advances/Advances in Pediatric Ophthalmology Research
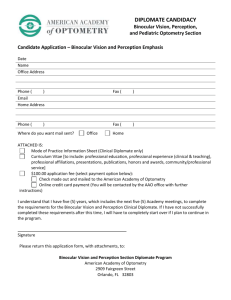
advertisement

The Sigvard & Marianne Bernadotte Research Foundation for Children Eye Care was founded in January 1990 by Princess Marianne Bernadotte and the late Prince Sigvard Bernadotte. The aim of the Foundation is to support pediatric ophthalmology research in Sweden, and to create a center for research and advanced eye care for children at Karolinska Institutet in Stockholm. Now, in 2010, the Foundation celebrates its 20th anniversary. This volume, Advances in Pediatric Ophthalmology Research, is a part of the celebration, representing an account of important advances in pediatric ophthalmology in Sweden and internationally. Advances in Pediatric Ophthalmology Research Reports presented in 2010 at the 20th anniversary of the Sigvard & Marianne Bernadotte Research Foundation for Children Eye Care Edited by Gunnar Lennerstrand and Gustaf Öqvist Seimyr Advances in Pediatric Ophthalmology Research Reports presented in 2010 at the 20th anniversary of the Sigvard & Marianne Bernadotte Research Foundation for Children Eye Care Edited by Gunnar Lennerstrand and Gustaf Öqvist Seimyr The research presented in this publication has been supported by the Sigvard & Marianne Bernadotte Research Foundation for Children Eye Care Preface The Sigvard & Marianne Bernadotte Research Foundation for Children´s Eye Care was founded in January 1990 by Princess Marianne Bernadotte and the late Prince Sigvard Bernadotte. The aim of the Foundation is to support pediatric ophthalmology research in Sweden, and to create a center for research and advanced eye care for children at Karolinska Institutet in Stockholm. As the years have passed, the Foundation has become an important contributor to research funding in pediatric ophthalmology. Scientists from all universities of Sweden have been supported in their research projects. The Bernadotte Laboratories for pediatric ophthalmology have been established at St. Erik Eye Hospital in Stockholm. Symposia and other meetings in pediatric ophthalmology have been funded. A named Honorary Lecture for Prince Sigvard has been presented at each Nordic Pediatric Ophthalmology Congress since 1994 by a distinguished researcher of pediatric ophthalmology. A Prize is awarded in the name of Princess Marianne biannually since 1995 to a prominent researcher in clinical pediatric ophthalmology. At its 10th anniversary the Foundation published a résumé of the research it had supported at that time, included in a short handbook of pediatric ophthalmology for laymen and parents. Now, in 2010, the Foundation celebrates its 20th anniversary. This volume is a part of the celebration, representing an account of important advances in pediatric ophthalmology in Sweden and internationally. Marianne Bernadotte Gunnar Lennerstrand Founder Chairman Authors Ann Hellström, Professor. Department of Ophthalmology, University of Gothenburg, Queen Silvia Children’s Hospital, Gothenburg Gerd Holmström, Professor. Department of Clinical Neuroscience. University of Uppsala, Academic Hospital, Uppsala Lena Jacobson, Associate Professor. Department of Clinical Neuroscience, Karolinska Institutet, Astrid Lindgren Children’s Hospital, Stockholm Peter Jakobsson, Associate Professor. Department of Ophthalmology, University of Linköping, University Hospital, Linköping Maria Kugelberg, Associate Professor Department of Clinical Neuroscience, Karolinska Institutet, St. Erik Eye Hospital, Stockholm Gunnar Lennerstrand, Professor em. Department of Clinical Neuroscience, Karolinska Institutet, St. Erik Eye Hospital, Bernadotte Labs, Stockholm Lene Martin, Associate Professor. Department of Clinical Neuroscience, Karolinska Institutet, St. Erik Eye Hospital, Bernadotte Labs, Stockholm Tony Pansell, Assistant Professor Department of Clinical Neuroscience, Karolinska Institutet, Optometry, Bernadotte Labs, Stockholm Agneta Rydberg, Associate Professor. Department of Clinical Neuroscience, Karolinska Institutet, St. Erik Eye Hospital, Bernadotte Labs, Stockholm Kristina Teär Fahnehjelm, Associate Professor. Department of Clinical Neuroscience, Karolinska Institutet, St. Erik Eye Hospital, Bernadotte Labs, Stockholm Jan Ygge, Professor. Department of Clinical Neuroscience, Karolinska Institutet, St. Erik Eye Hospital, Bernadotte Labs, Stockholm Gustaf Öqvist Seimyr, Researcher. Department of Clinical Neuroscience, Karolinska Institutet, St. Erik Eye Hospital, Bernadotte Labs, Stockholm Contents Introduction i The First 20 Years of the Foundation 1 Gunnar Lennerstrand Research reviews I The Development and Assessment of Vision 2 Agneta Rydberg II Development of the Visual Field 3 Lene Martin III Eye Development and Refractive Errors 4 Tony Pansell IV Ocular Motility Development 5 Jan Ygge V Childhood Strabismus 6 Gunnar Lennerstrand VI Visual Screening in Children 7 Peter Jakobsson VII Pediatric Cataract Maria Kugelberg 8 VIII The Impact of Growth and Growth Factors for 9 Vascular and Neural Development in Preterms Ann Hellström IX Prematurity and the Eye 10 Gerd Holmström X Visual Function and Ocular Findings in Children with 11 Pre- and Perinatal Brain Damage Lena Jacobsson XI The Eye Mirroring Inherited Metabolic Disorders 12 Kristina Teär Fahnehjelm XII Vision for Reading Gustaf Öqvist Seimyr 13 i The First 20 Years of the Foundation Gunnar Lennerstrand Introduction The Sigvard & Marianne Bernadotte Research Foundation for Children’s Eye Care was established in January 1990. The founders were Princess Marianne Bernadotte and the late Prince Sigvard Bernadotte. Support for the initial idea of this foundation was supplied by the late artist Sven Inge and by myself. The motto of the foundation is “Vision in the Future”, recognizing that vision, being low at birth can reach normal levels in adulthood only if proper visual stimulation is provided during childhood. Retarded visual development will lead to poor vision throughout life, and early detection of visual dysfunction and early treatment is of greatest importance in order to restore normal vision. The by-laws state that the Foundation should promote good visual health in the child population and support scientific research on vision and eye care of children. A goal of the Foundation, announced already at the first meeting, is to create an institute for research and advanced eye care of children at Karolinska Institutet in Stockholm. In the following a description will be given of how the Foundation has fulfilled these objectives. The members of the board in 1990 were: Professor, Nobel Laureate 1967, Ragnar Granit; Princess Marianne Bernadotte; Professor Gunnar Lennerstrand; Managing director Sven Wallgren; Professor Curt von Euler;Professor Ove Broberger; Dr Theol Bertil Persson; Artist Sven Inge Höglund. The start and the development of funds The first action to bring funds to the foundation was taken by Princess Marianne Bernadotte in arranging an auction at Bukowskis, the most important auction house in Stockholm. Over 200 works of art were solicited and registered in a catalogue with pictures, and already on February 13, 1990, the auction took place. The net result was about 1.2 million SEK for the foundation, a very good start in funding. Through active work of the board members, contacts with the press and with the help of promotion material of various kinds, the foundation quite rapidly became known to the public. Grant applications to other foundations and institutions were relatively successful and increased the funds. A large donation of 5 million SEK from the Tomteboda School in 1991 constituted a major advance of funds and made it possible for the foundation to start to support pediatric ophthalmology in 1992 with grants for research and travel. Donations of varying amounts have been made to the foundation during the years, the most remarkable being donations at separate occasions, amounting to 50 million SEK, by the late Birgit and Gösta Törnlöf . The list of donations of 50 000 SEK or more is as follows: 1994 Stiftelsen Frimurare Barnhuset i Stockholm Fondation Harari, Paris; 1995 Essilor, Paris Pharmacia Sigvard och Marianne Bernadottes Vänförening 1998 Victor J.B. Pastor, Monaco; 1999 Fondation Oussemi, Genève; 2000 Redaktör, med dr h c, Maj Ödman; 2001 Sven-Ivar Marthín, Vilhelmina; 2002 Department of Ophthalmology, Huddinge University Hospital; 2004 Michel Francois-Poncet Magda & Enrico Bragiotti Kay & Lyndon L. Olson jr.; 2005 Birgit & Gösta Törnlöf; 2009 Anders Tengbom In addition to donations, the funds have increased by successful investments in stocks and other financial instruments, according to a placement strategy worked out in collaboration with the SE bank, handling the accounts of the foundation. The development of funds is shown in figure 1. At present the total value of funds is about 65 million SEK. Development of funds 80 000 70 000 SEK x 1000 60 000 50 000 40 000 30 000 20 000 10 000 19 91 19 92 19 93 19 94 19 95 19 96 19 97 19 98 19 99 20 00 20 01 20 02 20 03 20 04 20 05 20 06 20 07 20 08 20 09 0 Year Figure 1. Development of funds of the Foundation since 1991. Funding of research Research projects in pediatric ophthalmology have been funded yearly since 1992. Applications are solicited for presentation before May 1 and the applications are evaluated by the Scientific committee and presented to the board for decision at the annual meeting in June. Support has been given in the form of scholarships for travel and for research, grants to individual researchers or to the Bernadotte laboratories (see below). The amount of support supplied since 1992 is approximately 10 million SEK, with a marked increase in 2008 and 2009, as shown in figure 2. In addition to the fields of pediatric ophthalmology represented in the review chapters in this book, research has been supported also on retinal development, retinal dystrophies, retinal neovascularisation, visual evoked potentials, fetal alcohol syndrome, congenital glaucoma, ocular allergy, genetics of eye diseases, and visual handicap in children. The recipients of the research grants and scholarships are scientists from all of the medical schools in Sweden. Mainly the younger scientists have been supported and of 77 researchers being funded, 57 were in the beginning of their scientific carrier, most of them Ph.D. students. Of these young scientists 48 have finished their Ph. D. degree and 3 their Master degree, i.e. about 90% of them have graduated. The financial support given to them by the foundation would seem very well invested. A broad basis has been laid for future and expanding research in pediatric ophthalmology. The other funded scientists have been already established researchers. The distribution between the Swedish medical schools of the scientists being funded is as follows: Stockholm 44, Gothenburg 16, Uppsala 8, Lund 3, Linköping 2 and Umeå 1. The distribution reflects the number of scientists active in pediatric ophthalmology at the different universities, Karolinska Institutet in Stockholm having the largest number in the country. Amount of grants awarded 2 000 1 800 1 600 SEK x 1000 1 400 1 200 1 000 800 600 400 200 19 92 19 93 19 94 19 95 19 96 19 97 19 98 19 99 20 00 20 01 20 02 20 03 20 04 20 05 20 06 20 07 20 08 20 09 0 Year Figure 2. The amount of grants awarded by the Foundation since 1992. The Prince Sigvard honorary lecture In 1992 the board decided to institute an honorary lecture in the name of Prince Sigvard to acknowledge the accomplishments of a prominent esearcher in the Nordic countries. Nominations are done by the board of the Nordic Pediatric Ophthalmology Association and presented to the board of the foundation for evaluation and decision. The award is presented at the Nordic Pediatric Ophthalmology meetings and the recipient gives a lecture. The list of awardees at the different meetings is as follows: 1994 Helsinki – Mette Warburg, Köpenhamn 1996 Copenhagen – Göran Stigmar, Lund 1999 Lugarvatn, Iceland – Hans Fledelius, Köpenhamn 2001 Tromsö – Kerstin Strömland, Göteborg 2003 Uppsala – Heikki Erkillä, Helsingfors; 2005 Åbo – Ruth Riise, Hamar 2007 Helsingör - Olav Haugen, Bergen; 2009 Bergen – Gerd Holmström, Uppsala The Princess Marianne price In 1994 the board of the foundation decided to create a price in the name of Princess Marianne Bernadotte to be presented to a prominent Swedish clinical researcher still in the active phase of their carrier. Nominations for the price are supplied by the professors of ophthalmology in Sweden, for dicision by the board of the foundation. The price sum has been 50 000 SEK. At the price ceremony the awardee presents a price lecture, and the ceremony finishes with a musical event. The list of price awardees is as follows: 1995 Kerstin Strömland, Göteborg 1997 Kristina Tornqvist, Lund 1999 Jan Ygge, Stockholm 2002 Lena Jacobson, Stockholm 2004 Gerd Holmström, Uppsala 2006 Ann Hellström, Göteborg 2008 Peter Jakobsson, Linköping The Bernadotte Laboratories for Pediatric Ophthalmology The research in pediatric ophthalmology has been strong at the department of ophthalmology at Karolinska Institutet, particularly from the 1980-ies and onwards. The foundation has supported this research and the laboratories at the department from the beginning. When the laboratories were offered a new location at Huddinge University Hospital, they were officially announced as the Bernadotte Laboratories of Pediatric Ophthalmology and inaugurated by Prince Sigvard in March of 2000. The laboratories moved to the St. Erik Eye Hospital in March of 2002. In the laboratories about 20 researchers at different levels are active in studies of normal and abnormal development of the visual and oculomotor system, strabismus, dyslexia, pediatric neuro-ophthalmology, ocular manifestations in pediatric diseases, among others. Teaching of pediatric ophthalmology for different categories of students and personnel is a prominent part of activities at the Bernadotte laboratories. The Laboratories are an important part of the newly created Bernadotte Institute at Karolinska Institutet for research and advanced eye care of children. This institute is a virtual one, combining research at the Bernadotte Laboratories with clinical work at St. Erik Eye Hospital and Astrid Lindgen Hospital for Pediatrics. Support for the institute from the foundation is directed to the Bernadotte Laboratories and to the hospitals through contracts between the foundation and the hospitals. The support includes scholarships and salaries for researchers at the hospitals and the laboratories, and funds for rent and equipment at the laboratories. Collaboration with other foundations The Bernadotte Foundation for Children’s Eyecare, Inc. was started 1993 in New York at the initiative of Princess Marianne Bernadotte and with support from business men and scientists with a Swedish background. Funds have been collected through auctions of donated art work and/or charity banquets. Such events have been held in New York 1994, Chicago 1997, Los Angeles 1999 and Palm Beach 2001, 2003 and 2005. The Foundation has supported three visiting researchers to the Bernadotte Laboratories in Stockholm, and researchers and doctors from developing countries to attend internal conferences of pediatric ophthalmology. An association called The Friends of Sigvard and Marianne Bernadotte was started in 1997. The members of the association want to support the Bernadotte foundations of Art and of Pediatric Ophthalmology. The association arranges cultural activities for the members. The association donates the assets collected each year to the two foundations. The members of the present board of trustees Professor, Nobel laureate 1981, Torsten Wiesel (honorary chairman); Princess Dr med h c Marianne Bernadotte; Professor Gunnar Lennerstrand (chairman); Managing director Sven Wallgren (vice chairman); Professor Anders Persson (secretary); Director Gunilla Stenberg Stuckey; Professor Jan Ygge; BM Christina Lagergren; University secretary Ulla-Britt Schützler- Peterson. Figure 3. The present board of trustees. Prince Sigvard and Princess Marianne Bernadotte Organizers of the charity auction at Bukowskis in February 1990. From left: Attorney Kerstin Sandels, Princess Marianne, mrs Gun Lennerstrand and professor Gunnar Lennerstrand From the charity auction at Bukowskis in 1990. Pediatric ophthalmology research among the art pieces was presented by Gunnar Lennerstrand and Jan Ygge From the festivities at Waldermarsudde in 1991 when the Foundation received a large donation from the Tomteboda School, represented by director Gunilla Stenberg Stuckey Princess Marianne´s Prize presented to professor Lena Jacobson at a ceremony in the Swedish Medical Association Exterior and interior of the Bernadotte Laboratories at St. Erik Eye Hospital Vision and eye motility research being performed using a Tobii eye tracker. Professor Jan Ygge and test subject I The Development and Assessment of Vision Agneta Rydberg Introduction The normal visual development occurs from birth up to the age of 10-12 years, and requires a normal visual system. Research during the last decades has emphasized the importance of adequate visual stimulation during the first months and years of life. It is therefore of great importance to identify children with subnormal vision early in life to start treatment and habilitation. A prerequisite is that reliable testing methods are available and can reveal visual defects as early as possible. The visual acuity testing methods in children can be divided into 3 subgroups according to the types of stimulus used; detection, resolution and recognition acuity. Different acuity values are usually obtained with the different tests. Contrast sensitivity measurements can reveal changes and loss of visual function that is not detected when testing visual acuity. Sweep-VEP could become a valuable test to assess vision in young children in a clinical setting. Normal visual development What can a newborn child see and how does the vision develop? A newborn child can hear quite well, but the vision is subnormal and has not developed much. A newborn baby can fixate a light, and from birth up to 4 weeks the baby starts to fixate and follow objects presented closer than 1 meter. At about 2-3 months the child can fixate and follow an object at 2-3 meters. Eye contact is usually said to be developed at 4-7 weeks, and at 8-12 weeks the child starts to play with its own fingers in front of the eyes. The visual acuity, recorded as Snellen decimal acuity, is approximately 0.01-0.05 in a newborn child, 0.1 at 6-12 months, 0.25 at 2 years, 0.5-0.65 at 3 years, 0.8 at 4 years and 1.0 at 6 years. Not until the age of 10 -12 years the visual acuity is fully developed, approximately 1.3-1.6. However, the acuity values depend to a great extent on the methods used in the examination and this issue will be discussed in more detail later in this chapter. Development of the visual pathways The subnormal vision in young children is due to the immaturity of the eye and the whole visual system-the retina, optic nerve, chiasma, lateral geniculate body, optical radiation, and visual cortex. At birth the axial length of the human eye is about 17 mm (or 3/4 of adult size), and by 13 years of age the eye has reached adult size, and an axial length of 23 mm. The fovea is immature at birth. In the fetal eye cup it appears as an elevation formed by the ganglion cells. The ganglion cells migrate peripherally during the first 25 weeks of fetal life to form the foveal pit. The retina and especially the fovea will reach full maturity at about 4 years of age. The main change is in the density and spread of cones in the retina during this period. The myelination of the optic nerves begins in the lateral geniculate nucleus, reaches the orbital part of the optic nerve at full term, and continues towards the retina over the following 2 years. The maturity of the lateral geniculate body and the visual cortex also take place during the first 4 years of life. Studies of vision in monkeys, with a visual system very similar to that of the human, have shown that the visual acuity during the first years is much lower than what could be expected from the structure of the retinal and the neuronal elements. However, at higher ages it correlates quite well to morphological parameters. The development of the still higher visual acuity in adulthood is mainly due to the maturity of the higher visual systems in the brain beyond the visual cortex. The sensitive period The plastic period (also called the sensitive period or the critical period) of the visual development is the time during which the visual acuity is developing and can