Systemic Complications Associated with Mastitis in a Holstein Cow
advertisement
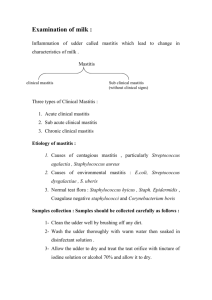
Systemic Complications Associated with Mastitis in a Holstein Cow Christina Butler Clinical Advisor: Dr. Emil Olsen Basic Science Advisor: Dr. Rodrigo Bicalho Senior Seminar Paper Cornell University College of Veterinary Medicine February 5th, 2014 Keywords: mastitis, cow, endotoxemia, endocarditis Summary: An eight-year-old Holstein cow presented to Cornell’s Equine and Farm Animal Hospital for mastitis unresponsive to treatment. She was referred to Cornell from her primary veterinarian following a six day history of mastitis, weakness, anorexia and drop in milk production. On presentation she was febrile, tachycardic, moderately dehydrated and had bilateral hemorrhagic sclerae. Her udder was warm, firm, hyperemic and asymmetrically swollen and her milk was yellow and watery with white flakes. Initial blood work revealed several hematological and biochemical abnormalities suggestive of systemic inflammation. Over the next few days the patient developed a heart murmur of increasing intensity and serial echocardiography revealed evidence of endocarditis and pericardial effusion. Milk, blood and pericardial fluid samples cultured negative for growth of aerobic and anaerobic bacteria, however the cow continued to have recurrent episodes of fever and lethargy. As such, no definitive etiology for the patient’s clinical signs could be identified. This case study will discuss the possible etiologies and treatment strategies of mastitis with secondary endotoxemia, bacteremia and sequelae such as endocarditis and pericarditis in the bovine. 1 Signalment and Case History: An eight year old Holstein dairy cow, 275 days in milk, presented to Cornell for mastitis which was diagnosed while at a state show five days previously. The patient had an extensive show history and was from a small herd with no history of problems with mastitis. Following diagnosis, she was treated by the referring veterinarian with intramammary antimicrobials and prednisone and was treated systemically with IV fluids, tribrissen, ceftiofur, and flunixin meglumine. Two days following initial diagnosis she developed bilateral scleral hemorrhage and went off-feed and was subsequently treated with intramammary gentamicin, intravenous calcium gluconate and subcutaneous penicillin. Despite treatment her clinical signs continued to worsen, and she was referred to Cornell the following day. Presenting Complaint and Initial Clinical Findings: Upon arrival at Cornell’s Farm Animal Hospital the patient’s presenting complaints were a five day history of mastitis non-responsive to treatment, inappetence, depression, and a possible heart murmur which was previously ausculted by the referring veterinarian. On initial physical exam, the patient was dull and depressed, febrile and tachycardic with a temperature of 105.1°F and heart rate of 96 beats per minute. Her mucous membranes were pale with a capillary refill time of less than 2 seconds and she had bounding jugular pulses bilaterally, but no other evidence of heart failure such as brisket edema or bottle-jaw. The heart murmur previously ausculted by the referring veterinarian was not noted on initial physical exam, but was detected the following day. Her eyes were sunken, she was approximately 8-10 percent dehydrated and her sclerae were bilaterally hemorrhagic. Her udder was diffusely firm, warm and hyperemic and the left side was enlarged to two times the size of the right udder. Milk sampled from the left front and hind 2 quarters was yellow and serum-like in appearance with many white flakes, and all four quarters were 3+ positive on California Mastitis Test (CMT). In the middle third of her neck was a firm, swollen, painful region overlying her jugular, which was presumed to be the site of previous intravenous injections. Significant findings on point of care blood work included mild hypokalemia (1.8 mg/dL) and hypocalcemia (1.13 mg/dL). Abnormalities noted on CBC included an inflammatory leukogram (segmented neutrophils 6.8 thou/uL, band neutrophils 4.2 thou/uL), as well as moderate thrombocytopenia (91 thou/uL). Problem List and Differential Diagnoses: Based on history, physical exam findings and initial diagnostic test results, the patient’s problem list included a painful, swollen udder with grossly abnormal milk in all four quarters, fever, tachycardia, moderate dehydration, a heart murmur, bounding jugular pulses, bilateral hemorrhagic sclerae, anorexia, hypocalcemia, hypokalemia, an inflammatory leukogram and moderate thrombocytopenia. From this list, two major problems were identified: mastitis and systemic inflammation or infection, with endotoxemia and septicemia being the most likely causes for the patent’s systemic illness. The most common causes of endotoxemia in cattle are toxic mastitis and metritis1; with other possible causes including pneumonia, pleuritis, peritonitis, pericarditis, acute enteritis, ruminitis or abomasitis, endocarditis or vasculitis. The patient’s clinical mastitis with no response to treatment was the most likely