ANATOMY Circulatory system- cardiovascular system & lymphatic
advertisement

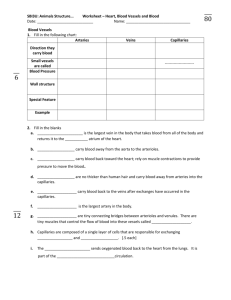
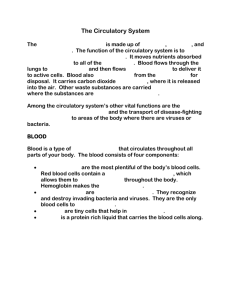
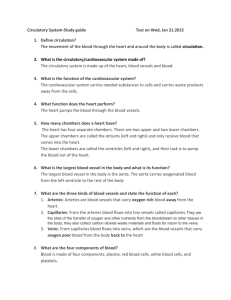
ANATOMY Circulatory system- cardiovascular system & lymphatic system Cardiovascular system- heart, blood vessels, blood Lymphatic system- lymphatic vessels, spleen, thymus, tonsils, lymph nodes Lymphatic system Consists of lymphatic vessels, lymphoid tissue & organs Liquid in lymphatic capillaries is called lymph Used to maintain fluid balance in tissues, to absorb fat from gastrointestinal tract Also part of body’s immune system Vessels drain intercellular fluid into bloodstream in the subclavian veins In small intestine, lymphatic capillaries called lacteals absorb fat away from GI tract Lymph is carried by lymphatic capillaries to lymph ducts that all interconnect & empty into the thoracic duct or the right lymphatic duct Lymph is filtered as it moves through lymph nodes where phagocytic cells purify the fluid Nodes are clustered in specific regions of body Other lymph nodes include the tonsils, spleen & thymus Tonsils- form a protective rings of lymphatic tissue around opening between nasal/oral cavities & pharynx Spleen- not vital in adults but helps other organs make lymphocytes, filter blood & destroy old RBC Thymus- key role in immune system Cardiovascular system Blood Connective tissue with liquid matrix, 3 types of cells suspended in liquid plasma Cells 45% & plasma 55% Average adult has 5L which is 8% of body mass Thicker/more viscous than water pH 7.35-7.45 Cells made in red bone marrow Bright red color indicates presence of oxygen & dull red indicates lack of oxygen Erythrocytes (red blood cells) 5.1-5.8 million/cubic millimeter of blood in males 4.305.2 million in females Most numerous blood cell Biconcave disc shape mature ones lack nuclei & mitochondria Survive 120 days & are then destroyed by phagocytic cells in liver/spleen Oxygen attached to hemoglobin molecules- each hemoglobin can carry 4 molecules Each RBC contains about 280 million hemoglobin molecules Actually 2 kinds of hemoglobin- A & B A makes up 98% of adult’s hemoglobin & B only 2% Made in bone marrow of arm/leg bones, vertebrae, ribs, sternum, skull Leukocytes (white blood cells) 5-10,000/cubic millimeter of blood Least numerous blood cell Larger than RBC & have nuclei/mitochondria Some can move out of capillaries & into tissues to destroy disease causing organisms 10 day life span Made in bone marrow, spleen, thymus & lymph glands Two main types Granulocytes- cytoplasm shows presence of large number of small granules Neutrophils- account for 60-75% of WBC; protect body against infection by eating/digesting foreign matter; usually die within a few hours so live 12-24 hours Eosinophils- 2-4% of WBC; do same as neutrophils but also help break up blood clots by releasing enzymes Basophils- 1% of WBC; release heparin (body’s natural anticoagulant) & secrete histamines (during allergic reactions) Agranulocytes- cytoplasm doesn’t have granules Monocytes- 3-8% of WBC; largest WBC; scavenges for foreign matter; can migrate into surrounding body tissues where they can increase in size & become macrophages that continue to scavenge for foreign matter Lymphocytes- 20-25% of WBC; smaller size with large nucleus & little cytoplasm; become B cells & T cells of immune system Thrombocytes (platelets) Fragments of larger cells in red bone marrow Lack nuclei 250,000-450,000/cubic millimeter of blood Can move out of capillaries Capable of amoeboid movement Live 5-9 days & then are destroyed by spleen/liver Important role in blood clotting & blood clot formation Rich in secretory granules that trigger clot formation/coagulation Stick to damaged areas & seal breaks Plasma Straw colored liquid where blood cells are suspended 90% water, rest is proteins, inorganic salts (sodium, potassium, calcium chloride, phosphates), carbohydrates (sugars), lipids, amino acids, chemical waste (urea, uric acid), vitamins, hormones Transports nutrients, gases, vitamins Regulates electrolyte/fluid balance & maintains blood pH Plasma proteins- 7-9% of plasma Albumins- smallest but most numerous proteins, made by liver, make blood thick, help regulate blood pressure (osmotic pressure) & transport lipids/bile Globulins- made in liver or lymphoid tissue; transport lipids, hormones, iron & vitamins as well as helping with immunity Fibrinogens- large proteins made in liver; help in blood clotting by forming a matrix where cells get trapped Heart Transport pump that