be modified. The Nobel laureates of 1981, Professor Torsten Wiesel (honorary president of the Sigvard and Marianne Bernadotte Research Foundation for Children Eye Care) and professor David Hubel, already in 1963 established the norms for the sensitive period in cats and monkeys. The period for cats is up to 16 weeks and in monkeys up to 30 weeks. In the human the sensitive period proceeds up to 8-10 years of age with the most critical part during the first 23 months. Abnormal visual development The normal visual development requires a normal visual system. Different eye diseases such as congenital cataract, strabismus, refractive errors (especially astigmatism and high hyperopia), ptosis, lid hemiangioma etc. will prevent clear vision and retard visual development. Amblyopia (amblyos= lazy, opia= vision) is a common visual sequelae to such eye disorders. It is defined as a unilateral or bilateral decrease of visual acuity caused by pattern vision deprivation or abnormal binocular interaction, where no signs of organic disease can be detected by physical examination of the eye and which in appropriate cases is reversible be therapeutic measures (see also chapter VI). Amblyopia can be successfully treated up to approximately the age of 8 years, provided the obstacle to normal form vision is removed, correct optical correction is provided, and occlusion of the good eye is introduced to train the amblyopic eye. An alternative treatment to occlusion is to use cycloplegic eye drops usually atropine in the good eye, a method that has attracted renewed popularity in the United States, despite the disadvantages with the different side effects. A contact lens to decrease the vision in the good eye can be used if other methods fail. Improved vision in amblyopia with pharmacological treatment such as levodopa and citicoline has also been reported (Leguire et al. 1993, Campos & Fresina 2006). In congenital cataract the opaque crystalline lens should be surgically removed before the age of 2 -3 months to reach good visual results (see also Chapter VI). Methods to assess visual acuity Visual acuity testing in young children in a clinical setting can be divided into three subtypes according to the type of stimulus used. In detection acuity the stimulus, usually white balls in various sizes, should be detected or distinguished from the black background. In resolution acuity, the stimulus pattern, a black and white grating, should be resolved. In recognition acuity the stimulus, a letter or symbol should be recognized by the subject and identified by matching or naming. The psychologist Fantz already in the 60´s reported that infants will prefer to look at a patterned stimulus when presented in a homogeneous field of vision. This behavioural method was called the preferential looking (PL) test. It was further developed by Teller and coworkers (1986) and brought into clinical practice. The test patterns are black and white gratings of variable spatial frequencies presented on printed cards, called the Teller Acuity Cards. We first performed a study in adults to evaluate the method in patients with strabismic amblyopia. It was shown that grating acuity (resolution acuity) overestimates the acuity values determined with recognition tests in patients with strabismic amblyopia (Rydberg 1997). To see how the correlation between the methods were in children, the next study was carried out in children with manifest strabismus, visual impairment due to organic eye diseases and children with normal vision. An overestimation of visual acuity was also seen in these groups of children, when grating acuity was compared with recognition acuity (Fig. 1). Hence, similar results were obtained in the children and adults. Figure 1. PL grating acuities plotted against the HVOT linear test in children with normal vision (circles), visual impairment (triangles) and strabismic amblyopia (squares). Each data point represents one subject, except for a few representing two subjects. The dashed line represents the line of equality between the tests. Logarithmic scales are used on both axes To see whether the PL test could be used as a screening test for amblyopia, the grating acuity in the amblyopic eyes and the non-amblyopic eyes were compared. In 30% of the subjects resolution acuity determined with PL was the same in both eyes, and the amblyopia would consequently have been missed if the PL test had been used in visual assessment (Fig. 2). Figure 2. PL-grating acuities in the amblyopic eyes, plotted against PL acuities in the nonamblyopic eyes, in the adult patients with strabismic amblyopia (n=28). Each point represents one patient. The dashed line represents the line of equality between the tests and the solid line marks the limit for one octave difference between PL-acuity in normal and amblyopic eyes. Linear scales are used on both axes There are some Swedish studies on the development of recognition visual acuity using tests with different kinds of optotypes. Lithander (1997) found a mean visual acuity of 0.48, with the O-test (single symbols for near), in children 24-29 months old. With the KOLT test for linear acuity, a visual acuity level of 0.55 was found in children aged 30-35 months, 0.67 in children of 36-41 months and 0.77 in children 42-48 months old. Rydberg et al. (1998) found a visual acuity of 0.67 with the LH-line test and 0.6 with the HVOT-test in children 29-41 months old and 0.99 with both tests at 48-83 months (median age 51 months). In a study by Larsson et al. (2005), 81.6% of the control subjects had a recognition visual acuity of 1.33 or more at the age of 10 years. The crowding phenomenon Crowding also called “separation difficulty” is the inability to discriminate letters and symbols that are presented closely together, as optotypes in a line. Visual acuity determined with single optotypes is usually much better than line acuity. Crowding phenomenon is present to a small extent in normal eyes of young children. and is common in strabismic amblyopia and also in children with cerebral visual impairment (Pike et al. 1994, Jacobson et al. 1996). Different tests assess different types of visual acuity Different acuity values are often obtained in the same child with the different tests. For example a child with visual impairment can sometimes detect a small pearl of 0.2 cm at a distance of 3 meters. The grating acuity (resolution acuity) can be as high as 15 cycles per degree corresponding to a Snellen visual acuity of 0.5. The recognition acuity with single letters could be 0.3, whereas the recognition acuity with linear optotypes only is 0.1, due to crowding. Detection and grating acuity do not correspond to Snellen acuity, and therefore grating acuity should always be recorded in cycles per degree, and in measuring detection acuity the size of the object and the distance used should always be recorded. The discrepancies between the tests have to be kept in mind so that the acuity values are not misinterpreted. It is important to have reliable methods to detect subnormal vision at an early age to be able to start the treatment and habilitation. However, there are still no tests available to get reliable values when assessing vision in young children. It is not until the age of 3 ½ to 4 when children can be tested with optotypes (symbols and letters) in a line that reliable responses can be obtained (Rydberg et al. 1999). Contrast sensitivity testing Visual acuity represents only one aspect of visual capacity. Acuity is estimated as the smallest stimulus that can be detected at a high contrast level. However, most objects in everyday visual environment are larger than objects used in visual acuity testing and usually appear at a lower contrast. Contrast is defined as the difference in luminance between adjacent areas in a stimulus pattern. In determining the Contrast Sensitivity Function (CSF) gratings, symbols or letters can be used at different spatial frequencies or sizes and at different contrast levels. A bell shaped CSF curve is obtained with a peak of maximum sensitivity at 3-5 cycles per degree (Fig 3). The cut-off spatial frequency is the highest spatial frequency that can be resolved at maximum contrast and also represents the visual acuity value. This value is normally 30-60 cycles per degree. There are many different tests to assess contrast sensitivity. Some tests include patterns of different contrast values but only at one spatial frequency. Other tests use patterns at only one contrast level but with many spatial frequencies (Rydberg et al.1997). For a description of the whole CSF, different spatial frequencies at different contrast sensitivity levels should be tested. The normal contrast sensitivity function in young children is lower than in adults and the function increases with age, as shown in figure 3. Contrast sensitivity measurements may reveal changes and loss of visual function that is not detected when testing visual acuity. Figure 3. CSF for normal adult subjects (thick solid line) and in comparison with CSF for children at different ages (dashed lines) and older subjects (thin solid lines). (From Abrahamsson & Sjöstrand 1992) Sweep- VEP (Visual Evoked Potentials) An electrophysiological method was introduced for objective assessment of vision in children by Norcia & Tyler (1985). In this so called sweep-VEP method, the test patterns are sinusoidal gratings and the visual evoked potentials (VEP) to the pattern stimulation are recorded with surface electrodes placed on the occipital part of the scalp. The spatial frequency of the grating changes gradually in a sweep from 32 to 2 cycles per degree. The pattern is presented in an on-off or a pattern reversal mode, with such a high temporal frequency that a “steady state” response is obtained. The VEP amplitude is plotted against spatial frequency of the stimulus, and the visual acuity value can be extrapolated from the curve. Sweep-VEP could be a suitable method to assess vision in young children. We have tested fifty normal subjects age 6 months-50 years (Rydberg et al. 2008). Sweep-VEP gave mostly reliable results in adults. Good test-retest reliability was obtained in 5 adult patients who were tested twice. In the younger children the results were more variable and sometimes difficult to interpret. One possible explanation is poor fixation of the stimulus pattern. If fixation could be controlled, sweep-VEP could become a valuable test to assess vision in young children in a clinical setting. More research will be performed in this area in the future. Conclusions Reliable visual acuity measurements in children can be obtained at about the age of 3 ½-4 years, when visual acuity can be assessed with a recognition test using letters or symbols in a line. Detection and resolution acuities overestimates the acuity values and different acuity values are usually obtained with the different tests. The existing methods for clinical testing of children under the age of 2 years are limited. Sweep-VEP could become a suitable test to assess vision in young children. References Abrahamson M & Sjöstrand J (1992): Kontrastkänslighet och bländning. Nordisk medicin. 107:316-318. Campos EC & Fresina M (2006): Medical treatment of amblyopia: present state and perspectives. Strabismus, 14:71-73. Jacobson L, Ek U, Fernell E, Flodmark O & Broberger U (1996): Visual impairment in preterm children wih perivenricular leukomalacia-Visual cognitive and neuro-pediatric characteristics related to cerebral imaging. Developmental Medicine and Child Neurology, 38:724-735. Larsson E, Rydberg A & Holmström G (2005): A population-based study of the visual outcome in 10-year-old preterm and full-term children. Archives of Ophthalmology, 123:82532. Leguire LE, Walson PD, Rogers GL, Bremer DL & Mc Gregor ML (1993): Longitudinal study of levodopa/carbidopa for childhood amblyopia. Journal of Pediatric Ophthamology and Strabismus 30:354-60. Lithander J (1997): Visual development in healthy eyes from 2 months to four years of age. Acta Ophthalmologica Scandinavica, 75:275-276. Norcia AM & Tyler CW (1985): Spatial frequency sweep VEP: visual acuity during the first year of life. Vision Research, 25:1399-1408. Pike MG, Holmström G, de Vris LS, Pennock LM, Drew KJ, Sonksen PM & Dubowitz LMS (1994): Patterns of visual impairment associated with lesions of the preterm infant brain. Developmental Medicine and Child Neurology, 36:849-862. Rydberg A (1997): Assessment of visual acuity in adult patients with strabismic amblyopia: A comparison between preferential looking and different acuity charts. Acta Ophthalmologica Scandinavica, 75:611-617. Rydberg A, Han Y & Lennerstrand G (1997): A comparison between different contrast sensitivity tests for the detection of amblyopia. Strabismus, 5:167-184. Rydberg A & Ericson B (1998): Evaluation of methods for assessing visual function in children 1 1/2 years of age with normal and subnormal vision. Journal of Pediatric Ophthalmology and Strabismus, 35:312-319. Rydberg A, Ericson B, Lennerstrand G, Jacobson L, Lindstedt E (1999). Assessment of visual acuity in children aged 1 1/2 - 6 years, with normal vision, visual impairment and strabismus. Strabismus, 7 (1): 1-24. Rydberg A, Bengtsson M & Andersson T (2008): Sweep-VEP, a method to assess vision in children. 32nd Meeting of the European Strabismological Assoociation, Abstract P12:55. Teller DY, Mc Donald MA, Preston K, Sebris SL & Dobson V (1986): Assessment of visual acuity in infants and children. The acuity card procedure. Developmental Medicine and Child Neurology, 28:779-789. II Development of the Visual Field Lene Martin Introduction The visual field is defined as the area that can be seen when the eye is directed forward and steadily fixating, including that which is seen with peripheral vision. The visual field is almost always tested one eye at the time, and there are several methods and more or less advanced equipments for visual field testing (also called perimetry). This chapter describes visual field testing in children and factors influencing the visual field development and the test results. Methods for testing the visual field in children A simple, although quite informative way of testing the extent of the visual field is ad modum Donders, when you use your own hands as stimuli, and your own visual field as reference. This method is used in adults to detect large constrictions and when no equipment is available. For quantitative testing of the sensitivity within the visual field, computer assisted techniques are preferred. Since most of the diseases affecting the visual system first affects in the central part of the visual field (although not necessarily affecting the area for reading ability; the fovea), most computerized perimeters test the central 30° area. In children, however, it is sometimes interesting also to test the extent of the visual field, and then different manual methods, possible to adapt to the children’s age and ability to co-operate, have to be used. In small children, testing the visual field is a challenging task. A number of different methods have been developed but only a few of them have been adequately evaluated. In very young children a variant of “preferential -looking” is used, in which the examiner observes if the infant shifts gaze when a stimulus is presented. In toddlers the so called ball-on-a-stick can be used. Pre-school children are able to co-operate in a manual Goldmann examination and school children can perform computerized perimetry (Fig 1). Figure 1. Different techniques for visual field testing. Goldmann perimetry (Courtesy of Luisa Mayer) (Left), Computerized perimetry: Rarebit perimetry (Right) The Normal Visual Field in Children Measuring the visual field in young children; infants and toddlers, is complicated. Yet, several studies have provided knowledge about the extent of and sensitivity in the visual field in the growing child, even if different reports give somewhat varying results. The extent of the visual field in small children is also depending of the method used; kinetic or static, the size of the stimulus and, in children at 1-2 years of age, also on the presentation of competing stimulus in the fixation area. The effective visual field has been shown to expand between 2 and 4 months of age and the ability to respond to peripheral objects more distant than the fixation object develops after 3 months. Visual field extent corresponding to adult levels has been reported to be present at 17 and 30 months of age, measured with kinetic and static perimetry, respectively (Dobson et al 1998), see figure 2. Figure 2. Visual field extent in different ages measured a with 6° stimulus (Goldmann III – IV). Thin continous blue line = newborn, dashedd blue line = 3.5 months, thick continous blue line = 7 months, red dash/dot line = 4 years, blue dash/dot line = adult (adapted from Dobson et al 1998). Regarding the standard tests, routinely used in adults, it is well known that the child has to reach an age of 5-7 years before reliable visual field results can be expected. Using the most common computerized methods the extent and sensitivity values, equal to those from adults, can be obtained at the age of 10-12 (Martin 2005, Martin & Lundvall 2007; 2009). Attention One main reason for the different results in children and adults, especially regarding static and moving stimuli, may relate to differences in peripheral summation areas or to differences in attention between infants and adults. The visual field in pre-school children is affected by non visual factors, such as vigilance and cognitive processes (Tschopp et al 1998). From the age of 5 to 7, the child is able maintain steady fixation on a target and to respond to a stimulus presented in the periphery by pressing a button. But in younger children and infants, the examiner has to rely on the fixation eye movements of the child. However, infants between approximately 1 and 4 months of age were reported to have difficulty with disengagement, i.e. looking away from a stimulus, once their attention has been engaged (Hunnius 2007). The eccentricity to which infants move their gaze to locate a target has been found to increase rapidly during the first 4 months of age (Harris & MacFarlane, 1974; Lewis & Maurer1992). Despite this fast early development, several studies report that an adult-like performance is not attained before the end of infancy or even the school-age years. Other authors have reported that from the age of approximately 6 months, infants’ performance when shifting gaze between two stimuli is comparable to that of adults (Atkinson et al, 1992). Normal visual field development As has been stated above, there are numerous studies using manual perimetry for examining the visual field in children and for evaluation of the extent of the visual field. We have been interested in evaluating new computerized perimetric methods in children for evaluation the sensitivity of the central visual field, both in healthy children and pediatric patients. Two methods have been used, both developed in Sweden; the high-pass resolution perimeter (HRP (Frisén 1993; Martin et al 2008a) and Rarebit perimetry (Frisén 2002; Martin 2005). Especially the latter was found to be suitable for children of at least 6 year of age. The method is sensitive to low-degree damage, very patient-friendly, requires short examination time and is preferred by the children, when compared to other techniques (Martin et al 2004). Figure 3 shows a summary of five of our studies of healthy children of different ages, evaluating the normal values established with Rarebit perimetry (Martin et al 2004; Martin 2005; Martin & Lundvall 2007; Martin et al et al 2008b; Hellgren et al 2009). Abnormal visual field development There are several factors that can disturb the normal development of the visual field. In several studies we have described the effect of intrauterine incidents, intrauterine growth restriction, premature birth, treatments for side effects of premature birth (retinopathy of prematurity) and other hinders for the normal visual development such as ametropia, strabismus and congenital cataract. Figure 3. Results from computerized perimetry (Rarebit perimetry), expressed as a percentage of stimuli seen (hit rate) from age 7 to 20 (healthy subjects). Note the low increase in hit rate from age 7 to 12 and the somewhat larger variability in examination results in younger children (Martin & Lundvall, submitted). Prematurity and co-morbidity Prematurity influences the visual system in several ways. In a follow-up study of 11-year old children, born prematurely, we could confirm findings in previous studies, i.e. that children treated for retinopathy