IMQ CMA Accreditation Application for CME May 29, 2014
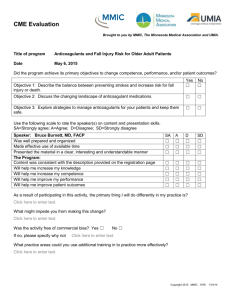
advertisement

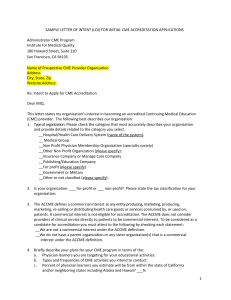
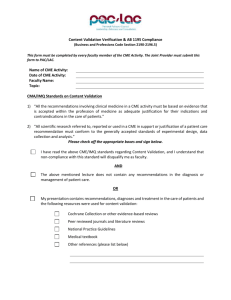
IMQ/CMA Continuing Medical Education Accreditation Program Application for CME Accreditation Please refer to the IMQ Instructions for CME Accreditation Application when preparing the narrative and activity files for submission. 180 Howard Street, Suite 210 San Francisco, CA 94105 415.882.5182 IMQ CME Accreditation Application Section I PROGRAM OVERVIEW 1. Briefly describe the history of your continuing medical education (CME) Program. 2. Describe the leadership and organizational structure of your CME program and how it fits within the overall structure of your organization. Describe the role of the physicians and staff involved, for example, CME coordinator, CME chair, and CME committee. Are there other committees, departments, staff or organizations that contribute to your CME program? Please attach an organizational chart. 3. Does your organization enter into joint providerships (formerly known as joint sponsorship)? Yes or No If yes, briefly describe this component of your program. 4. Does your organization accept commercial support (financial or support-in-kind)? Yes or No 5. Do you offer the following (check all that apply): __ Regularly Scheduled Series (RSS) __ Enduring Materials __ Internet CME __ Journal-based CME Section II PURPOSE & MISSION (CRITERION 1) 6. Attach or insert your CME mission statement that identifies the expected results of your CME program, articulated in terms of changes in physician competence, performance, or patient outcomes. If your mission statement includes multiple elements, please highlight the expected results. Section III EDUCATIONAL ACTIVITY PLANNING (CRITERIA 2-6) The next questions are designed to gather information on the components of your planning process that serve as a basis for a CME activity: 7. Describe how you identify Professional Practice Gaps (PPGs) defining the difference between current practice and desirable or achievable practice or outcomes for your own learners. (C2) 2 ©2014 IMQ May 2014 IMQ CME Accreditation Application 8. Describe how you incorporate into CME activities the educational needs (knowledge, competence or performance) that underlie the Professional Practice Gaps of your learners. (C2) 9. Describe how you generate activities designed to change physician competence, and/or performance, and/or patient outcomes as identified in your mission statement. (C3) 10. Describe what educational format(s) (i.e., activity type and methodology) you use and how you choose educational format(s) that is appropriate to the setting, objectives, and desired results of an activity. (C5) 11. Describe how your activities are planned within the context of desirable physician attributes (e.g., ABMS/ACGME Competencies, IOM Competencies). (C6) 12. Include TWO (2) CME examples for each step of the planning process you have described above that show how you: a. Identify the Professional Practice Gap (PPG) of your own learners that the CME activity was addressing. The PPG is the difference between the current practice and the desired or achievable practice outcome. List the sources of information and/or data you used to determine the PPG. (C2) b. Determine the educational need(s) underlying this gap for your learners. Identify if there was an underlying need for knowledge and/or competence and/or performance. Incorporate this need into the CME activity. (C2) c. Designed the activity to change physician competence and/or performance and/or patient outcomes. (C3) d. Show that the choice of format for the activity is appropriate for the setting, desired results of the activity. (C5) e. Identify the desirable physician attributes or core competencies associated with the activity. (C6) 3 ©2014 IMQ May 2014 IMQ CME Accreditation Application Section IV Commercial Support Independence, Identification and Resolution of Conflicts of Interest, Disclosure to Learners (Criterion 7) NOTE: You must respond to this section, regardless of whether or not your organization accepts commercial support. 13. Describe how your organization ensures independence from commercial interests in the CME planning process, including the identification of needs; determination of educational objectives; selection and presentation of content; selection of all persons and organizations in a position to control the content; selection of educational methods; and evaluation of the activity (SCS1) 14. Describe the mechanism(s) used to ensure that everyone in a position to control educational content (e.g., faculty, planners, reviewers, and others who controlled content) has disclosed to your organization relevant financial relationships with commercial interests. (SCS 2.1) Include in your description if your organization disqualifies individuals who refuse to disclose. (SCS 2.2) 15. Describe the mechanism(s) your organization uses to identify conflicts of interest prior to an activity, for example, use of a disclosure form. (SCS 2.3) 16. Describe the mechanism(s) your organization uses to resolve conflicts of interest prior to an activity. (SCS 2.3) 17. Describe your organization’s process and mechanism for disclosure to the learners prior to the activity of: a. Relevant financial relationships, or lack thereof, for all persons in a position to control educational content b. Source of support from commercial interests, including “in-kind” support, if