keeps blood continuously circulating through body Roughly the size of fist 255 g in adult females & 310 g in adult males Contracts 42 million times/yr pumping 700,000 gallons of blood Located in thoracic cavity between lungs Parietal pericardium (pericardial sac) Loose fitting double walled sac of dense fibrous connective tissue that encloses/protects heart Forms wall of pericardial cavity that is filled with pericardial fluid Wall of heart Epicardium- outer layer; also called visceral pericardium Myocardium- thick middle layer made of cardiac muscle tissue; layer that actually contracts Endocardium- inner layer of wall; continuous with endothelium of blood vessels Interior of heart- 4 chambers; right/left halves separated by septum Atria- two upper chambers separated by thin muscular interatrial septum; each has ear shaped expandable appendage called an auricle Ventricle- two lower chambers separated from each other by thick muscular interventricular septum; walls are thicker than atria since must push blood farther (left is thicker than right) Valves- 4 total Atrioventricular valves- AV valves between atria/ventricles; bicuspid or mitral valve on left side, tricuspid on right side Semilunar valves- between ventricle & arteries leaving heart; pulmonary valve & aortic valve Blood circulation routes Blood in heart Superior vena cava & inferior vena cava drain deoxygenated blood from body into right atria; blood passes through tricuspid valve to fill right ventricle; when the ventricle contracts it pushes the blood through the pulmonary valve to the pulmonary arteries; the blood leaves the heart here to go to the lungs to drop off carbon dioxide & pick up oxygen; the pulmonary veins deposit oxygenated blood into the left atrium; blood passes through the bicuspid valve to fill the left ventricle; when the left ventricle contracts with a mighty force the blood exits the heart through the aortic valve & the aorta Pulmonary circulation Vessels transport blood to the lungs & then back to the heart after blood has refreshed its oxygen level; pulmonary arteries are only arteries that transport deoxygenated blood; pulmonary veins are only veins to carry oxygen rich blood; right ventricle of heart pumps blood to lungs for purpose of enriching the blood’s oxygen content & diminish the carbon dioxide content System circulation Vessels transport blood from left ventricle of heart, through body & back to the right atrium; delivers oxygen & picks up carbon dioxide from body; left ventricle of heart pumps blood to all the body’s organs to nourish & remove wastes; aorta, arteries, arterioles, capillaries, venules, veins, vena cava Coronary circulation Vessels that supply the heart walls with the oxygen it needs; made of coronary arteries that exit the aorta & the coronary veins deliver blood back to the right atrium through the coronary sinus Contraction of heart is controlled by specialized strands of interconnecting cardiac muscle tissue (sinoatrial node, atrioventricular node, atrioventricular bundle & conduction myofibrils) SA node is called the pacemaker & is found in the posterior wall of the right atrium SA node initiates the contraction, AV node in inferior portion of interatrial septum sends signal on to AV bundle between ventricles Contraction of ventricles is systole & their relaxation is diastole These cause pressure in arteries & is measured as blood pressure Sounds of heart come from 2 actions “lub” is made when AV valves close “dub” is from closing of other valves Both right/left sides of heart act together- both atria fill at the same time, both ventricles fill at the same time, both ventricles expel blood at the same time Blood vessels Form closed network of tubes that allow blood to flow through body If lined up end to end an adult human’s blood vessels would circle the Earth’s equator 4 times Walls of arteries/veins are made of 3 layers Tunica externa (adventia)- outermost layer made of loose connective tissue Tunica media- middle layer of smooth muscle & elastic fibers Tunica interna (intima)- innermost layer made of simple squamous epithelium & elastin; also called endothelium Differences between arteries & veins Arteries have more muscle than veins thus thicker walls; arteries are both strong/elastic Arteries appear more round than veins Arteries carry blood away from heart; veins carry blood toward heart Veins are usually partially collapsed because they don’t fill all the way Veins can stretch more & have valves inside them Veins aren’t found in the wall of the heart Arteries Expand with