of prematurity have somewhat constricted visual fields compared to age-matched controls. But we could also show that prematurity per se reduced the sensitivity in the central visual field (outside the fovea), presumably reflecting a reduced density of retino-cortical neural channels (Larsson et al 2004). This was true also for children born small for gestational age due to intrauterine growth restriction (Martin et al 2004). Approximately one third of the children born prematurely and/or with very low birth weight have cerebral sequelae, such as white brain matter damage (Olsén et al. 1997). Studies regarding visual outcome, especially the visual field are sparse, due to the wide-spread misunderstanding that quantitative perimetry is not possible in these children. However, using a combination of the manual kinetic Goldmann perimetry for examination of the extent of the visual field, and one of two computerized techniques for examining the central visual field, we were able to carefully examine a number of prematurely born teenagers and young adults with visual dysfunction due to white matter damage of immaturity of pre- or perinatal origin. They all had subnormal visual field function, although the depth and extension of the defects differed between subjects. Typically, the inferior field function was more impaired than the superior. We could also show that, as in adults, the static computerized techniques revealed a slightly higher frequency of abnormality (Jacobson et al. 2006) compared to Goldmann perimetry. In a separate study of adolescents with very low birth weight (<1500 g) we found that the subjects are at a disadvantage regarding visual outcome compared to subjects with normal birth weight (Hellgren et al 2007). Almost one fifth of all VLBW children, and 40% of those with white matter damage, had subnormal visual fields (Hellgren et al. 2009). Congenital cataract It is well known that dense cataract, even when surgically treated early in infancy, causes persistent impairment of visual acuity. Recently we have shown that not only the extent of the visual field, but also the sensitivity in the 30-degree visual field is affected, although less pronounced than visual acuity (Martin et al. 2008a). This finding has to be taken into account when evaluating visual field results in for example in the diagnosis of glaucoma, a frequent complication after cataract surgery in early infancy. Glaucoma Computerized visual field examinations are gold standard in the diagnosis and follow-up of glaucoma. Nevertheless, not many studies are published using computerized perimetry in pediatric glaucoma. We have found that the Rarebit perimetry is well suited for glaucoma management in children (Martin & Lundvall 2007). Recently we could show that the visual fields remained essentially unchanged during 5 years of follow-up in children and adolescents, carefully treated for glaucoma (Martin & Lundvall 2009). Conclusions Visual fields develop rapidly during early infancy as shown in studies with tests appropriate for the age of the child. However, conventional perimetric techniques are less suitable for children below the age of 7 to 12 years. Recent developments in perimetric methods may improve the ability to detect visual field abnormalities in even younger children. References Atkinson J, Hood B, Wattam-Bell J, Braddick O (1992): Changes in infants' ability to switch visual attention in the first three months of life. Perception. 21(5):643-53 Dobson V, Brown AM, Harvey EM, Narter DB (1998): Visual field extent in children 3.5-30 months of age tested with a double-arc LED perimeter. Vision Res 38:2743-60 Frisén L (1993): High-pass resolution perimetry: a clinical review. Doc Ophthalmol. 83:1–25 Frisén L (2002): New, sensitive window on abnormal spatial vision: rarebit probing. Vision Res 42:1931-1939 Harris P & MacFarlane A (1974): The growth of the effective visual field from birth to seven weeks. J Exp Child Psychol. Oct;18(2):340-8 Hellgren K, Hellström A, Jacobson L, Flodmark O, Wadsby M, Martin L (2007): Visual and cerebral sequelae of very low birth weight in adolescents. Arch Dis Child Fetal Neonatal Ed 92:F259-64 Hellgren K, Hellström A, Martin L (2009): Visual fields and optic disc morphology in very low birth weight adolescents examined with magnetic resonance imaging of the brain. Acta Ophthalmol 87:843-8 Hunnius S (2007). The early development of visual attention and its implications for social and cognitive development.C. von Hofsten & K. Rosander (Eds.) Progress in Brain Research, Vol. 164. 007 Elsevier B.V. Jacobson L, Flodmark O, Martin L (2006): Visual field Defects in Prematurely Born Patients with Periventricular White Matter Damage - a Multiple Case Study Acta Ophthalmol Scand 84:357-362 Larsson E, Martin L, Holmström G (2004): Peripheral and central visual fields in 11-year-old children who had been born prematurely and at term. J Pediatr Ophthalmol Strabismus 41:3945 Lewis TL, Maurer D (1992): The development of the temporal and nasal visual fields during infancy. Vision Res. May;32(5):903-11 Martin L, Ley D, Marsal K, Hellström A (2004): Visual function in young adults following intrauterine growth restriction. J Pediatr Ophthalmol Strabismus 41:212-8 Martin L (2005): Rarebit and frequency-doubling technology perimetry in children and young adults. Acta Ophthalmol Scand 83:670-677 Martin L & Lundvall Nilsson A (2007): Rarebit Perimetry and Optic Disk Topography in Paediatric Glaucoma. J Pediatr Ophthalmol Strabismus 44:223-31 Martin L, Magnusson G, Popovic Z, Sjöstrand J (2008a): Resolution visual fields in children surgically treated for bilateral congenital cataract. Invest Ophthalmol Vis Sci 49:3730-3 Martin L, Aring E, Landgren M, Hellström A, Andersson Grönlund M (2008b): Visual fields in children with attention-deficit/hyperactivity disorder before and after treatment with stimulants. Acta Ophthalmol Scand 86:259-64 Martin L & Lundvall A (2010): Rarebit Visual Field Follow-Up in Pediatric Glaucoma (submitted for publication) Olsén P, Pääkkö E, Vainionpää L, Pyhtinen J & Järvelin M-R (1997): Magnetic resonance imaging of periventricular leukomalacia and its clinical correlation in children. Ann Neurol 41:754-61 Tschopp C, Safran AB, Viviani P, Reicherts M, Bullinger A, Mermoud C (1998): Automated visual field examination in children aged 5-8 years. Part II: Normative values. Vision Res 38:2211-8 III Eye Development and Refractive Errors Tony Pansell Introduction The emmetropization process involves monitoring the ocular growth to match the refractive power of the eye. Myopia occurs when the ocular axial length exceeds the value corresponding to the refractive power of the eye. This chapter will report the current understanding of the emmetropization process and present recent findings of myopia research. Eye development and emmetropization The ocular refractive status refers to the locus of the optical focus in relation to the retina during minimal accommodation. In the ideal eye the distance from the cornea to the retina (i.e. axial length) are in concordance with the total refractive power and the light entering the eye will form a sharp image on the retina, that is an emmetropic eye. In a hyperopic eye the light is focused behind the retina which is due to a too low refractive power alternative a too short axial length. In a myopic eye the light is focused in front of the retina, which can be due to either a too high refractive power alternative a too long axial length. The axial length of the eye ball in an adult is approximately 24 mm and to focus the light onto the retina the optical power has to measure approximately 60 dioptres. The refractive elements of the eye are the corneal surface, which accounts for approximately 42 diopters of the total refractive power and the crystalline lens, which accounts for approximately 18 diopters. In a newborn full term child the axial length is shorter (~17 mm) and the refractive power higher (~85 dioptres). The cornea counts for ~50 diopters and the crystalline lens 35 diopters. The eye bulb reaches almost full axial length at 3 years of age but the ocular growth does not cease until 14-15 years of age. The eye thus only grows approximately 1 mm from 3 years of age to early teenage. When growing, the relation between ocular axial length and ocular refractive power has to be adjusted simultaneously to maintain a well working optical system. This mechanism is referred to as the emmetropization process. Emmetropization regulates the shape of the refractive media, by detecting the refractive error of the eye at rest and initiating ocular changes to minimize the refractive error. In experimentally induced focusing errors by means of positive or negative lenses, the net result of the initiated ocular changes was that the eyes become approximately emmetropic with the lenses in place (Schaeffel et al. 1988). When the lenses were removed, the eyes showed a refractive error in the opposite direction, hyperopic after imposed myopia and myopic after imposed hyperopia. After removing form deprivation filters in chick eyes, the myopia quickly decreased to negligible levels, provided that optical correction was not introduced and that the treatment was initiated at a sufficiently early age (Wallman & Adams 1987). When inducing monocular deprivation in animals the occluded eye ball became longer than normal. The difference in length was over 1 mm and the sclera of the on the posterior wall of the occluded eye was thinner. This effect was found to be largest on younger animals (Wiesel & Raviola 1977). Even a modest degree of constant form-deprivation using partially occluding filters would trigger an axial length growth inducing myopia. The denser the filter is the larger the myopia became (Smith & Hung 2000). The fovea is not essential for normal refractive development as foveal ablations has no apparent effect on emmetropization. However, the peripheral retina, in isolation, can regulate emmetropizing responses and produce anomalous refractive errors (Smith et al. 2007). Hyperopia is more common than myopia in early infancy, and most individuals undergo emmetropization to a refractive state of low hyperopia rather than precise emmetropia (Irving et al. 1996). A few are born myopic and this has to be reversed before reaching young adulthood because the eye ball can grow, but it can not shrink. Current research in myopia While hyperopia is considered relatively harmless, myopia is clearly linked to eye health hazards. Myopia is considered to be the leading cause of visual impairment (World Health Organization, 2000). Immense effort is put into understanding the underlying mechanisms of myopia progression and the biological, neurophysiological and environmental bases for myopia development. The goal is to find predictors to show who will develop myopia and to begin prophylactic treatment in them to minimize or hinder its progression. The prevalence of myopia is increasing globally and myopia has reached epidemic proportions in parts of East Asia with up to 70% to 90% of 17- to 18-year-olds in the region affected (Lin et al., 2001; Saw et al., 2005; Zhao et al., 2000). A Swedish prevalence study in 12-13 year old school children from 2000 showed myopia in 49.7% (Villarreal et al. 2000). Previous prevalence studies in Scandinavia revealed considerably lower values for myopia. In Denmark, 1983, Fledelius reported a prevalence of 30% myopia in individuals 16 years of age and older (Fledelius 1983). In Finland, 1980, Laatikainen found a prevalence of 29% in the 14- to 15-year-olds (Laatikainen & Erkkilä 1980). During the last decade the understanding in the mechanisms of myopia development have increased through ocular biometry, i.e. measurements of the intraocular parameters affecting the refractive state of the eye. From the CLEERE multicentre study in US it seems clear that both early-onset myopia (childhood) and late-onset myopia (15-18 y) typically involve excessive enlargement of the eye where the axial length is prolonged in the absence of compensatory lens changes (see table 1 below for details). Table 1. Summary of the main findings of the Collaborative Longitudinal Evaluation of Ethnicity and Refractive Error (CLEERE) study, a US multicentre 6-year study on normal ocular growth in 2583 children aged 6-14 years (Zadnik et al., 2003) Parameter Aged 6 years Aged 14 years Spherical equivalent refractive error (D) +0.85 ± 0.86 -0.28 ± 2.48 Corneal power (D) 43.67 ± 1.48 43.37 ± 2.48 Anterior chamber depth (mm) 3.54 ± 0.25 3.66 ± 0.29 Vitreous chamber depth (mm) 15.50 ± 0.61 16.44 ± 1.19 Crystalline lens power (D) 24.23 ± 2.16 22.38 ± 2.09 Myopic eyes are larger in all three dimensions (i.e. equatorial, anterior-posterior, and vertical axes). Twin and family studies indicate a genetic predisposition to myopia (Goss & Wickham 1995) and a parental history of myopia is well known to be a high risk factor for developing myopia. The prevalence with two myopic parents is 30% to 40%, whereas it is reduced to 20% to 25% in children with one myopic parent, and to >10% with no myopic parent (Mutti et al. 1996). Anterior and vitreous chamber depths are larger as the risk (the number of myopic parents) of myopia increases. Although the eye growth ceases at around 15 years of age, between 8 and 15 % of the myopes develop their myopia between 15 and 18 years of age (i.e. late-onset myopia) with slow progression to levels rarely exceeding 2 D. The environmental risk factors most often cited include education, urbanization and near work but the nature of their interaction with genetic factors remains unclear (Saw 2003). Late-onset myopia has been attributed to near work, especially when the work has a high level of cognitive demand. The influence of electronic displays on myopia progression is still not clear and a better understanding of the interaction of accommodation and the oculomotor system to these displays need to be consolidated, especially as a new generation of 3D displays is forthcoming. Interestingly, sustained accommodation has been shown to reduce intraocular pressure by up to 2.4 mm/Hg and there is recent evidence for a relationship between IOP and myopia in a Japanese population. Refractive errors in prematurely born children Low birth weight is one factor influencing the refractive development. Premature infants are more prone to develop myopia from an early age and myopia development can continue up to 2 years of age. The incidence of myopia in preterm infants ranges from 1% to 16% and the children may remain myopic later on in childhood and adolescence. Retinopathy of prematurity (ROP) is a disease affecting prematurely born infants due to an immature eye and incomplete development of the retinal blood vessels. The incidence of ROP among prematurely born infants is approximately 40% (Holmström et al. 1993). If mild ROP is present the incidence of myopia increases to 17% to 50%. The more severe the ROP is the higher the incidence of myopia became. Some populations show up to 100% incidence of myopia in the advance stages of the disease. The biometric components found to contribute to the refractive error in prematurely born children include a shallower anterior chamber and a shorter axial length (15 mm), increased lens power (45 D) and increased corneal refractive power (54 D). The mechanism of myopia development thus seems different from that in full term children. The available treatment options for ROP are cryo therapy and laser treatment and it is very difficult to differentiate the effects of the disease and the effect of the treatment on myopia. Treated infants have a higher incidence of myopia than non-treated infants. At the same time, the more advanced stages of ROP are more likely to need more treatment. Research on myopia prevention Today the best single predictor for developing myopia is cycloplegic refraction. Children with hyperopia of 0.75 D or less at a mean age of 8.6 years have been shown to have a sensitivity of 86.7 % and specificity of 73.3 % for developing myopia (Zadnik et al.1999). The question is how refractive errors should be treated while the eye still is growing. There is unfortunately no straightforward answer on that question. The clinical tradition recommends undercorrecting myopia and fully correcting hyperopia in children before entering puberty. The philosophy is to reduce the accommodative demand in order to not induce transient myopia and in the long run manifest myopia. One theory of myopia progression is based on the observation that myopic children have a higher lag of accommodation than non-myopic children. The hyperopic retinal blur that results from a high lag of accommodation during near work is hypothesized to cause an increased rate of axial length growth. However, several studies could not find any change in axial growth when prescribing near reading addition, which minimizes or eliminates the lag of accommodation. The CLEERE study suggests that high accommodative lag is a by-product of myopia, rather than the causative factor. Pharmacological treatment by Pirenzepine, a muscarinic receptor antagonist, shows promising results in reducing the myopia progression. In a recent US study a significant 0.27 D reduction in myopia progression was found after the first year of treatment and a 0.41 D overall reduction after the second year (Siatkowski et al. 2004). Development of new pharmacological agents for controlling scleral growth is today a topic for discussion. This is an exciting and hopefully promising treatment option for the future. Several challenges for myopia research society still exist. The current treatment options are more based on a clinical experience than scientifically proven evidence. The majority of myopia research performed is based on animal studies. Human research is required to fully understand the interaction of genetic and environmental risk factors for developing myopia. Further, better tools for measuring near work exposure are required in order to fully understand the effect of near work on myopia. Conclusions A clear optical image is of main importance for a normal ocular development. The emmetropization process regulates ocular growth and is based on defocus of the peripheral image on the retina. Neural mechanisms involving the fovea or the visual cortex do not seem to be take part in the process. Myopia due to excessive axial length of the eye has increased globally and has become a major concern with regard to ocular health. Great efforts have been made in trying to understand the mechanisms of ocular growth and how to retard myopia progression. References Fledelius HC (1983): Is myopia getting more frequent? A cross-sectional study of 14-16 Danes aged 16 years+. Acta Ophthalmologica 61: 545-559. Goss DA & Wickham MG (1995): Retinal-image mediated ocular growth as a mechanism for juvenile onset myopia and for emmetropization. A literature review. Documenta Ophthalmologica Advances in Ophthalmology 90: 341-375. Holmström G, el Azazi M, Jacobson L &Lennerstrand G (1993): A population based, prospective study of the development of ROP in prematurely born children in the Stockholm area of Sweden. British Journal of Ophthalmol 77: 417-423 Irving EL, Sivak JG, Curry TA & Callender MG (1996): Chick eye optics: zero to fourteen days. J Comperative Physiololgy and Sensory Neural Behaviour Physiology 179: 185-194. Laatikainen L & Erkkilä H (1980): Refractive errors and other ocular findings in school children. Acta Ophthalmologica Scandinavica 58: 129-136. Lin LL, Shih YF, Hsiao CK, Chen CJ, Lee LA & Hung PT (2001): Epidemiologic study of the prevalence and severity of myopia among schoolchildren in Taiwan in 2000. Journal of the Formosan Medical Association 100: 684-691. Mutti DO, Zadnik K & Adams AJ (1996): Myopia: The nature versus nurture debate goes on. Investative Ophthalmology & Visual Sciences 37: 952-957. Saw SM (2003): A synopsis of the prevalence rates and environmental risk factors for myopia Clinical & Experimental Optometry 86: 289-294. Saw SM, Tong L, Chua WH, Chia KS, Koh D, Tan DT & Katz J (2005): Incidence and progression of myopia in Singaporean school children. Investigative Ophthalmology & Visual Science 46: 51-57. Schaeffel F, Glasser A & Howland HC (1988): Accommodation, refractive error and eye growth in chickens. Vision Research 28: 639-657. Siatkowski RM, Cotter S, Miller JM, Scher CA, Crockett RS & Novack GD (2004): Safety and efficacy of 2% pirenzepine ophthalmic gel in children with myopia: a 1-year, multicenter, double-masked, placebo-controlled parallel study. Archives of Ophthalmology 122: 1667-74. Smith EL & Hung LF (2000): Form-deprivation myopia in monkeys is a graded phenomenon. Vision