cause for her signs of systemic illness; however, endocarditis could not be ruled out given her heart murmur, tachycardia and jugular pulses. Initially, vasculitis was also a differential as given the painful area overlying the patient’s left jugular vein, but this differential was ruled out following ultrasonographic 3 evaluation which indicated that the inflammation was limited to the soft tissues superficial to the vein. Initial Stabilization and Treatment: To address the patient’s hypovolemia and tachycardia presumptively resulting from endotoxemia she was initially stabilized with intravenous administration of 2 liters of hypertonic saline followed by a 30 liter bolus of intravenous plasmalyte supplemented with 20 mEq/L of potassium chloride to treat her electrolyte abnormalities. Additionally, 500 mL of calcium gluconate was added to her fluids to treat her mild but persistent hypocalcemia. She was given flunixin meglumine, an NSAID, as an anti-pyretic, anti-inflammatory, and analgesic. In cases of toxic mastitis, frequent stripping of the affected quarters is essential to remove remaining intramammmary organisms, endotoxin and phagocytes whose presence in the udder may cause ongoing immune stimulation1. Given this fact, the patient was given intravenous oxytocin and hand-milked every four hours. The patient was also administered intravenous oxytetracycline, a broad spectrum tetracycline antibiotic, for control of bacteremia and prevention of systemic infection. Diagnostic Plan: Following initial stabilization, a diagnostic plan was formulated to further characterize the cause of the patient’s mastitis as well as her signs of systemic inflammation. Milk samples were taken from each quarter and submitted for culture and sensitivity to determine the bacterial cause of her mastitis. The presumptive cause of the patient’s systemic signs was toxic mastitis resulting in endotoxemia, causing her persistent tachycardia, pyrexia and bounding jugular pulses. However, the following morning, the heart murmur described by the referring veterinarian was clearly 4 ausculted on the patient’s left thorax. Persistent tachycardia, bounding jugular pulses and heart murmur of growing intensity could have been resulting purely from endotoxemia, but further work-up was required to rule out concurrent heart disease or sepsis. To assess the patient’s cardiac status, the diagnostic plan included an echocardiogram and a cardiac troponin level to assess the heart’s function and rule out heart failure. Additionally, blood was collected and submitted for culture, complete blood count and chemistry panel to help determine the cause of the patient’s systemic signs. Diagnostic Test Results: Blood Work: The results of blood work submitted the following day were fairly consistent with point of care blood work from initial presentation. The CBC showed an increasingly severe neutrophilia with a left shift (segmented neutrophils 18 thou/uL, band neutrophils 5.8 thou/uL) and toxic change, indicating persistent systemic inflammation, and a persistent but improving thrombocytopenia (109 thou/uL). The chemistry panel abnormalities showed a persistent hypokalemia (2.7 mEq/L), hypomagnesemia (1.2 mEq/L) and hypoalbuminemia (3.0 g/dL), and the cardiac troponin level was zero, which indicated that there was no evidence of myocardial damage. Echocardiography: The first echocardiogram was performed the day following initial presentation. The tricuspid and mitral valves showed evidence of mild thickening and increased turbulence and regurgitation of blood flow. On the mitral valve were two foci of increased echogenicity. Additionally, there was mild effusion and a few fibrin strands within the pericardial space. Over the next few days the patient underwent two more echocardiograms which showed progressive thickening of the 5 mitral, tricuspid and aortic valves and enlargement of the lesions on the mitral valve. Fluid and fibrin strands continued to accumulate within the pericardial space. Culture Results: Milk samples from all four quarters were submitted for culture and sensitivity, all of which returned no growth. Similarly, blood cultures were negative as well as cultures of pericardial fluid performed following demonstration of pericardial effusion on echocardiogram. Interpretation: The majority of the patient’s blood work abnormalities including hypocalcemia, hypokalemia and hypomagnesemia, were consistent with toxic mastitis. Thrombocytopenia occasionally occurs with endotoxemia, and often is observed in conjunction with disseminated intravascular coagulopathy. DIC may have been occurring in the patient given her bilateral scleral hemorrhage, but she exhibited no other signs of coagulopathy, and scleral hemorrhage can also be a direct result of circulating toxins in cattle1. The presence of an inflammatory leukogram is indicative of systemic inflammation; however, toxic mastitis commonly results in a mature neutropenia rather than neutrophilia due to massive recruitment of neutrophils from general circulation to affected udder tissues. The patient’s persistent neutrophilia in the face of severe clinical