deposit of fats/plaque Arteriosclerosis: 2. Hypertension & Hypotension Hypertension: Prehypertension: Stage 1: Stage 2: Consequences of untreated hypertension: Causes: -primary -secondary Hypotension Reduced cardiac output: (hypovolemia, ↓HR, ↓ venous return) Orthostatic hypotension: 3. Deep Vein Thrombosis (DVT) usually in thigh or calf more common in surgical patients S/S: pain, swelling, redness risk of clot breaking free and causing pulmonary embolism Tx: 9 4. Circulatory Shock ( pgs. 142-144 in Applications Manual: Shock) Early stage: ↓ CO = ↓ BP = ↓ peripheral blood flow= ischemic tissues Sympathetic N.S. responds: ↑HR, ↑CO to try to ↑ BP if unsuccessful – tissues become ischemic, low BP ↓ venous return = ↓CO Later stages (irreversible): damage to cardiac muscle, damage to tissues – vasodilation of blood vessels = circulatory collapse 4. Meds used for BP treatment those used for the heart because: Beta-blockers: Ca++ Channel blockers: ACE Inhibitors: Diuretics (diaqua, oretic, lasix, furoside) Note: The applications manual has excellent clinical information for this unit. Read pages 118-142 for additional information. 10 Arteries and Veins of the Body – see ADAM packet 2 Pulmonary Circuit: Systemic Circuit: aorta: aortic arch, thoracic aorta, abdominal aorta Circle of Willis or Cerebral Arterial Circle (pg. 743) encircles the infundibulum ensures brain gets adequate blood flow from either carotid or vertebral arteries Cerbrovascular accident (CVA) or stroke: middle cerebral artery most common site of a stroke supplies temporal, frontal, parietal lobes: sensory/motor skills damage occurs on opposite side of body as artery Hepatic Portal System: hepatic portal vein – drains venous blood into liver receives blood from: inferior mesenteric, splenic and superior mesenteric veins brings nutrient rich blood to liver for processing liver processes and releases to hepatic vein which empties into IVC Fetal Circulation: pgs. 755-758 Umbilical cord contains umbilical arteries & vein Umbilical arteries: transports deoxygenated blood from fetus to placenta Umbilical veins: transports oxygenated blood from placenta to fetus 11 Shunts: Foramen ovale: between R and L atria Ductus arteriosus: between pulmonary trunk and aorta Ductus venosus: receives blood from umbilical vein and shunts it to the inferior vena cava. pressure changes at birth due to breathing close foramen ovale and ductus arteriosus left atrial/ventricular pressure increases and pulmonary pressure decreases in adults have fossa ovalis and ligamentum arteriosum patent foramen ovale: 12