Research 40: 371-381. Smith EL, Ramamirtham R, Qiao-Grider Y, Hung LF, Huang J, Kee CS, Coats D & Paysse E (2007): Effects of foveal ablation on emmetropization and form-deprivation myopia. Investigative Ophthalmology & Visual Science 48: 3914-3922. Villarreal MG, Ohlsson J, Abrahamsson M, Sjöstrom A & Sjöstrand J (2000): Myopisation: the refractive tendency in teenagers. Prevalence of myopia among young teenagers in Sweden. Acta Ophthalmologica Scandinavica 78: 177-181. Wallman J & Adams JI (1987): Developmental aspects of experimental myopia in chicks: susceptibility, recovery and relation to emmetropization. Vision Research 27: 1139-1163. Wiesel TN, Raviola E (1977): Myopia and eye enlargement after neonatal lid fusion in monkeys. Nature 266: 66-68. World Health Organization (2000): Elimination of Avoidable Visual Disability due to Refractive Errors (WHO/PBL/0079) Geneva: World Health Organization; Vision 2020 Zadnik K, Manny RE, Yu JA, Mitchell GL, Cotter SA, Quiralte JC, Shipp M, Friedman NE, Kleinstein RN, Walker TW, Jones LA, Moeschberger ML & Mutti DO (2003): Ocular component data in schoolchildren as a function of age and gender. Optometry and Vision Science 80: 226-236. Zadnik K, Mutti DO, Friedman NE, Qualley PA, Jones LA, Qui P, Kim HS, Hsu JC & Moeschberger ML (1999): Ocular predictors of the onset of juvenile myopia. Investigative Ophthalmology & Visual Science 40: 1936-1943. Zhao J, Pan X, Sui R, Munoz SR, Sperduto RD & Ellwein LB (2000): Refractive Error Study in Children: results from Shunyi District, China. American Journal of Ophthalmology 129: 427-435. IV Ocular Motility Development Jan Ygge Introduction Ocular motility, i.e. the ability to move the eyes is very important for humans to have a good visual function. Our eyes are equipped with a fovea, i.e. the area of the retina with the highest visual acuity. Since this fovea represents only about a degree of the visual field we only have a high visual acuity in a very limited part of the visual field. Therefore we need to move the eyes in order to keep the visual surroundings updated. To do so it is required that the eyes are able to i) keep a steady fixation on a stationary target of visual interest, ii) keep a steady fixation although the target is moving, iii) move the eyes precisely to different parts of the visual field and iv) have a well developed eye alignment and avoid double vision. Eye movements of different types are required for these specific functions, and they are controlled by different areas of the brain and the brain stem. The separate types normally mature during different stages of child development. Therefore studies of the development of the eye movement types can bring information about the maturity of the specific brain region from which it is generated and also help in diagnosing and following diseases in the brain and brainstem. Visual Fixation Visual fixation is the ability to hold the eyes stable on a stationary target both when the head and body are stationary as well as when in motion. This is crucial for the good visual function since as stated above the visual acuity is highest within only a very small part of the visual field. A stable fixation is usually interrupted by several involuntary eye movements such as micro tremor, visual drift, and micro saccades and blinks (Fig. 1). Figure 1. Ten seconds recording of a ten year old child fixating a stationary target on a computer screen. Note the presence of micro saccades, drifts and tremor It was recently shown that the ability to keep a steady fixation on a stationary target matures with age and that this ability does not reach adult values until in the teens (Fig. 2). A stable fixation is also required when the head and body are moving. Since humans are in motion most of the time we need an effective reflex to obtain a stable view of the visual surroundings. Two reflexes, both initiated in the balance organ in the inner ear serve this function. The VOR, i.e. the vestibulo-ocular reflex originates in the semicircular canals of the vestibular apparatus in the inner ear. The semicircular canals detect rotational forces in all directions. The signals from them help keep the eyes on a target by inducing eye movements that compensate for body and/or head movements. This ability develops early in childhood and a well functioning VOR can be seen already at a few days of age. Figure 2. Histograms showing increased fixational stability by lesser number of intruding saccades during fixation. Note also that the number of blinks during fixation is almost similar between the different age groups. Group A1 represent children 4-7 years, A2 6-9 years, A3 912 years and A4 12-15 years. When the human body rotates with larger amplitude the VOR cannot compensate fully for the rotation since the amplitude response of the reflex is limited. Instead the OKN, i.e. the optokinetic reflex keeps the eyes on a target when the body is rotating or the visual scene is moving with larger amplitude. An example is when being on a train and looking out of the window. The image of the world outside is moving and in order to get a detailed view of a target, the eyes have to follow it. When the eyes reach a certain deviation and viewing sideways becomes inconvenient, the eyes move rapidly towards the straight ahead position to fixate on a new target and then follow it. In doing so fixation and good vision is maintained on targets of interest, although the surrounding is moving. The sequence of following eye movements and rapid re-fixations is the OKN. The same reflex is effective when we view the surroundings sitting on a rotating chair. The OKN is quite a primitive reflex and it develops early. However, during the first months of life directional asymmetries have been observed. When testing the monocular OKN, the temporal-nasal directed OKN is seen to be developed earlier than the nasal-temporal OKN. Normal OKN is not developed until about a year of age. In subjects with early childhood strabismus this directional asymmetry is known to persist throughout life. Saccadic system As stated above, the area of a good visual acuity is corresponding to only about a degree of the visual field and in order to view a larger visual scene we need to move our eyes to fixate different parts of interest. These eye movements, called saccades, are used both spontaneously as well as voluntary in all our daily activities. When reading for example, the line of sight is not moved continuously over the text but instead in small jumps, saccades, between different parts of fixation in the text. The amplitude of saccadic movements and the duration of the fixation periods depend on the complexity of the text and the reading comprehension. It is known that the more difficult the text, the shorter are the saccadic jumps between points of fixation. It is also known that the beginner reader makes smaller saccades and longer fixations on the different words before acquiring an adult reading performance (Fig. 3). Figure 3. Increased fixational stability by more central fixation with increasing age. For explanation of procedure see text. Same age groups as fig 2. The saccadic system has to be trained to mature. There are two fundamental differences between mature saccadic performance and saccades performed by a child. Firstly, it is known that the latency to initiate a saccade is about 200 msec in the adult whereas in the child the latency can be much longer. The saccadic latency in a preschool child is usually about 400 msec, i.e. twice the adult value (Fig. 4). The system matures with age and adult values for saccadic latencies will be reached at about the age of school start or even later. The other difference between a child and an adult regarding saccadic development is that the child usually makes multi-step saccades. Since the saccadic system is still immature, the ability of a child to adequately calculate the exact amplitude of a saccade is not yet developed. Thus the child will make several saccadic steps when trying to reach a target within the visual scene (Fig. 4). Also this function matures with age (and training) and adult values are probably reached by the early teens. Children with neurological disease such as Ataxia teleangiectasia will never reach adult values and they show also in the teens extremely long saccadic latencies. Figure 4. Reading eye movements in a normal 10 year old child (left) and a Dyslexic 10 year old (right). Same time scale in both figures. Note that the normal child performs better reading eye movements with two lines completed during the recording while the Dyslexic child during the same time has almost only completed reading of one line of text due to longer fixations and shorter reading saccades. Smooth pursuit eye movements In order to keep a moving target in a visual scene on the foveal area representing best vision, we need to track the target. The eye movements that serve this function are the smooth pursuit movements. The ability to exactly track the moving object requires practice to get well calibrated. This ability to perform adequate smooth pursuit movements develops with the maturation of the fovea and visual acuity, since a good vision is needed to be able to see the target and to track it. During the period of fovea development and subnormal visual acuity, small children often exhibit a cogwheel tracking, i.e. a tracking consisting of with small saccades instead of a smooth pursuit movement. This type of tracking is represented by a very low so called smooth pursuit gain, i.e. the ratio between eye position and target position is below normal. The smooth pursuit gain in adults usually is close to 1.0, meaning that the eye is tracking the target almost perfectly. The pursuit gain in children can be as low as 0.6, which means that the eyes are directed exactly at the target only 60% of the time trying to track it. The adult smooth pursuit gain is probably reached at early teenage. Vergence eye movements The vergence eye movements are used for tracking targets in depth and for keeping the eyes aligned. Vergence eye movements depend on the maturation of the fovea and visual acuity function as does the smooth pursuit movements. The first months of life when the fovea starts to mature and the visual acuity increases, is also the time when accommodation begins to function and the vergence eye movements start to develop. A full convergence response to a near target can be seen already in a 2 months old baby (figure 5). Figure 5. Vergence in a two-month old child. However, the other vergence functions are not fully developed at this early age. Deviations of eye position can be seen in infants both in the horizontal and the vertical directions. Even if vergence positions stabilize during the first couple of years, they are probably not mature until the early teens (Fig. 6). Figure 6. Histograms showing the increased fixational stability in terms of horisontal and vertical vergence positional SD with increasing age. Both the horizontal as well as the vertical vergence stability increases. Conclusions The different eye movement systems mature at different times of child development. Some systems parallel the maturation of the visual acuity function as the smooth pursuit system and the vergence eye movements. On the other hand, some eye movement systems seem to be independent of the visual maturation such as the VOR and OKN, and they are functioning already soon after birth. It is therefore important when examining a child to take all the different eye movements systems into consideration and after a thorough clinical investigation draw conclusions if the child has a normal eye movement development or not. Several neurological, metabolic and endocrine inborn diseases include eye movement abnormalities, which must be separated from the normal development. With a careful investigation of the eye movement ability in the child such diseases can sometimes be excluded or verified. References Aring E, Grönlund MA, Hellström A & Ygge J. (2007): Visual fixation development in children. Graefes Arch Clin Exp Ophthalmol. 11:1659-1665. Leigh J & Zee DS (2006): Neurology of Eye movements, fourth edition, Oxford University Press, Oxford. Riise R, Ygge J, Lindman C, Stray-Pedersen A, Bek T, Rødningen OK & Heiberg A. (2007): Ocular findings in Norwegian patients with ataxia-telangiectasia: a 5 year prospective cohort study. Acta Ophthalmol Scand 85:557-562. V Childhood Strabismus Gunnar Lennerstrand Introduction Strabismus is a condition in which the two eyes are not parallel but one is deviated with respect to the other, horizontally and/or vertically. The cause of childhood strabismus is generally unknown, although weakness of one or several of the eye muscles may be present as will be shown in the case presentation below. The most common type of strabismus, without any obvious dysfunction of the eye muscles, is called concomitant strabismus, implying that the angle or size of the strabismus is more or less constant, irrespective of the direction of gaze. This is in distinction to strabismus due to muscle weakness, called incomitant strabismus where the angle varies with the direction of gaze. Manifest concomitant strabismus is quite a common disease, affecting about 2 % of the population. In this type of strabismus the eyes are constantly deviated in relation to each other. Latent concomitant strabismus is even more common and seen in more than half the population. In latent strabismus the eyes stay straight most of the time due to activation of the eye muscles over the visual system to keep the eye aligned in binocular single vision. After the presentation of a case of complicated strabismus, the effects of strabismus on the visual functions will be described, and the connections between strabismus and eye muscle function and eye proprioception explored. Case report The following case report exemplifies recent advances in the management of a difficult case of incomitant strabismus. An infant boy presented with horizontal convergent strabismus of a very large angle, as a part of a so called Möbius syndrome, a congenital disorder, involving weakness of both the outer (lateral) eye muscles and of many of the facial muscles (Fig. 1, left). Ordinary surgery for convergent strabismus failed due to the complete absence of function of both lateral eye muscles. In order to restore some ability to deviate the eyes to the sides and obtain an acceptable eye position, the tendons of the upper and lower vertical eye muscles were transposed to the insertion of the non-functioning lateral eye muscles. A weakening was also done of the inner (medial) horizontal eye muscles of both eyes by injection of Botulinum toxin into the medial muscles. This combination of surgical and pharmacological procedures resulted in fairly straight eyes (Fig. 1, right), a limited range of horizontal movements and almost normal vertical eye motility. Vision was normal in both eyes due to alternate fixation and well performed occlusion therapy during the first years of life (see Chapter I). Binocular vision was abnormal as a result of the early onset strabismus. Figure 1. (Left) Boy 18 months old with Möbius´syndrome, prominent convergent strabismus and slight vertical strabismus. (Right) Same boy at 9 years of age after strabismus surgery supplemented with Botulinum toxin. Much improved appearance, although some vertical strabismus remains. Visual functions In manifest strabismus where one of the eyes is constantly out of line, the child will experience double vision. In childhood the visual system is very flexible and double vision may be quite easily compensated and shifted into single vision by suppressing the image of one eye at a time. However, suppression may impair the visual development of the eye that is out of line most of the time, i.e. the image of the object fixated is falling outside the fovea centralis. In order to prevent reduced vision of the deviated eye treatment is instituted. It consists of occlusion of the better eye with a patch for a period each day. In most cases glasses are also prescribed, producing sharp images on the retina of the two eyes and supplementing the occlusion therapy. The therapy has to be started at an early age, and continued and supervised up to about age 10-12, during the so called plastic period of visual development (see also Chapter I). Suppression leads to disrupted binocular vision, the main part being loss of stereopsis, but this is a visual handicap of very limited consequences for the individual with strabismus. Reduced vision due to strabismus is uncommon in our country as a result of the extensive scheme for visual screening of young children and early treatment of children with impaired vision in one or both eyes (see also Chapter VI). Thus, we now know very much of the visual dysfunctions that are a result of manifest strabismus and we have reliable means to detect and treat them. Motor functions Some types of convergent strabismus are connected with refractive errors of the child´s eye, the most common being hyperopia (far-sightedness). In order to see clearly without glasses, the hyperopic eye has to accommodate and the motor activity of the ciliary (focusing) muscle inside the eye produces an impulse to converge the eyes, which may result in a manifest convergent strabismus. This type of strabismus may be cured by proper glasses to compensate the hyperopia. In concomitant strabismus there exist only small abnormalities of eye muscle function. The eye muscles that move the eyes and control the gaze positions are known to be very fast and strong with respect to their size, and also very fatigue resistant. Fast movements are used in repositioning the eyes and delicate but long-lasting muscle activity is needed in steady fixation with both eyes directed to the same point in space. The muscle components for steady fixation have been shown to develop earlier than those for swift eye movements, showing that steady control of the eye position is needed for proper development of visual acuity and binocular functions. Function of the muscle components can be adjusted in proportion to visual activity, and in strabismic eye muscles the components for steady control do not develop to a full extent when the need for steady control in binocular vision is reduced. In some of the divergent types of strabismus the eyes have to converge constantly in order to overcome an inherent outward deviation and subsequently the medial eye muscles become stronger in order to keep the eyes straight. Control of eye position is mediated also by connective tissue structures outside the eye muscles proper. These structures can control the muscle tendon directions and therefore influence the actions of the muscle on position and movements the eye globe. The connective tissue structures are under influence of the eye muscles themselves, possibly independent of the main eye muscle activity. This would imply that eye position and eye movements are controlled by two muscle systems, one directly acting on the eye globe and the other indirectly by adjusting the sideway forces on the muscle tendon. The control of the connective components around the tendon could be of importance for high precision eye movement activities in e. g. prolonged fixations for near, but the clinical significance of this motor system and how it works in strabismus has to be further investigated. Eye muscle proprioception The disturbances that strabismus exerts on vision are treated with glasses and occlusion as described in Chapter I. There is as yet no effective treatment for binocular dysfunction. Even if the eyes seem properly aligned by surgery at an early age, and weak binocularity may be restored, the stereoscopic vision will always remain abnormal. Eye muscle surgery is the common mode of treatment and it is generally performed at an age when the child can cooperate in mea in creating an acceptable eye position and facial appearance, so important for the self-esteem and social interaction of the child. Surgery also often creates conditions for some binocular vision although abnormal. In addition to surgery, treatment with eye muscle injection of Botulinum toxin A has been recently introduced. Such injection can reduce small angle strabismus without surgery and has been used in childhood strabismus of both manifest and latent types. In may be useful also in the treatment incomitant strabismus as shown in the Case report. Treatment of strabismus The disturbances that strabismus exerts on vision are treated with glasses and occlusion as described in Chapter I. There is as yet no effective treatment for binocular dysfunction. Even if the eyes seem properly aligned