mastitis was indicative of a concurrent ongoing inflammatory process. Echocardiographic evidence of valvular thickening and rapidly growing lesions on the patient’s mitral valve were diagnostic for endocarditis. The acute development of the vegetative lesions and the rapidly increasing intensity of the patient’s heart murmur strongly suggested that endocarditis had developed secondarily to a bacteremia which occurred in conjunction with endotoxemia resulting from toxic mastitis. The additional diagnosis of acute bacterial 6 endocarditis was supported by the patient’s development of intermittent fevers, persistent tachycardia and neutrophilia, all of which are common findings with bacterial endocarditis2. Diagnoses: The patient’s final diagnoses were mastitis, which was definitive based solely on gross abnormality of her milk and inflammation of her udder, with toxic mastitis resulting in endotoxemia being the presumptive cause of her systemic illness. Additionally, the diagnoses of endocarditis and pericarditis were confirmed via echocardiogram. Treatment: Supportive therapy with intravenous fluids and flunixin meglumine was continued to counteract the effects of the patient’s endotoxemia. Due to the fact that no causative organism was identified on milk or blood culture, she was treated systemically with oxytetracycline and penicillin to offer broad spectrum coverage of both gram-negative and gram-positive organisms. She was treated with an intramammary infusion of amikacin for coverage of gram-negative organisms, and dexamethasone, a corticosteroid to decrease inflammation in the udder. Because the patient’s milk production continued to decline, she was treated with Spectramast, a broad spectrum dry cow treatment, in all four quarters and subsequently dried off. Prognosis: Over the next few days, the patient continued to exhibit intermittent fevers and went on and off feed. She remained persistently tachycardic and her heart murmur continued to increase in intensity, progressing to a grade IV/VI continuous murmur which was auscultable on the left and right thorax. Despite the evidence of clinical progression of endocarditis, she remained stable 7 and the owner elected to bring her home. The patient was discharged with a grave prognosis for long term survival following eight days as an inpatient at Cornell’s Farm Animal Hospital. Because of this poor prognosis, a recommendation was made to the owner to begin a superovulation protocol to harvest her ova for in-vitro fertilization. Outcome: Following her discharge, the patient showed slow but steady improvement over the course of the next three weeks. By three months later she had returned to normal weight, had an excellent appetite and showed no clinical signs of disease and the owner expressed plans to breed her in the coming year. Discussion: Toxic Mastitis Many mastitis-causing organisms can also cause signs of systemic illness. Staphylococcus aureus and other gram-positive cocci, Mycoplasma bovis, Pseudomonas aeruginosa, Bacillus cereus and mycotic infections have been shown to cause clinical signs which, in the absence of positive culture results, can be virtually indistinguishable from severe coliform mastitis3. However, mastitis caused by severe infection with coliforms is by far the most common cause of systemic illness in cattle1. Coliforms are gram-negative lactose fermenting rod-shaped bacteria such as E. coli, Klebsiella and Enterobacter species. Lipopolysaccharides (LPS), also known as endotoxins, are large molecules found in the outer membrane of these bacteria and when the bacteria are destroyed, this cell membrane component can trigger a powerful systemic inflammatory reaction4. 8 Upon entering the teat, coliforms multiply rapidly by 16 hours after entering the streak canal and overcoming local resistance mechanisms1. Once in the mammary gland, the bacteria are destroyed by phagocytosis and intracellular killing within local phagocytes. Lysis of the bacteria releases endotoxin, causing recruitment of large numbers of neutrophils from systemic circulation. This rapid recruitment results in highly efficient bacterial destruction, but also causes release of even more endotoxin. Damage to local mammary tissue as well as leaky blood vessels allows endotoxin to cross into the blood stream, initiating a cascade of systemic inflammation. In addition to endotoxemia, bacteremia may also occur when surviving bacteria are able to escape into general circulation through these same mechanisms. Systemic circulation of endotoxin causes activation of inflammatory mediators including histamines, serotonin, prostaglandins, IL-1, IL-6 and TNFa, resulting in clinical signs such as the fever, bounding jugular pulses, tachycardia and weakness which were observed in the patient. While it is widely agreed that supportive therapy should be the mainstay of treatment for toxic mastitis, use of systemic antimicrobials remains controversial due to the pathophysiology of infection with gram-negative organisms1. Intramammary bacterial concentrations peak and decline very rapidly following initial infection and resultant large-scale