pressure of blood when heart contracts & recoil when pressure decreases Small muscular arteries are 100 micrometers or less in diameter Capillaries 7-10 micrometers in diameter Functional unit of circulatory system since this is where exchange of gases, nutrients & wastes occurs Over 40 billion capillaries in body Walls are only 1 cell layer thick Blood flows slowest here but there is little frictional resistance to the movement of blood Types of capillaries Continuous- those in which adjacent endothelial cells are tightly joined together Found in muscles, lungs, adipose tissue & CNS Fenestrated- have wide intercellular pores that are covered by layers of mucoprotein Occur in kidneys, endocrine glands & intestines Discontinuous- large spaces between endothelial cells Found in bone marrow, liver & spleen Veins Carry oxygen poor blood from capillaries back to heart Very little pressure which isn’t enough to return blood to heart Massaging action of muscles as well as presence of venous valves moves blood through Valves in medium-large veins Valves help to move blood by preventing blood from flowing backwards Blood pressure Force exerted by blood against the inner walls of the vessels through which it flows Considered a vital sign Measured with sphygmomanometer over the brachial artery Normal is 120/80 Difference between the two numbers is the pulse pressure Diminishes the further the blood moves from the heart PHYSIOLOGY Major jobs of circulatory system Transport oxygen, nutrients & raw materials to body’s tissues Remove carbon dioxide & metabolic waste from body’s tissues Transport hormones & other secretory substances from one tissue/organ to another Distribute body’s heat of metabolism Regulation of body homeostasis Protection against disease Cardiac cycle Sequential actions of heart’s chambers About 0.8 sec long if heart is beating 75 times/min Begun by SA node Systole- contraction of heart chamber that empties it Atrial systole 0.1-0.2 sec Ventricular systole 0.3 sec Diastole- relaxation of a heart chamber to it can fill About 0.5 sec long Right/left atrial systole occur at same time & are accompanied by right/left ventricular diastole Ventricular systole accompanied by atrial diastole When chambers contract, they do not eject all of the blood in them (only about 50-60%) The more blood entering the ventricle, the greater the force with which the ventricle contracts to eject it (Frank-Starling Law of the Heart) Stroke volume- volume of blood expelled from left ventricle with each systole About 70 mL of blood when resting & more during exercise Cardiac output or minute voume 5250 mL of blood (70 mL x 75 beats/min) at rest & more when exercising Amount of blood leaving heart If average adult male has 5 L of blood & a resting cardiac output of 5250 mL then it takes an average of 1 min for a drop of blood to circulate through the body If you have a major leak & had been working out, it could take about 7 sec to pump your body dry or about 63 sec at resting heart rate Blood pressure Pressure against the walls of the vessels through which blood is flowing Decrease between aortic pressure & vena cava pressure is due to friction within the blood & between the blood/vessel walls called peripheral resistance Must use artery to measure blood pressure because venous pressure is very low (almost 0 mm Hg in vena cava) Systolic blood pressure- occurs at peak of ventricular contraction 120 mm Hg Diastolic blood pressure- occurs as left ventricle relaxes/fills with blood 80 mm Hg Pulse pressure- difference between systolic/diastolic pressures Measuring with sphygmomanometer Pump air into cuff until pressure level reaches 180 mm which stops flow of blood in arm No sounds will be heard Slowly release air from cuff & listen. When faint Korotkoff sounds are heard note the pressure (systolic) As cuff pressure continues to drop the sound will fade. Note the pressure when sounds can no longer be heard (diastolic) Factors affecting blood pressure Nervous control via reflex arcs Kidneys- renal regulation changes thickness of blood Chemicals Elasticity of vessels- allows them to expand/contract as blood pressure changes Pumping action of heart- heart pumps 5.6 L of blood/min Size of blood vessels- smaller the vessel, the higher the pressure forcing the blood through Amount of blood present- loss of blood lowers pressure Thickness of blood- thicker blood has more pressure How fast does blood move? 10 inches/sec through the aorta but in capillaries it can drop to 1/100th inch/sec & then it speeds up some in the veins