by surgery at an early age, and weak binocularity may be restored, the stereoscopic vision will always remain abnormal. Eye muscle surgery is the common mode of treatment .It is generally performed at an age when the child can cooperate in the measurements needed for surgery. The aim of surgery is to create an acceptable eye position and facial appearance, so important for the self-esteem and social interaction of the child. Surgery also often creates conditions for some binocular vision although abnormal. In addition to surgery, treatment with eye muscle injection of Botulinum toxin A has been recently introduced. Such injection can reduce small angle strabismus without surgery and has been used in childhood strabismus of both manifest and latent types. In may be useful also in the treatment incomitant strabismus as shown in the Case report. Conclusions Concomitant childhood strabismus is a common eye disorder and about 2% of the population is affected by the manifest type and at least 50% by the latent type. The cause of strabismus is most likely a deficiency in the visual system leading to a misalignment of the eyes. Manifest strabismus is accompanied by reduced vision, sometimes manifested as monocularly reduced visual acuity and always as reduced binocular vision. Latent strabismus may cause visual discomfort and headache due to eye muscle fatigue in keeping the eye aligned. The ocular motor dysfunction is considered secondary to the primary visual deficits. In order to gain further understanding of the underlying basic mechanisms of strabismus more studies are needed of the visual and ocular motor development. References Lennerstrand G, Tian S & Han Y. (2000).: Functional properties of eye muscles: motor and sensory adaptation in strabismus. In Lennerstrand G & Ygge J (eds) Advances in Strabismus Research: Basic and Clinical Aspects”, Wenner-Gren International Series, vol. 78, Portland Press, London, pp 3-15. Lennerstrand G (2007): Strabismus and eye muscle function. A review. Acta Ophthalmol Scand, 85: 711 – 723 Lennerstrand G, Bolzani R, Schiavi C, Tian S & Benassi M (2009): Isometric force development in human horizontal eye muscles and pulleys during saccadic eye movements. Acta Ophthalmologica, 87: 837 – 842. VI Visual Screening in Children Peter Jakobsson Introduction Screening for ocular disease and visual dysfunction in children has been conducted at different levels and to varying extent in different countries of the world. There are two main periods in a child’s life that are of special interest. In the neonatal period detection of organic disease such as congenital cataract and retinopathy of prematurity (ROP) is important. Screening for congenital cataract is a type of mass screening, where every child is examined, while examination for ROP is a selective screening of a special high-risk group of premature babies. For many of the congenital ocular conditions there may be no treatment available as such, but an early detection is nonetheless essential since early visual rehabilitation plays an important role in the child’s visual development. In the developed countries the incidence of severe visual handicap has been quite constant at about 3 in 10 000 inhabitants for several decades (Riise 1993). For other conditions such as cataract and ROP there are successful treatments and for the individual this could mean the difference of being socially blind or seeing as an adult. The other period in a child’s life at the age of 2-4 years involves finding less serious conditions, mainly amblyopia. Amblyopia is preferably diagnosed by testing monocular visual acuity. Amblyopia Amblyopia is defined as a reduction in visual acuity due to abnormal visual development, usually caused by a defocused retinal image where a refractive error leads to under-stimulated neurons in the visual cortex or by inhibition of the connections to the neurons in the visual cortex of one eye caused by anisometropia or strabismus. It is the most common cause of reduced vision in the population below the age of 50 years and the prevalence is about 3% (Hauffman 1974). Amblyopia can be treated successfully if detected at an early age, i.e. in the preschool years. Strabismus is usually detected and diagnosed in the first years of life at home or at the Child Health Care Centers, while amblyopia caused by refractive errors and anisometropia more commonly is detected with testing of monocular visual acuity at the Child Health Care Centers. The disability caused by having amblyopia in one eye has been disputed (Snowdon & Stewart-Brown 1997). In a study by Packwood et al. (1999) a significant number of amblyopic patients complained that the amblyopia interfered with school (52%) and work (48%). Although there is argument about the significance of having amblyopia in one eye there is little argument about the fact that a patient is seriously handicapped when losing vision in the non-amblyopic eye. Amblyopia was the main cause of decreased visual acuity in one eye in at least 1.72% of the patients at visual rehabilitations centres (Jakobsson et al. 2002). This means that approximately 1.2% of the people with amblyopia ≤0.3 will eventually become visually handicapped due to lesions in the better eye. This visual handicap could have been avoided by screening and treatment in childhood. Screening in the world The most extensive programs of ocular and visual surveillance and with good attendance from the parents and children seem to be those performed in Scandinavia and Holland and in some provinces in Canada (Köhler & Stigmar 1973, 1978; Nörskov 1984; Lantau et al. 1991; Lantau 1992; MacPherson et al. 1991). The attendance rate at the Child Health Care Centres is reported to be 95% or more in Sweden and Holland for the children below 1 year of age, but lower in the other countries. In the studies from Denmark, where population studies have been performed before and after the introduction of screening programs for children, the prevalence particularly of deep amblyopia (visual acuity <0.1) has been reduced markedly, from 1.5% before screening to <0.01% when screening was introduced and amblyopia treatment was started at an early age (Vinding et al. 1991, Jensen & Goldschmidt, 1986). Screening in Sweden Screening for visual disorders was introduced in Sweden in the 1960-ies and a national program was established in the 1970-ies. Nordlöw and Joachimson (1966) and Köhler and Stigmar (1973, 1978) showed convincingly that amblyopia and other types of visual disorders could be efficiently detected by monocular testing of visual acuity, performed by the nurses at the Child Health Care Centers in all children when they were 4 years of age. This system has now been in use for almost 40 years. All children are examined within the Child Health Care system at the age of 1–3 days, 6–12 weeks, 6, 18 and 36 months. These examinations are done by visual inspection and behavioural testing. The children with clear or suspected visual and ocular abnormalities are referred to (paediatric) ophthalmologists. All children are tested for monocular visual acuity at the age of 4 years (and also at 5.5 years in some areas), at the Child Health Care Centres, and in school at 7 years and 10 years of age. Visual acuity (VA) is tested on charts with optotypes in rows. A more extensive study was performed in three different populations of 10-years old children (Kvarnström et al. 1998, Kvarnström et al. 2001), in order to determine the efficiency of the system of screening at the Child Health Care Centers. Some of the results of this study will be presented in the following: The attendance rate was more than 99%. The sensitivity was 92 % and specificity was 97%, both very high. The numbers of false negative and false positive cases were small. Figure 1 show the total number of patients who are referred to the Eye Clinic at different ages. As expected there is a predominant peak at the age of 4 and less predominant peaks in the first year of life, and at 5 and 7 years. After the age of 8, the patients are mostly referred to opticians. These children are not included in this diagram. Number of children 160 140 120 100 80 60 40 20 0 0 1 2 3 4 5 6 7 8 9 10 11 Age (years) Figure 1. Age at referral to the eye clinic (Jakobsson et al. 1996). Figure 2 shows a more detailed view of when refractive errors are detected. The first vision test is done at 4 years and as can be seen the main part of the ametropes are detected here. The ametropes detected earlier than this are mainly those with known hereditary factors. Quite a few of the ametropias are also diagnosed after the age of 4, which is seen in the figure. The graph does not display the children who are referred to the optician. This means, for instance, that children older than 8 years who are developing myopia do not show up in this diagram. 70 Ametropia Number of children 60 Anisometropia 50 40 30 20 10 0 0 1 2 3 4 5 6 Age (years) 7 8 9 10 11 Figure 2. Age at detection of refractive errors (Jakobsson et al. 1996). In the first year of life many cases of strabismus are diagnosed (Figure 3). Among these are the children with infantile esotropia and those with known heredity. Between 1 and 4 years additional cases of strabismus are discovered. Many children with strabismus are detected at 4 years of age, and one third of them have microtropia. After the age of 4, very few cases of strabismus are detected, which is also a sign of the efficiency of the screening system at the earlier ages. Number of children 25 20 Strabismus Strabismus + ametropia 15 10 5 0 0 1 2 3 4 5 6 Age (years) 7 8 9 10 11 Figure 3. Age at detection of strabismus (Jakobsson et al. 1996). How efficient has the screening system in combination with early treatment been at reducing the prevalence of amblyopia? This is illustrated in Table 1 where a comparison has been made between the prevalence of amblyopia prior to the screening system (Lennerstrand 2000) and after (Kvarnström et al. 1998). The table shows that the benefits of screening and amblyopia treatment are most pronounced for the lower visual acuities. The number of persons with visual acuity ≤ 0.3 is reduced 10-fold while the number of persons with visual acuity ≤ 0,1 is reduced almost 20-fold. Table 1. The prevalence of persons with different degrees of amblyopia before (Lennerstrand et al. 2000) and after screening (Kvarnström et al. 1998). Visual acuity ≤ 0,1 ≤ 0,3 ≤ 0,5 ≤ 0,7 Lennerstrand et al. 2000 1.15% 2.00% 2.84% 3.77% Kvarnström et al 1998 0,06% 0,19% 0.90% 1.70% At which age should the child be tested? Since amblyopia should be detected as early as possible Kvarnström and Jakobsson (2005) tested if visual acuity could be examined at the age of 3 years instead of 4. Three-year-old children co-operate well in visual acuity testing. However, the examination time is a little longer and the testability rate is about 10% lower than at 4 years. However, the positive predictive value was 58% for the 3-year-olds as compared to 75% for the 4-year-olds. This puts an extra load on the eye clinics and it is therefore doubtful whether visual acuity testing at 3 years is worthwhile. Conclusions Screening for visual disorders in combination with treatment has proven to be an efficient way of reducing visual impairment and amblyopia. Visual acuity testing in 4-year-old children has a high sensitivity and specificity. The prevalence of amblyopia with visual acuity below 0.5 is very low compared to the prevalence without visual screening. Together with additional measures in Child Health Care system to detect ocular disorders, the rate of serious amblyopia has been substantially reduced. References Hauffman M (1974): Reduction of visual acuity in a Swedish population. Ph. D. Thesis, Karolinska Institutet. Jakobsson P., Kvarnström G. and Lennerstrand G. (1996) Amblyopia in Sweden. Transactions of the 23rd European Strabismological Association Meeting 23, 25-30. Jakobsson P, Kvarnström G, Abrahamsson M, Bjernbrink-Hörnblad E & Sunnqvist B (2002): The frequency of amblyopia among visually impaired persons. Acta Ophthalmologica Scand 80: 44-46. Jensen H & Goldschmidt E (1986): Visual acuity in Danish school children. Acta Ophthalmologica 64: 187- 191. Kvarnström G, Jakobsson P & Lennerstrand G (1998): Screening for visual and ocular disorders in children, evaluation of the system in Sweden. Acta Paediatr 8: 1173 – 1179. Kvarnström G, Jakobsson P & Lennerstrand G (2001): Visual screening in Sweden: An ophthalmological evaluation. Acta Ophthalmologica Scand 79: 240-244. Kvarnström G & Jakobsson P (2005): Is vision screening in 3-year-old children feasible? Comparison between the Lea Symbol chart and the HVOT (LM) chart. Acta Ophthalmol Scand 83: 76-80. Köhler L & Stigmar G (1973): Vision screening of four-year-old children. Acta Paediatr Scand 62: 17-27. Köhler L & Stigmar G (1978): Visual disorders in 7-year-old children with and without previous vision screening. Acta Paediatr Scand 67: 373-377. Lantau K, Loewre-Sieger DH & Wenniger-Prick LJJM. (1991): Early detection of visual disorders in young children in health care centers- implementation into the Netherlands - age: 0-4 years. In: "Advances in amblyopia and strabismus", Transactions of the 7th International Orthoptic Congress, pp 357. Lantau K (1992): Early visual screening at age 1, 9, 18 and 30 months with the VOV-method: instruction of the method by orthoptists to all community doctors in the Netherlands. In: Kaufmann H (ed) Transactions of the 20th Meeting of the European Strabismological Association, Brussels. pp 339-341. Lennerstrand G, Hauffmann M, Jakobsson P, Kvarnström G & Lindeberg A (2000): Prevalence of amblyopia in Sweden 1970 and 1992. In: Spiritus M (ed) Transactions of the 26th European Strabismological Association Meeting, Brussels. 26: 3-6. MacPherson H, Braunstein J & La Roche GR (1991): Utilizing basic screening principles in the design and evaluation of vision screening programs. Am Orthoptic J 41: 110- 121. Nordlöw W & Joachimsson S (1966): The incidence and results of treatment of reduced visual acuity due to refractive errors in four year old children in a Swedish population. Acta Ophthalmol (Copenh) 44: 152-163. Nörskov K (1984): Screening for amblyopia in pre-school children in Denmark. In: Transaction of the 14th meeting of the European Strabismological Association, Jenkodan Tryk AS, Copenhagen, pp 327. Packwood E, Cruz O, Rychwalski P & Keech R (1999): The psychosocial effects of amblyopia study. J AAPOS 3: 15-17. Riise R (1993) Nordic registers of visually impaired children. Scand J Soc Med. 21: 66 - 68. Snowdon SK & Stewart-Brown SL (1997): Preschool vision screening. Health Technol Assess 1997 1: 1-75. Vinding T, Gregersen E, Jensen A and Rindziunski E (1991): Prevalence of amblyopia in old people without previous screening and treatment. An evaluation of the present prophylactic procedures among children in Denmark. Acta Ophthalmol 69: 796 - 798. VII Pediatric Cataract Maria Kugelberg Introduction A study in Sweden showed the incidence of all congenital cataract cases to be 36/100,000 (Abrahamsson et al. 1999). In addition, a few hundred children develop juvenile cataract each year in Sweden. Congenital cataract is considered to be the most common cause of treatable blindness in children. It is present at birth and may be unnoticed until the visual function is affected or a whitish pupil is seen. If the babies do not have surgery quickly they develop irreversible amblyopia. Pediatric cataract surgery is nowadays an increasingly safe procedure, although there are some complications to the surgery. Visual axis opacification is the most common complication, which threatens the vision again and can lead to amblyopia if not managed. Secondary glaucoma is the most feared complication and can lead to blindness and a cosmetically disturbing eye. Developmental cataract, which is not dense at birth, is more common and could be operated on much later. This would lead to fewer complications and a better outcome. Congenital cataract Congenital cataract is hereditary in approximately one third of the cases. It is often inherited autosomal dominant but can also be inherited autosomal recessive or X-linked. In approximately one third of the cases other diseases can be found. Metabolic disorders, such as galactosaemia and hypocalcaemia are rare causes. Intrauterine infections such as rubella, toxoplasmosis, herpes, varicella and syphilis can cause congenital cataract. Genetic syndromes such as trisomy 21 or Turner’s syndrome and a variety of neurological disorders are often associated with congenital cataract. Other ocular anomalies such as iris coloboma, aniridia, microphthalmia, retinopathy of prematurity, or persistent foetal vasculature (PFV) are often combined with cataract. In the rest of the patients, the congenital cataract is idiopathic. In unilateral cases, the cause is most often idiopathic and in a clinically healthy child, or if the cataract is inherited, there is no need for an extensive pre-operative evaluation. 5-20% of childhood blindness worldwide is caused by cataracts. There are different types of cataract; nuclear, lamellar, sutural, polar, lenticonus, membranous and those associated with PFV. The size, density, laterality of the cataract and the presence of associated ocular abnormalities decide how strong the indication is for surgery. The more central and the more posteriorly located, the more visually significant the cataract will be. Since there are more complications after early surgery as discussed below, it is important to wait if the cataract is not visually significant. In cases with dense congenital cataract the cataract surgery must be performed early to prevent irreversible amblyopia and nystagmus. At the same time the risk of secondary glaucoma increases in these very small children, the earlier the surgery is performed. It is therefore very important to find ways to reduce the risk for secondary glaucoma. Also, the visual axis opacification formation is much more pronounced in the youngest children. Secondary glaucoma The earlier the surgery is performed, the greater the risk of secondary glaucoma. The risk also seems to be greater in small eyes, as in microphthalmus with persistent fetal vessels. It is yet not clear what causes the secondary glaucoma. However, an IOL seems to decrease the risk. Arsani et al (Asrani et al. 2000) found a much higher rate of glaucoma following cataract surgery in patients who were left aphakic (14/124 patients), than if they were implanted with an IOL (1/377 patients). They also reviewed the literature and found no reported case of openangle glaucoma in the over one thousand pseudophakic patients from the studies. In one of our studies, no eye out of 31 children implanted with a small acrylic SA30AL IOL at 2-28 months of age developed secondary glaucoma (Kugelberg et al. 2006). In a rabbit study we performed with 20 three week old rabbits, no eye implanted with an AcrySof SA30AT IOL developed secondary glaucoma, but three aphakic eyes did during the follow-up time. However, in other animal studies with different IOLs the frequency of secondary glaucoma was similar in aphakic and pseudophakic eyes. It might also be due to the increased inflammatory response in young children and infants, compared to older children. Treatment of postoperative aphakia Implantation of an IOL is now a common and accepted management of the postoperative aphakia even in the smallest children. For the very small eye of an infant most of the commercially available IOLs are too large. The myopic shift that occurs in the child’s growing eye is also a great concern. Lately, after surgery for unilateral cataract, many surgeons implant an IOL also in infants. However, for optical correction in bilateral cases with congenital cataract, contact lenses are probably still most often used in the Western World. Contact lenses can cause infection, are sometimes hard to handle, tedious for the family and expensive. Compliance is often also poor regarding the use of contact lenses. Therefore it would be of great interest if it were possible to develop an IOL that fits the small eye. We have performed some studies evaluating different smaller lenses in a rabbit model and in small children. They seem well tolerated by the small eye. Visual axis opacification Visual axis opacification or after-cataract occurs when lens epithelial cells (LECs) migrate and proliferate from the anterior capsule and the equator of the lens capsule, onto the posterior capsule. The visual axis is then obscured, and vision blurred again. Children develop more and faster visual axis opacification than adults. This opacification, or posterior capsule opacification