applicable (SCS 6.1-6.5) c. Prohibition of trade names or product group messages (SCS: 6.4) 18. Include two examples and provide the following for each example: a. List of all CME planners, committee members, faculty, staff, and others that are in a position to influence CME content. (SCS 2.1) b. Disclosure information for all individuals listed. Disclosure information should include Relevant Financial Relationships (RFR) that occurred in the past 12 months, include spouse/partner, and use the correct definition of a Commercial Interest. (SCS 2.1) Identify if anyone was disqualified for refusal to disclose. (SCS 2.2) 4 ©2014 IMQ May 2014 IMQ CME Accreditation Application c. Mechanism used to identify and resolve conflicts of interests (COI) prior to the activity. If applicable, include the documentation of resolution of a COI or state if there were no COIs. (SCS 2.3) d. Disclosure to learners (e.g., copy of slide, handout, or verbal attestation) made prior to the activity of the presence or absence of relevant financial relationships for all who controlled content (SCS 6.1, 6.2, 6.5) e. Disclosure, if applicable, of the source(s) of support including “in-kind” support, from commercial interests. (SCS 6.3-6.5) Section V Management of Commercial Support (Criterion 8) 19. Whether or not your organization accepts commercial support, attach your written policies and procedures governing honoraria and reimbursement of out-of-pocket expenses for planners, teachers, and/or authors. 20. Highlight where in your policy or procedure it states: a. Amount or range of honoraria and what expenses are reimbursable. (SCS 3.7) b. Payment is made directly by the provider or designated education partner and not by commercial interest. (SCS 3.8) NOTE: If your organization accepts commercial support respond to Questions 21 – 23; if not, go to Section VI. 21. Attach a written letter of agreement signed by provider and commercial supporter documenting terms, conditions, and purposes of commercial support and specify the source of commercial support (SCS 3.4-3.6) 22. Provide an example detailing the receipt and expenditure of the commercial support. (SCS 3.13) 23. Describe your process to ensure that: a. You make all decisions regarding the disposition and disbursement of both funds and inkind commercial support. (SCS 3.1). You do not accept advice or services as a condition of receiving support (SCS 3.2) b. All commercial support is given with your organization’s full knowledge and approval (SCS 3.3) c. No other payment is given to the director of the activity, planning committee members, teachers or authors, joint provider, or any others involved in the activity (SCS 3.9) 5 ©2014 IMQ May 2014 IMQ CME Accreditation Application d. If teachers and authors are presenting and participants, their expenses can only be reimbursed as presenters and not as learners (SCS 3.10) e. Social events do not compete with or take precedence over educational activities. (SCS 3.11) f. Commercial support is not used to pay honoraria or expenses for participants who are not teachers or authors. (SCS 3.12) Section VI Separation of Education from Promotion; Promotion of Improvements in Healthcare (Criteria 9-10) NOTE: You must respond to this section whether or not your organization accepts commercial support or arranges for commercial exhibits or promotion in your activities. 24. Do you organize commercial exhibits in association with any of your CME activities? (C9) If yes, describe how your organization ensures that arrangements for commercial exhibits do not (1) influence planning or interfere with the presentation and (2) are not a condition of the provision of commercial support for CME activities. (SCS 4.1) 25. Do you arrange for advertisements in association with any of your CME activities? If yes, describe how your organization ensures that advertisements or other productpromotion materials are kept separate from the education. In your description, distinguish between your processes related to advertisements and/or product promotion in each of the following types of CME activities: (1) print materials, (2) computer-based materials, (3) audio and video recordings, and (4) face-to-face. (SCS 4.2, 4.4) 26. Describe the planning and monitoring your organization uses to ensure that: (C10) a. Content of CME activities does not promote the proprietary interests of any commercial interest (i.e., there is no commercial bias). (SCS 5.1) b. CME activities give a balanced view of therapeutic options (SCS 5.2) c. Clinical content of CME activities is in compliance with the IMQ/CMA content validity statements1. (See Policy on Content Validation) 1 IMQ/CMA’s Policy on Content Validation: All the recommendations involving clinical medicine in a CME activity must be based on evidence that is accepted within the profession of medicine as adequate justification for their indications and contraindications in the care of patients. All scientific research referred to, reported or used in CME in support or justification of a patient care recommendation must conform to the generally accepted standards of experimental design, data collection and analysis. Providers are not eligible for IMQ/CMA accreditation or reaccreditation if they present activities that promote recommendations, treatment or manners of practicing medicine that are not within the definition of CME, or known to have risks or dangers that outweigh the benefits or known to be ineffective in the treatment of patients. 