recruitment of neutrophils. The subsequent release of endotoxin following bacterial destruction, not viable bacteria, is the inciting cause for systemic illness associated with toxic mastitis. This has led to debate as to whether systemic antimicrobial therapy is indicated in cases of toxic mastitis, and several studies examining this question have produced mixed results3. However, bacteremia may 9 also occur in up to 48 percent of toxic mastitis cases, which is a strong argument for the use of systemic antimicrobials in the treatment of severe coliform mastitis3. Treatment of severe clinical mastitis is further confounded when culture results are negative, which indeed is often the case. In fact, recent literature has shown that between 25 to 44 percent of milk samples from quarters showing clinical infection return no growth on culture5. Furthermore, molecular sequencing techniques have revealed that microbial populations present within bovine mastitic milk may be more diverse than was previously believed, and that conventional culturing techniques may not reveal the true inciting bacterial cause of mastitis6. Endocarditis: Diseases which cause bacteremia allow circulating bacteria to colonize the heart valves and endocardium and remain relatively protected from the immune system. The most common organisms which cause endocarditis in cattle are Trueparella pyogenes and Streptococcus species, but Staphylococcus species and gram negative organisms such as coliforms may also cause the disease2,7. In cattle the most consistent clinical signs of bacterial endocarditis are intermittent fever, tachycardia and a systolic heart murmur, and definitive diagnosis is via echocardiographic demonstration of valvular thickening and vegetative lesions8. Long-term antimicrobial treatment is required for treatment of bacterial endocarditis, and successful blood cultures allow for selection of the appropriate antibiotic. However, up to 50% of blood cultures will be negative despite definitive diagnosis of bacterial endocarditis1. 10 The prognosis for bacterial endocarditis is guarded for survival of longer than six months, with early recognition and treatment offering the best outcome2. Pericarditis: Echocardiography revealed the presence of effusion and fibrin strands within the patient’s pericardial space. This was a particularly confusing aspect of the case due to the fact that endocarditis and pericarditis are two separate disease processes, which initially suggested that the patient’s bacteremia may have also caused pericarditis or there was a completely different cause for the pericardial effusion. Pericarditis in cattle is most commonly caused by traumatic reticulopericarditis, secondary to pneumonia or pleuritis, neoplastic effusion secondary to lymphoma or mesothelioma and idiopathic aseptic pericarditis2. A pericardiocentesis revealed serosanguinous fluid which showed inflammatory cells and fibrin with no evidence of bacteria on cytology and no bacterial growth on culture. Additionally, radiographs of the cranial abdomen and caudal thorax showed no evidence of traumatic reticulopericarditis. Definitive diagnosis is again via echocardiogram, with demonstration of fluid within the pericardial space. Treatment and prognosis for pericarditis is dependent on its etiology and severity, with clinical evidence of heart failure being a poor prognostic indicator1,2. A definitive cause for the patient’s pericardial effusion could not be identified, and because the amount of fluid within the pericardial space did not increase, specific treatments such as drainage of the fluid or pericardiostomy were not indicated. References 1. Divers, T.J.; Peek, S.F.; Rebhun, W.C.; Diseases of Dairy Cattle. St. Louis, Mo.: Saunders/Elsevier; 2007. 11 2. Buczinski, S.; Rezakhani, A.; Boerboom, D.; Heart disease in cattle: Diagnosis, therapeutic approaches and prognosis. The Veterinary Journal. 2010; 184(3):258-263. 3. Erskine, R.J.; Wagner, S.; DeGraves, F.J.; Mastitis therapy and pharmacology. Veterinary Clinics of North America: Food Animal Practice. 2003; 19(1):109-138. 4. Smith, G.W.; Supportive therapy of the toxic cow. Veterinary Clinics of North America: Food Animal Practice. 2005; 21(3):595-614. 5. Taponen, S.; Salmikivi, L.; Simojoki, H.; Koskinen, M. T.; Pyörälä, S.; Real-time polymerase chain reaction-based identification of bacteria in milk samples from bovine clinical mastitis with no growth in conventional culturing. Journal of Dairy Science. 2009; 92(6):2610-2617. 6. Oikonomou, G.; Machado, V. S.; Santisteban, C.; Schukken, Y.H.; Bicalho, R.C.; Microbial diversity of bovine mastitic milk as described by pyrosequencing of metagenomic 16s rDNA. PLoS ONE. 2012; 7(10). 7. Buczinski, S.; Francoz, D.; Fecteau, G.; Difruscia, R.; A study of heart diseases without clinical signs of heart failure in 47 cattle. The Canadian veterinary journal. La revue vétérinaire canadienne. 2010; 51(11):1239-46. 8. Buczinski, S.; Tsuka, T.; Tharwat, M.; The diagnostic criteria used in bovine bacterial endocarditis: A meta-analysis of 460 published cases from 1973 to 2011. The Veterinary Journal. 2012; 193(2):349-357. 12