as it is called in adults, can be removed in a second procedure in adults, using Neodymium: YAG (Nd:YAG) laser. An opening is then created in the posterior capsule, and the vision is clear again. In most cases, visual axis opacification in children can not be removed with only Nd:YAG laser, because the LECs will continue to grow on the anterior vitreous surface. The opacification has preferably to be removed in a second surgical procedure with anterior vitrectomy, often via the pars plana. However, in the very small children the LECs can grow also on the posterior surface of the IOL, even after a vitrectomy is performed. To diminish visual axis opacification in children, most cataract surgeons perform posterior capsulorhexis at surgery. It is also debated whether or not to do an anterior vitrectomy at primary surgery. It could be performed through the pars plana, or through the anterior chamber after the posterior capsulorhexis and implantation of an IOL. When the anterior vitreous has been removed, the LECs most often cannot grow on the remaining vitreous. It seems that anterior vitrectomy is necessary at least in children below 5 years, to avoid rapid visual axis opacification. Another surgical technique that has been studied is a so called optic capture, i.e. the IOL is pushed through the posterior capsulorhexis, while the haptics remain in the bag. However, the technique does not seem to fully prevent the formation of visual axis opacification, and it has been described that the anterior vitreous face became semi-opaque and that the LECs can grow also on the anterior surface of the IOL. However, optic capture might be a suitable technique in some instances, since it provides a good centration of the IOL, which is necessary in cases after trauma or an incomplete rhexis. Removal of residual LECs during the primary surgery is a key factor in avoiding posterior capsule opacification. Several chemicals have been suggested in experimental settings to remove or destroy residual LECs, but it has to be kept in mind that the substances may be toxic to other ocular structures. Research is directed towards finding a device or substance that can selectively remove the LECs. There are always complications associated with touching the vitreous and breaking the posterior lens capsule. If this can be avoided, it would be highly advantageous. This however, generates the need for a lens capsule with no remaining LECs. Perhaps a sealed-capsule irrigation could be an option at least in pediatric patients. Perfect Capsule The sealed-capsule irrigation device, Perfect Capsule, invented by Anthony Maloof (Agarwal et al. 2003), consists of a silicone plate, 0.7 mm thick, 7 mm in outer diameter, and 5 mm in inner diameter. It has an inflow tube, an outflow tube, and a tube for creation of a vacuum. The device can be folded and introduced through a normal small incision. After the lens extraction, the device is placed over the anterior capsulorhexis, and a vacuum is created with a syringe. This produces a sealed system between the capsular bag and the device. The capsule can be irrigated with a substance through the inflow tube, and the substance does not come in contact with the other intraocular structures. The substance is washed out with balanced salt solution (BSS), the vacuum is released, and the device is withdrawn. An IOL then can be placed in the bag. Human studies have reported the safety of the device in adults undergoing cataract surgery. In that study, the sealed system was irrigated with distilled deionized water, which did not prevent posterior capsule opacification development. Earlier in vitro studies had shown that the LECs succumbed from osmotic lysis when they were exposed to distilled deionized water. However, this evidently did not work in vivo. We evaluated the Perfect Capsule in a young rabbit model. Our experiments showed that 5fluorouracil 50 mg/ml was the most effective substance evaluated to prevent visual axis opacification (Abdelwahab et al. 2008) (Fig. 1 D). We also investigated a substance called thapsigargin, which has proven effective in in vitro studies of human LECs, but the substance was not effective in our model (Fig. 1). Tg BSS 5-FU 25 mg/ml 5-FU 50 mg/ml Figure 1. Rabbit eyes that have undergone clear lens extraction and irrigation with different substances in the sealed-capsule irrigation device Perfect Capsule. Conditions six weeks postoperativly. (Top left) Eye irrigated with thapsigargin. The eye shows synechia and visual axis opacification. (Top right) Eye irrigated with BSS; synechia and visual axis opacification is seen. (Bottom left) Eye irrigated with 5-fluorouracil 25 mg/ml. Some synechia is seen. (Bottom right) Eye irrigated with 5-fluorouracil 50 mg/ml. A clear visual axis and no synechia (Abdelwahab et al. 2008). The safety of 5-FU 50 mg/ml as an irrigation substance with the Perfect Capsule device was investigated, no damage was seen in the corneal endothelium, trabecular meshwork, and central and peripheral retina. We did not detect any damage when looking at the posterior capsule with transmission electron microscopy. Conclusions In conclusion, pediatric cataract is still much more problematic than cataract in adults. However, nowadays, IOLs are implanted at a younger age, less secondary glaucoma is then seen, and methods are invented to diminish the visual axis opacification. Hopefully, the research can continue and provide even more information to aid the children in the future. References Abdelwahab MT, Kugelberg M & Zetterstrom C (2008): Irrigation with thapsigargin and various concentrations of 5-fluorouracil in a sealed-capsule irrigation device in young rabbit eyes to prevent after-cataract. Eye (Lond) 22: 1508-13. Abrahamsson M, Magnusson G, Sjostrom A, Popovic Z & Sjostrand J (1999): The occurrence of congenital cataract in western Sweden. Acta Ophthalmol Scand 77: 578-80. Agarwal A, Agarwal S & Maloof A (2003): Sealed-capsule irrigation device. J Cataract Refract Surg 29: 2274-6. Asrani S, Freedman S, Hasselblad V, et al. (2000): Does primary intraocular lens implantation prevent "aphakic" glaucoma in children? J Aapos 4: 33-9. Kugelberg M, Kugelberg U, Bobrova N, Tronina S & Zetterstrom C (2006): Implantation of single-piece foldable acrylic IOLs in small children in the Ukraine. Acta Ophthalmol Scand 84: 380-3. VIII The Impact of Growth and Growth Factors for Vascular and Neural Development in Preterms Ann Hellström Introduction Despite significant improvement in neonatal intensive care the number of preterm children with severe visual impairment is increasing. Retinopathy of prematurity (ROP) is a major cause of blindness in children in the developed and developing world, despite current treatment of late-stage ROP. Approximately 40% of perinatal blindness can be attributed to ROP. A recent Swedish study demonstrated that one third of the boys born below 25 weeks of gestational age became visually impaired or blind due to ROP and /or cerebral dysfunction (Jacobson et al. 2009). Angiogenesis is a complex process involving changes in many metabolic pathways. Our research group has found a strong association between the circulating growth factor Insulinlike growth factor 1 (IGF-I), postnatal growth and development of vascular and neural elements in preterm infants. Ours and others findings on this topic will be presented in detail below. IGF-I and foetal growth IGF-I is a polypeptide, which resembles insulin in its molecular structure. In humans IGF-I is primarily produced by hepatocytes in the liver and the production is regulated by pituitary growth hormone. IGF-I exists extra-cellular and is bound to and controlled by six insulin-like growth factor binding proteins. Seventy-five percent of the IGF-I is bound to insulin-like growth factor binding protein 3 (IGFBP-3) together with an acid labile subunit (ALS). The insulin-like growth factor binding proteins can either inhibit, or potentiate cellular IGF-I responses, and influence distribution and elimination of IGF-I. The cellular actions of IGF-I are mediated through binding of IGF-I to the IGF-I receptor, which is located on the surface of different cell types in all tissues. IGF-I can also bind to the insulin receptor, but at a much lower affinity than insulin. IGF-I is of major importance for foetal growth and is synthesized by all foetal tissues early in gestation, and the placenta is actively involved in regulating circulatory foetal levels of IGF-I. Concentrations of foetal IGF-I are closely related to placental transfer of nutrients. The disruption of placental nutrient supply as well as amniotic supply at birth is followed by a rapid decline in levels of IGF-I. During pregnancy thyroxine plays a more important role than pituitary growth hormone in the regulation of foetal IGF-I, but after birth IGF-I is regulated by pituitary growth hormone. IGF-I is related to nutrition, birth weight and gestational age (Hellström et al. 2003) . Nutrition is an important environmental factor influencing IGF-I levels. At very preterm birth the IGF-I levels of the newborn decrease abruptly, and do not reach normal intrauterine values for several weeks/months (Engström et al. 2005), in contrast to term infants who restore their serum levels of IGF-I in a few days. A recent study found a dramatic decrease in the circulating serum levels of IGF-I and its major binding protein, IGFBP-3 in very preterm infants and that inflammation at birth with increased cord levels of pro-inflammatory cytokines was associated with a decrease in IGF-I (Hansen-Pupp et al. 2007). The important role of nutrition for the foetal IGF-I levels was demonstrated in an animal study of foetuses of pregnant rats, who were fasted during the last days of gestation, and the serum IGF-I levels were 30 % lower than in the control foetuses (Davenport et al 1990). IGF-I and brain development IGF-I acts directly on the brain and promotes differentiation, proliferation and maturation of progenitors of neural stem cells, and has anti-apoptotic properties (Ye & D´Ercole 2006). Oligodendrocyte maturation is crucial for myelination as mentioned above, and several studies on mice and other rodents have shown an important role of IGF-I in differentiation of oligodendrocyte progenitor cells (Ye & D´Ercole 2006). In vitro, IGF-I has been found to promote remyelination and cerebellar Purkinje cell development. In addition, a relationship has recently been shown in preterm infants between cerebellar volume and serum IGF-I (unpublished data). IGF-I may also play an important role in the stimulation of postnatal brain growth. Overexpression of IGF-I in mice stimulated the brain growth and ameliorated the brain growth even in the face of under-nutrition, and IGF-I protected myelination in cases with undernutritional insults. A relationship between low circulating levels of IGF-I, the development of ROP, and poor development of head circumference in preterm infants has also been documented (Löfqvist et al. 2006). IGF-I is essential for the development of normal vascularisation of the human retina as mentioned above (Hellström et al. 2001, Hellström et al. 2002), and promotes the angiogenesis in the brain (Lopez-Lopez et al. 2004). In the study by Lopez-Lopez and co-workers (2004) systemic injections of IGF-I in adult mice increased the brain vessel density. A gender difference in IGF-I levels, where boys had lower levels than girls, has been shown in preterm (GA < 32 weeks) infants (Engström et al. 2005). IGF-I and retinal development in prematurity Ocular growth is influenced by IGF-I and treatment with IGF-I increases the ocular axial eye length in patients with short axial lengths due to growth hormone insensitivity (Laron syndrome). In infants born prematurely the retina is not fully vascularised. The more premature the child, the larger is the avascular area. The sudden loss of nutrition and growth factors necessary for normal growth at preterm birth causes the vascular growth that would normally occur in utero to slow down or cease. In addition, the relative hyperoxia of the extra-uterine milieu together with supplemental oxygen cause a regression of already developed retinal vessel. IGF-I is necessary for normal development of retinal blood vessels (Hellström et al. 2002). Preterm birth is associated with a rapid fall in IGF-I, and the baby often suffers from immaturity, poor nutrition, acidosis, hypothyroxemia and sepsis which all may further reduce the IGF-I levels. When the neural elements of the retina mature and need more oxygen, poor vascularisation leads to hypoxia and production of vascular endothelial growth factor (VEGF). If sufficient IGF-I is not available VEGF is accumulated, as a minimum level of IGF-I is required for VEGF to induce vessel growth. When the IGF-I levels slowly increase when the infant matures, and IGF-I reaches the minimum level for VEGF to promote vessel growth, an excessive and uncontrolled neovascularisation may take place, see figure 1. The serum levels of IGF-I during the first weeks of life in the babies are inversely correlated with the severity of ROP (Hellström et al. 2003). In an experimental study on neonatal mice it was recently shown that exogenous administered IGF-I attenuated retinopathy and improved weight gain as well as maturation (Vanhaesenbrouck et al. 2009). Hök Wikstrand et al (2009) recently demonstrated that preterm children had reduced neuronal rim area of the optic disc and that this finding was associated with both low birth weight and poor early postnatal growth. This indicates that early weight gain is important for neural development of the visual system in preterm children. The same authors also found in preterm infants that poor visual acuity and visual perception was correlated with poor early weight gain and that the infants with hyperopia at school age had low neonatal serum IGF-1 levels (Hök et al. 2010). Figure 1. Schematic representation of IGF-I/VEGF control of blood vessel development in ROP. (A) In utero, VEGF is found at the growing front of vessels. IGF-I is sufficient to allow vessel growth. (B) With premature birth, IGF-I is not maintained at in utero levels, and vascular growth ceases. (C) As the premature infant matures, the developing but nonvascularized retina becomes hypoxic. VEGF increases in retina and vitreous. With maturation, IGF-I level slowly increases. (D) When the IGF-I level increases, with high VEGF levels in the vitreous, endothelial cell survival and proliferation driven by VEGF may proceed. NV ensues at the demarcation line, extending into the vitreous, leading to retinal detachment and blindness can occur. (Hellström et al 2001). Program to predict severe ROP An association between poor postnatal growth and later development of ROP has earlier been reported (Wallace et al. 2000). Hellström and co-workers have recently developed a web-based program to predict which children are at risk of developing the most severe form of ROP. This program named WINROP combines in a highly novel way the use of neonatal data (weight) and biomarkers (serum IGF-I levels) with statistical monitoring (Löfqvist et al. 2006). Löfqvist and coworkers (2006) have verified the program's ability to provide early and accurate identification of children with the greatest risk of developing the disease ROP in a new follow-up study of extremely preterm children (Löfqvist et al. 2009). A further development and significant simplification of this program has resulted in monitoring of the children's postnatal weight gain only in order to predict the development of severe ROP. This simplified approach was recently published and confirmed that WINROP correctly identified the very premature children at high risk of developing severe ROP (approx. 15%) and also correctly excluded those children who did not develop the disease (approximately 75%) (Löfqvist et al. 2009). In addition, we have successfully validated WINROP in cooperation with the neonatal/ophthalmology wards at Brigham and Women in Boston (Wu et al. 2010) and at the Departments of Ophthalmology and Pediatrics, Hospital de Clínicas de Porto Alegre, Federal University of Rio Grande do Sul, Brazil (Hård et al. 2010). WINROP provides a tool to identify infants at risk for sight threatening ROP. We believe that additional NICU data from developing countries will help in modifying the algorithm for these populations. The close association between poor neonatal weight development and ROP indicates that optimizing growth may be one way to reduce ROP. Conclusions In summary, for decades neonatal intensive care has focused on survival of the most immature babies. The time has now come to find ways to optimize weight development and normalize growth of vital structures such as vessels and neurons. References Davenport ML, D'Ercole AJ, Underwood LE (1990): Effect of maternal fasting on fetal growth, serum insulin-like growth factors (IGFs), and tissue IGF messenger ribonucleic acids. Endocrinology, 126: 2062-7. Engström E, Niklasson A, Albertsson Wikland K, Ewald U, Hellström A (2005): The role of maternal factors, postnatal nutrition, weight gain and gender in regulation of serum IGF-I among preterm infants. Pediatric Research, 57: 605-10. Hansen-Pupp I, Hellström-Westas L, Cilio CM, Andersson S, Fellman V, Ley D (2007): Inflammation at birth and the insulin-like growth factor system in very preterm infants. Acta Paediatr, 96: 830-6. Hellström A, Carlsson B, Niklasson A, Boguszewski M, De Lacerda L, Savage M, Svensson E, Smith LE, Weinberger D, Albertsson-Wikland K, Laron Z (2002): Insulin-like growth factor I is critical for normal vascularisation of the human retina. Journal of Clinical Endocrinology and Metabolism, 87: 3413-3416. Hellström A, Engström E, Hård A-L, Albertsson-Wikland K, Carlsson B, Niklasson A, Löfqvist C, Svensson E, Holm S, Ewald U, Holmström G, Smith LE (2003): Postnatal serum insulin-like growth factor I deficiency is associated with retinopathy of prematurity and other complications of premature birth. Pediatrics, 112: 1016-1020. Hellström A, Hard AL, Engström E, Niklasson A, Andersson E, Smith L, Lofqvist C (2009): Early weight gain predicts retinopathy in preterm infants A new simple and efficient approach to screening. Pediatrics, 123: 638-45. Hellström A, Peruzzi C, Ju M, Engström E, Hård A-L, Lui J-L, Albertsson-Wikland K, Carlsson B, Niklasson A, Sjödell L, LeRoith D, Senger D, Smith LE (2001): Insulin-like growth factor-I is critical to retinopathy of prematurity. Proceedings of the National Academy of Science, 98: 5804-5808. Hård AL, Löfqvist C, Borges JFF, Soibelmann Procianoy R, Smith L, Hellström A (2010): The new screening algorithm named WINROP predicts proliferative retinopathy in a Brazilian population of preterm infants. Arch Ophthalmol, in press. Hök Wikstrand M, Hård A-L, Niklasson A and Hellström A (2009): Birth weight deviation and early postnatal growth are related to optic nerve morphology at school age in very preterm children. Pediatr Res, 67: 325-9. Hök Wikstrand M, Hård A-L, Niklasson A and Hellström A (2010): Postnatal growth variables are related to morphologic and functional ophthalmologic outcome in children born preterm. Acta Ped, 99: 658-64. Jacobson L, Hård A-L, Hammarén H, Hellström A (2009): Visual outcome in children born less than 25 gestational weeks. Acta Ped, 98:261-5. Lopez-Lopez C, LeRoith D, Torres-Aleman I (2004): Insulin-like growth factor I is required for vessel remodeling in the adult brain. Proc Natl Acad Sci, 101: 9833-8. Löfqvist C, Engström E, Sigurdsson J, Hård A-L, Niklasson A, Ewald U, Holmström G, Smith LE, Hellström A (2006): Postnatal head growth deficit in premature infants parallels retinopathy of prematurity and Insulin-like growth factor-I deficit. Pediatrics, 117: 1930-1938. Löfqvist C, Andersson E, Sigurdsson J, Engström E, Hård AL, Niklasson A, Smith LE, Hellström A (2007): Longitudinal postnatal weight and insulin-like growth factor I measurements in the prediction of retinopathy of prematurity. Arch Ophthalmol, 124: 1711-8. Erratum in: Arch Ophthalmol, 125: 426. Löfqvist C, Hansen-Pupp I, Andersson E, Holm K, Smith L, Ley D, Hellström A (2009): Validation of a new ROP screening method monitoring longitudinal postnatal weight and IGF-I. Arch Ophthalmol, 127: 622-7. Vanhaesebrouck S, Daniëls H, Moons L, Vanhole C, Carmeliet P, De Zegher F (2009): Oxygen-induced retinopathy in mice: amplification by neonatal IGF-I deficit and attenuation by IGF-I administration. Pediatr Res, 65: 307-10 Wallace DK, Kylstra JA, Phillips SJ, Hall JG (2000): Poor postnatal weight gain: a risk factor for severe retinopathy of prematurity. J AAPOS, 4: 343-7. Wu C, Vanderveen D, Hellstrom A, Löfqvist C, Smith L (2010). Longitudinal