Valves in veins & the massaging of veins by skeletal muscles that keep blood flowing back to heart Cardiac muscle Myogenic- doesn’t rely on nervous system for stimulation Self-stimulating- first cell is stimulated & it excites neighboring cells Pace is set by SA (sinoatrial) node in wall of right atrium near superior vena cava If left to itself, SA node would make heart beat 100 times/min but it is controlled by the sympathetic/parasympathetic nervous system Beating of the heart SA node initiates an impulse about once a second; this depolarization wave spreads across the atria at 800-1000 cm/sec This wave is immediately followed by a wave of muscle contraction that pushes blood out of atria AV (atrioventricular) node is at base of right atria near heart’s center septum SA node depolarization triggers depolarization through heart septum to Bundle of His (30-50 cm/sec speed); Relays conduction of stimulus from atria to ventricles As we age, AV node may slow down & it may be necessary to get an artificial pacemaker Bundle of His divides into left/right bundle branches that travel down septum At heart apex the branches become Purkinjie fibers that radiate upward along inside walls of ventricles; this depolarization occurs very quickly (5000 cm/sec); this contraction pushes blood up/out of ventricles How is your heart controlled? Sympathetic NS- increases heart rate; center for this lies in medulla oblongata in the cardioaccelerator center Parasympathetic NS- decreases heart rate; center in medulla oblongata in the cardioinhibitor center These activities are determined by the nature of impulses reaching centers from cerebrum (ex. Watching scary movie makes heart beat faster), impulses reaching centers from aorta/carotid arteries (ex. Increase in pressure decreases heart rate), & chemical composition of blood flowing through medulla oblongata (ex. Oxygen decreases or carbon dioxide increases will cause heart rate to increase), age, gender, body temperature, postural changes, emotions, activity level Other control factors Nervous impulses to vessels Vasoconstriction- brain keeps arteries in slight contraction Vasodilation- brain relaxes muscle fibers in vessels Drugs Epinephrine- heart rate & blood pressure increase for a short time Acetylcholine- acts as a relaxing agent to dilate vessels Histamine- dilates arterioles/capillaries if in excess Alcohol- vasodilator/depressant Nicotine- vasoconstrictor/stimulant Ephedrine- constricts vessels locally Hematocrit Ratio of blood cells to total volume of whole blood Adult males 46% Adult females 42% If it drops below 30% person is anemic since there are too few RBC Buffy layer in middle is WBC/platelets How does exchange take place between tissues/blood? Capillary walls are one cell thick so small molecules are freely permeable & larger molecules must be moved other ways (diffusion/filtration) Diffusion occurs because there is a concentration gradient Movement goes from area of high concentration to area of lower concentration Filtration occurs due to pressure differences between blood/osmotic pressure Movement goes from area of high pressure to area of lower pressure Hemostasis Body’s effort to minimize amount of blood lost by body through wound Methods of hemostasis Vasoconstriction (vascular spasm)- happens immediately upon injury to blood vessels Smooth muscle tissue of vessel constricts to reduce blood flow Platelet plug formation- when injury to vessel wall occurs collagen fibers in connective tissue become directly exposed to blood; platelets catch on these fibers & to surfaces coated with von Willebrand factor; platelets release secretory granules that contain ADP/vasoconstrictors; as more platelets gather a platelet plug is formed to seal the wound temporarily Coagulation- most important mechanism Blood changes from fluid to solid to form long-lasting seal for wound (scab) Fibrin threads support the platelet plug & trap RBC/WBC to increase size of plug Fibrin threads formed from fibrinogen plasma proteins through a series of chemical reactions Step 1- thrombin protein alters the fibrinogen molecule to form fibrin monomer Step 2- monomers link together to form polymer Step 3- polymerized monomers cross link to form a stable fibrin clot Normally fibrinogen has a concentration of 200 mg/mL blood Blood types Blood carries proteins called antigens which stimulate the production of antibodies Blood classification (A-B-O) is based on antigens found on RBC surfaces RBC can carry A antigen, B antigen, both or neither to produce blood types A, B, AB, & O Genes