6 ©2014 IMQ May 2014 IMQ CME Accreditation Application Section VII Evaluation and Improvement (Criteria 11-13) 27. Describe how you use data and information to evaluate your program’s activities. Provide a summary of your data and your analysis of changes in your learners’ compentence, performance, or patient outcomes achieved as result of your overall program’s activities. (C11) 28. Submit two activity examples in which you have summarized the data and provided an analysis of changes in your learners’ competence, performance, or patient outcomes. (C11) 29. Based on activity data from Criterion 11, and other relevant information, provide a program-based analysis on the degree to which the expected results component of your CME Mission has been met through your CME activities. In addition to expected results, your program-based analysis may consider the impact of other factors that might contribute to the success of, or impede the CME program (e.g., resources, staff training, technology support, venues, and improvement efforts). (C12) 30. As a result of your program-based analysis (C12), list the program improvements you identified, planned and implemented to help you better meet the expected results component of your CME mission. (C13) Section VIII Cultural and Linguistic Competency (Assembly Bill 1195) NOTE: ALL ORGANIZATIONS must respond to this section. 31. For each planned CME activity, with a clinical care focus, describe: a. How CME Planners proactively determine if there are CLC health disparities relevant to the targeted physician learners and/or their patient populations and do not leave this to presenters or authors. b. When a CLC disparity is identified, describe your process to generate at least one educational component to address the specific need related to the educational activity. c. That you document when no CLC disparity is identified. 32. Include two examples of how planners proactively identified CLC disparities and generated an educational component for clinically-focused CME activity. 7 ©2014 IMQ May 2014 IMQ CME Accreditation Application Section IX IMQ/CMA Policies NOTE: ALL ORGANIZATIONS must respond to this section. 33. Describe the mechanism your organization uses to record and verify physician participation for six years from the date of your CME activities. 34. Include one example that demonstrates your practice to record and verify physician participation. 35. Describe how your organization retains educational activity files in accordance with IMQ/CMA Policies for your current accreditation term or for the last 12 months, or whichever is longer. 36. Include one example of correct use of IMQ/CMA Accreditation Statement and AMA Credit designation statement. 37. If applicable, describe the type of Regularly Scheduled Series (RSS) you conduct and how you plan RSS to be compliant with Criteria 2-11 and policies. (See IMQ/CMA Criteria and Policy for Continuing Medical Education glossary for RSS definition). 38. If you conduct enduring materials, internet CME, Journal-based CME, describe how you are compliant with the AMA and ACCME special requirements. Section X Accreditation with Commendation (Criteria 16-22) OPTIONAL NOTE: Complete the following questions if your organization is applying for Accreditation with Commendation. 39. If your organization integrates CME into the process for improving professional practice, describe how this integration occurs. Include at least two examples of explicit organizational practices that have been implemented. (C16) 40. If your organization utilizes non-education strategies to enhance change as an adjunct to its educational activities, describe the strategies that your organization has used as adjuncts to CME activities and how these strategies were designed to enhance change. Include in your description an explanation of how the non education strategies were connected to either an individual activity or group of activities. Include at least two examples of non-education strategies that have been implemented. (C17) 41. If your organization identifies factors outside of its control that will have an impact on patient outcomes, describe those factors. Include at least two examples of identifying 8 ©2014 IMQ May 2014 IMQ CME Accreditation Application factors outside of your organization’s control that will have an impact on patient outcomes. (C18) 42. If your organization implements educational strategies to remove, overcome, or address barriers to physician change, describe these strategies. Include at least two examples of educational strategies that have been implemented to remove, overcome, or address barriers to physician change. (C19) 43. If your organization is engaged in collaborative or cooperative relationships with other stakeholders, describe these relationships. Include at least two examples of collaboration and cooperation with other stakeholders. (C20) 44. If your CME unit participates within an institutional or system framework for quality improvement, describe this framework. Include at least two examples of your CME unit participating within an institutional or system framework for quality improvement. (C21) 45. If your organization has positioned itself to influence the scope and content of activities/educational interventions, describe organizational procedures and practices that support this. Include at least two examples of how your organization is positioned to influence the scope and content of activities/educational interventions. (C22) 9 ©2014 IMQ May 2014