postnatal weight measurements for the prediction of retinopathy of prematurity. Arch Ophthalmol, in press. Ye P, D'Ercole AJ (2006): Insulin-like growth factor actions during development of neural stem cells and progenitors in the central nervous system. J Neurosci Res, 83: 1-6. IX Prematurity and the Eye Gerd Homlström Introduction Prematurely born children have an increased risk to develop visual and eye problems compared to children born at term. In the neonatal period they may develop retinal disease, while later there is a risk of various visual dysfunctions. Retinopathy of Prematurity (ROP) Retinal disease in prematurely born infants was first decscibed by Terry in the beginning of the 1940ies and was given the name Retrolental fibroplasia (RLF). In the middle of the 1980ies the disease was given a new name, Retinopathy of prematurity (ROP), and a new classification by an international committee. ROP was divided into five stages, where stage 5 represents a total retinal detachment and a blind eye. Recently, a revised classification has been presented (ICROP 2005), describing aggressive and rapidly progressing ROP in the most immature infants. Without adequate treatment this type of ROP most often leads to progression to stage 5 ROP and blindness. ROP stages 2 and 3 and Aggressive ROP are illustrated in Figure 1. Early stages of ROP (ROP 1 and 2) often regress spontaneously, while more severe stages need treatment to prevent retinal detachment. In the 1970ies, treatment of the peripheral retina with so-called cryo therapy was introduced, to destroy the anoxic part of the eye that was stimulating the deleterious production of growth factors and vascular proliferations. In the 1990’s laser treatment has become the method of choice. Laser therapy is also a destructive method, but more beneficial for the eye. Given at a correct time, it is successful in most cases of ROP. If retinal detachment occurs, so-called vitrectomy may be performed. In the most advanced cases with total retinal detachment (ROP stage 5), the chance of useful visual function is, however, negligible regardless of surgical method. A. B. C. D. Figure 1. Normal fundus, including retina, optic disc and vessels (A). ROP stage 2, including ridge at the border between vascularised and non-vascularized retina (B). ROP stage 3, including vascular proliferations (C). Aggressive posterior ROP (D). (ICROP 2005) Incidence of ROP The incidence of ROP is related to the quality of neonatal care. In poor countries almost no ROP occurs since prematurely-born infants rarely survive. In middle-income countries with an increasing survival, there is a new epidemic of ROP leading to severe visual impairments and blindness. In Sweden several population-based studies on the incidence of ROP have been performed during the last decades. Twenty years ago we reported an ROP incidence of 40% in infants with a birth weight of 1500 grams or less born in the Stockholm County during the years of 1988 to 1990 (Holmström et al 1993). A new study in exactly the same geographical area 10 years later, revealed a similar incidence but a change in the distribution of ROP. The more ”mature” infants had a reduced incidence of ROP, while the most immature babies, previously not surviving, had the highest risk of ROP and particularly severe ROP, see figure 2. (Larsson et al 2002). Figure 2. Probality of ROP in relation to gestational age at birth (weeks) in two consecutive studies on ROP (1988 to 1990 and 1998 to 2000, respectively) in the Stockholm area of Sweden (Larsson et al 2002). During the last decade, improvements in neonatal care have resulted in a new population of extremely immature babies with a high risk of various complications. A recent study enclosing all infants in Sweden born before 27 weeks of gestations from 1 April 2004 to 31st March 2007, revealed that 70% of the infants survived up to one year of age (EXPRESS Group 2009). Major morbidities , i.e. intraventricular haemorrhage, broncopulmanry dysplasia and / or ROP, were found in 45 % of these infants. The ophthalmic data were separately collected and analysed. We recently reported that 73% of this population developed ROP; mild ROP in 38 % and severe ROP in 35 % (Austeng et al 2009). Treatment was performed in 20% of the infants. The most immature infants had the highest risk to develop ROP and to reach treatment criteria, and they also developed ROP earlier and were treated earlier than those born at a slightly higher gestational age (Austeng et al 2009). Screening for ROP ROP is one of the few causes of childhood blindness, which in most cases can be prevented. Screening for ROP with repeated eye examinations in the neonatal period is therefore of utmost importance for detection of severe ROP and for initiation of treatment at a correct time. Since the incidence of ROP is related to the neonatal care and socio-economic situation of the country, guidelines for screening have to be adapted to the country per se. In Sweden, the first national guidelines were suggested after the population-based study in 1988-1990 (Holmström et al 1993). ROP screening was recommended to include all infants born before 33 weeks of gestation and to start at 5 to 6 weeks of life and continue with one to two weeks interval up to term or until regression of ROP. In case of progressing ROP, the intervals between examinations were reduced and treatment was performed if indicated. Based on the results of the incidence study in the Stockholm area during 1998 to 2000, modification of screening recommendations with reduction of inclusion criteria to infants born before the 32nd week of gestation were proposed (Larsson & Holmström 2002). Analyses of the natural history of ROP in infants with a gestational age of less than 27 weeks at birth have revealed new information on the importance of time and retinal location of ROP at onset of the disease (Austeng et al 2010). These findings will probably lead to modifications of the screening guidelines in the group of extremely preterm infants. To further improve the quality of ROP screening, a national web based register for ROP, the so-called SWEDROP, has been developed (www.swedrop.se). The register was started in late 2006, has a steering group of six regional responsible ophthalmologists and today has a cover of around 80% of the prematurely-born infants in the country. In the near future we hope to have reliable data to further modify and improve the screening guidelines, leading to improved outcome for the infants. Other ophthalmological sequels in prematurity Retinopathy of prematurity (ROP) is a neonatal complication of the eye. Long-term follow-up studies in childhood and adolescence, however, have revealed various visual dysfunctions in prematurely-born children. Population-based studies on children of 10 years age in Denmark, United Kingdom and New Zealand have reported increased risks to develop refractive errors, strabismus, visual field defects, contrast sensitivity defects, and visual perceptual deficits. Children from the population-based study in Stockholm during 1988 to 1990 have been followed up repeatedly up to 10 years age (Holmström et al 1998, 1999). At that age, an extensive ophthalmological follow-up was performed together with a similar group of children born at term in the same geographical area. The visual acuity was found to be reasonable in a majority of the preterm children and only 2 % had a visual impairment (≤ 0.3), while a significant proportion had a subnormal visual acuity (Larsson et al 2005). Contrast sensitivity was slightly, but significantly, reduced (Larsson et al 2006), strabismus was much commoner (Holmström et al 2006), visual fields were slightly reduced (Larsson et al 2004) and refractive errors (Larsson 2003, Holmström et al 2005, Larsson et al 2006) were much more common in the preterm children compared to those born at term. The various ophthalmologic sequels were most common in children with previous severe ROP and with neurological problems, but also the children without such complications had an increased risk to develop ophthalmic problems. Finally, our studies revealed a significant correlation between visual dysfunction at 10 years and various school problems (Holmström & Larsson 2008). Ophthalmological follow-up in prematurely-born children As illustrated above, prematurely-born children indeed have an increased risk to develop various ophthalmological problems and dysfunctions. Major sequelae are well-known, while more subtle dysfunctions recently have been reported to affect the quality of life of these children. Hence, the question arises if these children ought to be offered a long-term followup, and in that case, which children and when and by whom. There is no consensus in the literature, but some authors suggest frequent follow-up of all prematurely-born children during childhood, some suggest follow-up of all children with ROP, while some propose follow-up of only those with severe ROP and neurological sequealae. The Stockholm children born in 1988 to 1990 had been followed up repeatedly up to 10 years, giving us the possibility to evaluate risk factors which could predict visual dysfunction at 10 years. Multiple regression analyses revealed that, apart from children who had been treated for ROP and children with neurological sequelae, also those with significant refractive errors (anisometropia and astigmatism) at 2.5 years, had an increased risk to develop visual dysfunction, according to our definition, at 10 years of age (Holmström&Larsson 2008). Based on our findings, we recommend that children who have been treated for ROP and children with obvious neurological lesions have a regular ophthalmic follow-up. Regarding the children with untreated ROP and without ROP, we propose that at least one follow-up is offered at around 2.5 years when the refraction is stabilized and amblyopia, with or without strabismus, is still treatable. This examination can preferably be performed by an orthoptist with a possibility to refer to a paediatric ophthalmologist, when indicated. Conclusions Prematurely-born infants and children are a risk group for various visual and ophthalmological problems. Screening programmes to detect and treat these children are necessary, but will continuously need to be modified parallel to new achieved knowledge. An upcoming 6.5-year follow-up of the Swedish cohort of 500 extremely preterm infants born before 27 weeks of gestation will hopefully provide us with new knowledge of the visual function in this group of children. References Austeng D, Källen K, Ewald U, Jakobsson P & Holmström G (2009). Incidence of retinopathy of prematurity in infants born before 27 weeks' gestation in Sweden. Arch Ophthalmol, 127:1315-9. Austeng D, Källen K, Ewald U, Wallin A & Holmström G (2009). Treatment of ROP in a population of extremely preterm infants born before the 27th week of gestation in Sweden. Br J Ophtalmol, Nov 30, Epub ahead of print. Austeng D, Källn K, Hellström A, Tornqvist K & Holmström G (2010): Natural history of ROP in a population of extremely preterm infants born before the 27th week of gestation in Sweden. Arch Ophthalmol, In press. EXPRESS group (2009): One-year survival of extremely preterm infants after active perinatal care in Sweden. JAMA, 301: 2225-2233. Holmström G, el Azazi M, Jacobson L & Lennerstrand G (1993): A population based, prospective study of the development of ROP in the Stockholm area of Sweden. Br J Ophthalmol, 77: 417-23. Holmström G, el Azazi M & Kugelberg U (1998): Ophthalmological follow-up of preterm infants - a population-based study of the refraction and its development. Br J Ophthalmology, 82: 1265-71. Holmström G, el Azazi M, Kugelberg U. Ophthalmological follow-up of preterm infants - a population-based study of visual acuity and strabismus (1999). Br J Ophthalmology, 83: 14351. Holmstrom GE & Larsson EK (2005): Development of spherical equivalent refraction in prematurely born children during the first 10 years of life: a population-based study. Arch Ophthalmol, 123: 1404-11. Holmström G, Rydberg A & Larsson E (2006): Strabismus and its development in 10-yearold prematurely-born children – a population-based study: J Pediatr Ophthalmol Strabismus, 43:346-52. Holmström G & Larsson E (2008): Longterm follow-up of visual functions in prematurelyborn children – a prospective population-based study up to 10 years of age. JAAPOS, 12:157162. International Commitee for the Classification of Retinopathy of Prematurity (ICROP) (2005). The International Classification of retinopathy of prematurity Revisited. Arch Ophthalmol, 123: 991-999. Larsson E, Carle-Petrelius B, Cernerud G, Ots L, Wallin A & Holmström G (2002): Incidence of ROP in two consecutive population-based studies. Br J Ophthalmology, 86: 1122-26. Larsson E & Holmström G (2002): Screening for ROP – evaluation and modification of guidelines. Br J Ophthalmology, 86: 1399-1402. Larsson E, Rydberg A & Holmström G (2003): A population-based study of the refractive outcome in 10-year-old preterm and full-term children. Arch Ophthalmol, 121: 1430-1436 Larsson E, Martin L & Holmström G (2004): Peripheral and central visual fields in 11 year old children who had been born prematurely and at term. Pediatric Ophthalmol Strab, 41: 3945 Larsson EK, Rydberg AC & Holmstrom GE (2005): A population-based study on the visual outcome in 10-year-old preterm and full-term children. Arch Ophthalmol, 123: 825-32. Larsson E, Rydberg A & Holmstrom G (2006): Contrast sensitivity in 10 year old preterm and full term children: a population-based study. Br J Ophthalmol, 90: 87-90. Larsson EK & Holmström GE (2006): Development of astigmatism and anisometropia in preterm children during the first 10 years of life. Arch Ophthalmol, 124: 1608-14. X Visual Function and Ocular Findings in Children with Pre- and Perinatal Brain Damage Lena Jacobson Introduction Children with visual impairment due to damage to the retro-geniculate visual pathways constitute an increasing group among visually impaired children in the Western world. The developing visual system may be affected by malformations arising early in gestation, by white matter damage of immaturity (WMDI) both in utero and as a sequel to premature birth, and by asphyxia as well as by cortical-subcortical damage due to perinatal cerebral infarcts in children born at term. Infections and trauma in the neonatal period may also affect the visual system. Much of the brain is devoted to vision. Damage causes visual problems ranging from profound impairment to cognitive visual problems only. Visual and ocular outcome after pre- or perinatal brain damage depends on localisation and extension of the lesion, but also on at what stage the developing system was injured. Plasticity of the brain may modify the functional outcome when the visual system is injured early in gestation Thus, reorganisation of the visual system by bypassing the lesion in the ipsilateral hemisphere or maybe by inter-hemispheric reorganisation may take place in the immature brain. In addition, retrograde trans-synaptic degeneration may affect the appearance of the optic disc in retro-geniculate lesions occurring during the pregnancy or in the neonatal period in children born preterm. Brain imaging techniques Examination of the newborn infant brain with ultrasound (US) may detect lesions engaging the posterior visual pathways, but US is an insensitive method to find minor injuries. Later during infancy and childhood magnetic resonance imaging (MRI) is the most sensitive imaging modality to detect permanent lesions to the posterior visual system. The paediatric neuroradiologist thus plays an important part in the identification of children with cerebral visual impairment. White matter lesions may be further understood and mapped out with diffusion tensor imaging techniques. Visual dysfunctions The manifestations of this kind of visual impairment include subnormal visual acuity and crowding, affected visual field function and associated disorders of higher visual processing. The principal cognitive visual pathways comprise the dorsal and the ventral streams. The dorsal stream runs between the occipital lobes, which process incoming visual data, the posterior parietal lobes, which process the whole visual scene and give attention to component parts, the motor cortex, which facilitates movement through the visual scene and the frontal cortex, which directs attention to chosen parts of the visual scene. The ventral stream runs between the occipital lobes and the temporal lobes, which enable recognition of people and objects facilitating route finding and serve visual memory. In addition, impaired control of the eye movements and disordered focusing may further complicate the effective use of vision. These problems can occur in any combination and severity. Visual function may improve over time. Cerebral palsy, learning disabilities and behaviour and attention problems are other wellknown consequences of pre- and perinatal brain damage. Concomitant cerebral visual impairment is common but often remains undetected, and therefore is not taken into account when designing habilitation programs for the individual child. Early brain damage may however cause only visual problems, and often manifests itself as early-onset strabismus. In these cases, the paediatric ophthalmologist is responsible for identification of children with cerebral visual impairment, for assessment of visual function, and for initiating habilitation. The habilitation of these children demands a multi-disciplinary team including paediatric ophthalmologist, orthoptist, neuropsychologist, paediatric neurologist, occupational therapist, physiotherapist, low vision teacher and remedial teacher. Our research team at Karolinska Institutet has in collaboration with researchers from Gothenburg during the years 1996-2009 contributed to the bank of new knowledge of visual and ocular outcome in children with pre- and perinatal brain damage. Prematurely born children with WMDI Crowding and cognitive visual problems in children with WMDI In a study of prematurely born children with visual impairment due to WMDI, we described subnormal visual acuity and crowding (Jacobson et al 1996). Using standard neuropsychological tests we described visuo-spatial deficiencies in this group with problems judging depth and movement, with simultaneous perception, with face recognition and with orientation. Other groups described similar findings; among them Dutton et al. 1996. Nystagmus, eye motility disorders, strabismus in children with WMDI Nystagmus was previously reported to be absent in children with cerebral visual impairment. In fact, the presence or absence of nystagmus was thought to reveal whether the cause of visual impairment in a child was of ocular or cerebral origin. In the 1990ies we studied fixation with infrared technique in a group of prematurely born children with cerebral visual impairment due to WMDI and reported latent or manifest nystagmus in a majority of these children (Jacobson et al. 1998). However, children with the most severe WMDI, with cerebral palsy and visual impairment presented an ocular motor apraxia with complete disruption of ocular motor organization, including absence of fixation and they had no nystagmus. Children with less extensive WMDI, representing the other end of the clinical spectrum, all exhibited nystagmus. Thus, nystagmus may be seen in children with cerebral visual impairment and the presence of nystagmus may depend on the extent, and maybe, on the timing of the insult which may affect input to the visual integrating circuits. Defective smooth pursuit movements and inability to perform visually guided saccadic movements in children with WMDI were found by us and by Cioni et al (1997) and Lanzi et al (1998). Strabismus as a consequence of WMDI was reported by Scher et al (1989) and also by us. The frequent finding of early-onset strabismus associated to WMDI may be the consequence of a deficient afferent pathway caused by axonal interruption in the optic radiation. Optic disc appearance in children with WMDI Brodsky and Glasier (1993) found a link between optic nerve hypoplasia and WMDI, but did not confirm their observations by fundus photography. We performed digital analysis of the fundus photographs of children with WMDI and found that the time at which the primary lesion of the optic radiation occurred was of importance for the appearance of the optic disc (Jacobson et al. 1997, Jacobson et al. 2003). Early WMDI, sometimes of prenatal origin, before gestational week 28 was associated with small discs. Normal-sized optic discs with large cupping and consequently a reduced