IA, IB or i Type A makes anti-B antibodies, Type B makes anti-A antibodies, Type O makes both anti-A & anti-B antibodies but Type AB makes neither When A blood is added to B blood, B antibodies attack foreign A antigens causing blood to clump together so transfusion recipients must receive blood that is compatible to theirs If transfusions do not match, then antigens make antibodies to attach foreign blood & blood clumps O is universal donor & AB is universal recipient Rh factor is another blood antigen If Rh+ blood is added to Rh- blood, antibodies will react with antigen & clumping will occur Rh incompatibilities during pregnancy (- mother + father) If first child is +, mother will react to second child & fetus may die if medication (Rhogam) is not given at first birth There are other types of blood antigens that aren’t as commonly known but still important in transfusions/transplants Some Disorders of Circulatory System Anemia Lack of hemoglobin (therefore fewer RBC) in blood which corresponds with a lower oxygen supply Most common type is iron-deficiencty anemia Aplastic anemia due to destruction of bone marrow such as in radiation therapy Pernicious anemia due to lack of vitamin B-12 Symptoms: fatigue, weakness, pale color Treatment: iron supplements Sickle cell anemia Genetic defect more common in African-Americans Sickling of RBC produced by lack of oxygen such as when traveling at high altitudes or exercising vigorously Hypertension (high blood pressure) ~20% of adults have this 140/90 is considered high Blood is forced through capillaries too fast for sufficient exchange of nutrients/waste Risk factors: heredity, male gender, obesity, high salt diets, alcohol use, smoking, inactivity, over age 35, stress Complications: damage to kidneys, weakened blood vessels, blindness, heart disease Treatments: lifestyle changes, medication (sympathetic nerve blockers, calcium channel blockers, ACE inhibitors), vitamin C may help Arteriosclerosis (hardening of arteries) Lining of arteries become thickened/roughened due to deposits of cholesterol, proteins & calcium Makes it easier for clots to become lodged since vessels are smaller Cholesterol- 2 types (low density & high density lipoproteins) LDL creates harmful deposits HDL may help block accumulation of LDL on walls; takes cholesterol from blood & returns it back to liver to be flushed from body Total blood cholesterol increases with age but HDL part remains fairly constant Exercise may increase LDL Varicose veins Cause chronically swollen legs & skin ulcers Swollen twisted veins at surface of skin look like bumpy blue ropes Valves have failed & blood is pooling in veins May be hereditary Symptoms: aching tired legs, itchiness, leg cramps/tenderness, stabbing pain Self helps: wear loose fitting clothing, elevate legs, don’t sit/stand too long, exercise regularly, lose excess weight, eat high fiber diet, avoid high heels/support hose Heart attack (myocardial infarction) Death to section of heart muscle due to blockage of blood supply possibly caused by blood clot (thrombosis) in coronary artery or fatty deposits 75% occur after age 65 Risks: smoking, excess weight, high blood pressure, lack of exercise, family history, age, gender (males) Symptoms: heavy chest pain, tightness, pain in jaw/shoulder/arm/neck, pain like severe heartburn, sweating, nausea, women tend to also feel short of breath Treatment: bypass surgery where healthy veins are transplanted to heart to increase blood flow Women are twice as likely to die within a few weeks Aspirin may reduce risk of having first heart attack in men by keeping blood thinner & from forming clots Stroke (brain attack) 3rd leading cause of death Blockage of blood supply to brain due to clot or bulge in blood vessel that bursts Some cause loss of speech, memory or paralysis but can be severe enough to cause immediate death Symptoms: sudden weakness or numbness to one side of body, sudden loss of vision, loss of speech or understanding, sudden severe headache, unexplained dizziness Prevention: reduce high blood pressure, reduce stress, dietary changes Hemophilia Sex linked inherited condition caused by recessive allele More common in males Blood in person fails to clot or clots very slowly after injury Once treated with blood transfusions but now there are blood factor treatments Heart murmur- result of defective heart valves that do not close completely so blood squirts back into chamber it just left Mononucleosis Symptoms: low energy, chronic sore throat, low grade fever, tired/achy feeling, enlarged spleen