neuro-retinal rim area was the consequence of later lesions, occurring after 28 weeks of gestation. In this developmental phase, the supportive structures of the optic nerve have become established and probably do not adapt to the smaller number of nerve fibers. The reduced rim area, either expressed as a small disc or as a large cup in a normal-sized disc is probably the result of retrograde trans-synaptic degeneration of optic nerve axons caused by the primary bilateral lesions in the optic radiation. Thus, optic disc appearance together with the pattern of cerebral morphology depicted by MRI may give information about the timing of the lesion. Visual field defects in children with WMDI Interruption of axons in the optic radiation may explain restriction of visual field (VF). Variable restriction of the fields may also be attributable to problems with simultaneous attention. Thus the functional VF may vary depending on the amount of visual stimuli present and on the degree of attention paid to the fixation target. We assessed VF function in a group of children with WMDI (Jacobson et al. 2006). All subjects had subnormal VF function, although the depth and extension of the defects differed between subjects. The lower VF was often more affected than the upper, which could be interpreted as a bilateral homonymous lower quadrant dysopia due to the bilateral lesions in the upper part of the optic radiation. The VF abnormalities could be demonstrated by both manual and computerized perimetry. Case report This case illustrates visual outcome associated to WMDI (Jacobson & Dutton 2000). A boy was born prematurely at 32 full gestational weeks, with asphyxia at birth and he was early diagnosed with cerebral palsy (spastic diplegia). His verbal development was normal.Visual function is characterized by normal visual acuity (RE=LE 1.0) inferior altitudinal visual field defects (Fig. 1), strabismus, nystagmus, defect saccades and smooth pursuit movements and severe dorsal and ventral stream dysfunction. Thus, he is not able to judge depth by vision, he cannot find his way around and he cannot recognise even family members if he meets them unexpectedly. He is a slow reader, and often gets lost in the text. He has developed a battery of compensating strategies based on hearing, tactile information and memory. The optic discs are of normal size with large cupping (Fig. 2); the intraocular pressure is normal. GDx of the fundus (Fig. 3) documents loss of ganglion cell axons above the optic disc secondary to the brain lesions. MRI of the brain (Fig. 4 and 5) illustrates bilateral periventricular WMDI. With fiber tractography of the optic radiation (Fig. 6) connecting fibres are only detectable in the lower part of optic radiation on both sides which corresponds well with the finding of an inferior bilateral homonymous quadrant anopia. Figure 1. Altitudinal inferior visual field defects (bilateral inferior homonymous quadrant anopias) due to bilateral WMDI affecting the upper parts of the optic radiations. Figure 2. Large cupping of normal-sized optic discs; a consequence of retrograde transsynaptic degeneration from interruption of axons in the optic radiation occurring after 28 gestational weeks. Figure 3. GDx fundus images illustrating loss of nerve fibres layer above the optic discs, due to retrograde trans-synaptic degeneration from the lesions in the upper part of both optic radiations, corresponding to the visual field defects Figure 4. This MRI at the level of the posterior horns and trigonum shows the occipital horns to be dilated due to reduced periventricular white matter volume and consequent loss of axons in motor and visual pathways. Note how cortex abuts the ventricular wall giving trigonum of the ventricles a slight irregular shape. Also note increased signal in remaining white matter adjacent to the frontal horns and extending deep into white matter in both frontal lobes. (Courtesy of Olof Flodmark, Dept of Neuroradiology, Karolinska University Hospital) Figure 5. This image is at a level just at the top of the lateral ventricles. Increase signal beyond the borders of the lateral ventricles in the parietal and frontal lobes represent gliosis in damaged white matter. (Courtesy of Olof Flodmark, Dept of Neuroradiology, Karolinska University Hospital) Figure 6. Fiber tractography of the optic radiation (OR). It is difficult to accurately track the OR with tensor-based tracking. Here, instead tractography between LGN and primary visual cortex is performed with probabilistic tractography in a crossing-fiber model. The results show a normal periventricular extent of OR in a healthy volunteer (Left). In our case (Right) connecting fibers are only detectable in the lower part of OR. The degree of connectivity is also lower (i.e. lower probability that initiated fibers in LGN reach the target area in primary visual cortex), and more so on his left than on his right .side. This finding corresponds well with loss of nerve fibres in the upper part of the fundi and with an inferior bilateral homonymous quadrant anopia. (Courtesy of Annika Kits and Finn Lennartsson, Dept of Neuroradiology, Karolinska University Hospital) Visual field outcome in children with unilateral cerebral palsy The frequency of VF defects in different groups of children with cerebral palsy has been estimated to 20-25%. However, in most studies only confrontation techniques have been used. We have recently assessed VF function in a group of children with unilateral cerebral palsy (CP) with confrontation technique and with Goldmann perimetry. The type and extension of brain lesion was documented with cerebral imaging. 62% had subnormal VF function, and the VFs were severely restricted in 21%. The underlying brain lesions were malformation, WMDI and cortico-subcortical lesions. VF function could be correlated to the pattern of brain damage in cortico-subcortical lesions and in extensive lesions due to malformation or WMDI. Total homonymous hemianopia was common in the cortico-subcortical group but rarely found in children with malformation or WMDI. Five children had malformation or WMDI engaging parts of the brain that usually contain the posterior visual system, but they had normal VF function. Thus, the VF function may be preserved by plasticity of the immature brain in children with malformation and WMDI. Severely restricted VF function was more often associated with brain damage occurring later in the developing brain. All children with severely restricted VFs were identified with confrontation technique. Goldmann perimetry was a suitable method to identify also relative VF defects in this age group of children with unilateral CP (Jacobson et al. 2010). Conclusions Visual impairment due to pre-and perinatal brain damage has become the most common cause of visual disturbance among children in the Western world; a consequence of increased survival of very immature and very sick infants. The resulting visual dysfunction depends on localisation and extension of the lesion involving the visual brain, but also on at what stage of maturity the brain was damaged. As there is considerable plasticity of the developing visual system, the outcome may be difficult to predict by routine imaging of the brain. Assessments of acuities, visual field function, fixation, eye motility and of cognitive visual function constitute the basis for implementation of developmental programmes designed for these children. References Brodsky M & Glasier (1993): Optic nerve hypoplasia: clinical significance of associated central nervous system abnormalities on magnetic resonance imaging. Arch Ophthalmol 111: 66-74. Cioni G, Fazzi B, C et al. (1997): Cerebral visual impairment in preterm infants with periventricular leukomalacia. Pediatr Neurol 17: 331-8. Dutton G, Ballantyne J, Boyd G et al. (1996): Cortical visual dysfunction in children. Eye (London) 10: 302-9. Jacobson L & Dutton G (2000): Periventricular leukomalacia: an important cause of visual and ocular motility dysfunction in children. Surv Ophthalmol 45: 1-13. Jacobson L. Ek U, Fernell Eet al. (1996): Visual impairment in preterm children with periventricular leukomalacia – visual, cognitive and neuropaediatric characteristics related to cerebral imaging. Dev Med Child Neurol 38: 724-36. Jacobson L, Flodmark O & Martin L. (2006): Visual field defects in prematurely born patients with white matter damage of immaturity; a multiple case study. Acta Ophthalmol Scand 84: 357-62 Jacobson L, Hellström A & Flodmark O (1997): Large cups in normal-sized optic discs. A variant of optic nerve hypoplasia in children with periventricular leukomalacia. Arch Ophthalmol 115: 1263-9 Jacobson L, Hård AL, Svensson E, et al. (2003): Optic disc morphology may reveal timing of insult in children with periventricular leukomalacia and/or periventricular haemorrhage. Br J Ophthalmol 87: 1345-9 Jacobson L, Rydberg A, Eliasson AC et al. submitted manuscript. Visual field function at school age in children with spastic unilateral cerebral palsy, related to different patterns of brain damage Jacobson L, Ygge J & Flodmark O (1998): Nystagmus in periventricular leucomalacia. Br J Ophthalmology 82: 1026-32. Lanzi G, Fazzi E, Uggetti CD, et al. (1998): Cerebral visual impairment in periventricular leukomalacia. Neuroped 29: 145-50. Sher M, Dobson V, Carpenter N, et al. (1989): Visual and neurological outcome of infants with periventricular leukomalacia. Dev Med Child Neurol 31: 353-65. XI The Eye Mirroring Inherited Metabolic Disorders Kristina Teär Fahnehjelm Introduction A few decades ago many children with inborn errors of metabolism died early. Today, with better diagnostic procedures and more efficient treatment they often reach adulthood. However, somatic or ocular complications are common as long-term sequels. Early diagnosis does not make already existing ocular complications vanish but often, although not always, treatment can stop progression. It is therefore important for the paediatric ophthalmologist to be acquainted with the pathogenesis of metabolic disorders and to get a good knowledge of how, why and when the eyes are affected. Although the individual inherited inborn errors of metabolism are rare diseases, taken as a group, they affect approximately 1 child per 2500. In the following a few common inherited metabolic disorders with severe ocular complications are presented. Mucopolysaccharidosis I (MPS I) Hurler Mucopolysaccharidoses are lysosomal storage diseases, due to deficiencies of different enzymes, where MPS I - Hurler is the most common. It is a life-threatening disease where corneal clouding can be one of the first presenting signs and thus also a diagnostic clue. The world wide incidence of MPS I has been reported to be 1/100 000 newborns. More than 90 mutations in the gene coding for the lysosomal enzyme α-L-iduronidase are known to cause deficiency or absence of the enzyme. This abnormality leads to intra- and extracellular accumulation of the glucosaminoglucans (GAG), causing cell death, tissue damage and disturbance of normal tissue growth as well as excessive excretion of GAG in the urine. The children, who usually grow normally until six months of age, will manifest severe skeletal deformations, short stature, scoliosis, coarsening of facial features, large heads, communicating hydrocephalus, mental retardation, hepatosplenomegaly, and cardiac complications. Death, in untreated children, usually occurs during the first decade of life (Wraith 2005). Ocular characteristics apart from corneal clouding (Figure 1) include protruding wide set eyes, atypical eyebrows, retinal dystrophies, glaucoma, chronic papilloedema and optic atrophy. Also posterior visual pathway pathology or visual cortical abnormalities have been reported due to accumulation of storage material in the white matter of the CNS. Early allogeneic stem cell transplantation (SCT), where a HLA matched graft is given to a conditioned patient, has been used as a treatment since the early 1980-ies. SCT has been shown to reduce the accumulation of GAG in visceral organs and to increase survival and stabilising long-term neuro-cognitive functions. Today SCT is offered to children below two years of age with a normal intellectual development (Wraith 2005) but SCT performed even earlier, at 12 months of age, is preferable. With regard to eye symptoms, various degrees of improvement of the corneal clouding after SCT have been reported. However, despite early improvement of retinal conditions with SCT, it has been suggested that retinal dysfunction will still progress (Gullingsrud et al. 1998). As life expectancy increases in children with MPS I-H, it becomes more important to detect remaining ocular complications and additional SCT related complications, such dry eye syndrome and cataract. In a Swedish study corneal opacities diminished in four children with MPS I (one of them shown in Figure 2), after SCT before 2 years of age (Fahnehjelm et al. 2006). Although early SCT thus seems to be beneficial, no objective grading of the corneal opacities was made and the number of patients was limited. In accordance with previous studies, no patient had a complete resolution of the corneal opacities. However, the best corrected visual acuity (BCVA) was good in these 4 patients, in comparison with patients in other international studies, partly maybe due to early intervention with glasses for hyperopia. No patient has needed corneal transplantation, developed cataract and/or glaucoma. A recent follow-up has been made of five of seven Swedish patients with MPS I who had SCT before 23 months of age. The median age in the group was 8 years, BCVAwas ≥ 0.5 in the majority of the patients despite mild/moderate opacities while high hyperopia (+4.0 to +9.0 spherical equivalent) was present in all patients. Keratometry values were low and axial lengths short in comparison with reference material (Fahnehjelm, Törnquist& Winiarski accepted ACTA Ophthalmol April 2010) Our hypothesis is that the storage of GAG will lead to increased rigidity of the cornea and sclera, with a flattening of the curvature of the cornea and a reduction of the refractive power of the corneal surface. This, together with the reduced axial length, can explain the high incidence of hyperopia in the MPS I patients. Detection of refractive errors and prescription of glasses are important in order to avoid amblyopia. Photochromatic glasses were shown to be beneficial in minimizing photophobia, increasing comfort and optimizing visual function. To conclude, children with MPS 1-H show a variety of ocular symptoms. Early SCT seems beneficial in reducing, but not eliminating, corneal opacities. The clinical evaluation of MPS I children in their early years offers a challenge to the paediatric ophthalmologist. Retinoscopy might be difficult to perform due to dull fundus reflexes and/or severe photophobia but is important to measure the refraction since high hyperopia is common. It is possibly caused by storage of glucasaminoglucans that affect the refractive power of the cornea. Intraocular pressure is often recorded as falsely high, due to corneal stiffness. In the future, stromal transplantation of mesenchymal cells might be a solution for reduction of corneal opacities. Enzyme replacement therapy has so far not been shown beneficial in reducing corneal opacities, probably due to reduction of enzyme transport to the avascular cornea. Long-chain 3-hydroxyacyl-CoA dehydrogenase (LCHAD) deficiency LCHAD (Long-chain 3-hydroxyacyl-CoA dehydrogenase) deficiency is a life-threatening disorder of deficient fat metabolism. The LCHAD enzyme catalyzes the β-oxidation of fatty acids and has the highest specificity towards chain lengths of 14-22 carbon atoms. The disease is inherited in an autosomal recessive manner and is the second most common β-oxidation defect in Sweden with an estimated incidence of 1:100.000. As triglycerides offer an important source of energy, a defect in the degradation can have deleterious effects during catabolic states. The diagnosis is usually established within the first eight months of life, based on life threatening hypoketotic hypoglycaemia accompanied by liver enlargement, muscular hypotonia and hypertrophic cardiomyopathy. Measurements of dicarboxylic and 3-hydroxy fatty acids in plasma followed by mutation analysis contribute to the diagnosis. Emergency treatment with glucose infusion followed by a diet with reduced intake of fat (approximately 20% of calories), mainly composed of medium chain triglycerides, supplemented with vitamins, minerals and essential fatty acids, has resulted in reversion of the above symptoms. Neonatal death is a major risk. The surviving children have a fasting intolerance making night feeds necessary in the majority of cases and necessitating hospital care and glucose infusion during febrile infections. Long-term complications include peripheral neuropathy, mental retardation and chorioretinopathy. Flattened and hypopigmented retinal pigment epithelium cells and secondary loss of choriocapillaris macrophages have been demonstrated in the central parts, while the peripheral parts of the ocular fundii have been normal (Tyni et al. 1998b). The retinal findings can be graded: Stage 1 is a normal/ pale fundus with normal visual acuity and electroretinograhy (ERG); Stage 2 a fundus with clumping of the retinal pigment epithelium in the posterior pole and ERG deterioration(Figure 3); Stage 3 a fundus with progression to chorioretinal atrophy , and Stage 4 a fundus with additional posterior staphyloma and extinguished ERG (Tyni et al. 1998a). Presently, there are 12 living children diagnosed with LCHAD deficiency in Sweden. One patient has been treated for 18 years and is one of the longest treated worldwide. Ten of the patients have been included in our study (Fahnehjelm et al. 2007). They all showed chorioretinal changes of different severity. This is a higher frequency than previously reported and may be explained by a longer ocular follow-up. Hence, the present regimen seems not to prevent but possibly to delay the development of ocular symptoms. The ERG responses correlated with the stages of chorioretinopathy, suggesting that disturbance of the retinal neuro-epithelium paralleled the damage of the retinal pigment epithelium and the progressive loss of choroid vessels. All patients were treated with Omega 3 (docosahexaenoic acid /DHA/) to keep DHA within normal levels. Low plasma levels of essential fatty acids, especially DHA, have previously been suggested as a contributing factor for the retinopathy (Gillingham et al. 1999). A correlation between DHA levels and VA measured by Sweep VEP (Gillingham et al. 2005) has been seen in these children. The accumulation of long-chain 3-hydroxyacylcarnitines has also been found to be negatively correlated to ERG amplitude (Gillingham et al. 2005). In conclusion, children with LCHAD-deficiency should have an ocular examination within the first month of diagnosis and thereafter annually. The ophthalmologist has an important role in early detection, since LCHAD deficiency may be difficult to diagnose. Unusual chorioretinal findings, especially if there is a history of neonatal hypoglycaemia or failure to thrive, should lead to the suspicion of LCHAD deficiency. Fundus photography and repeated ERGs should be performed. Furthermore, it is important that an ocular evaluation is done of all patients with a suspected defect in the beta oxidation system. Mitochondrial diseases Mitochondrial diseases lead to dysfunction of the respiratory chain affecting the cellular energy metabolism of all organs, giving rise to a variety of symptoms from any organ at all ages. With an estimated minimum prevalence of 1/5000 the mitochondrial diseases can be regarded as one of the most common groups of inborn errors of metabolism. The respiratory chain consists of five enzyme complexes (I-V) located in the mitochondrial inner membrane with the main function to generate adenosine triphosphate (ATP). This process is under dual genetic control, with communication between the nuclear and mitochondrial genomes. Isolated complex I deficiency is the most common mitochondrial respiratory chain defect. There is a wide variety of clinical phenotypes. Subacute necrotizing encephalopathy (Leigh syndrome) and Leigh-like syndrome are common manifestations in infants. Causative mutations are found in mitochondrial DNA (mtDNA) as well as in nuclear DNA (nDNA). Mutations in mtDNA are maternally inherited while nuclear mutations most often are autosomal recessively inherited. In children, a multi-system disease is often seen, with a failure to thrive, encephalopathy, visual and hearing impairment, severe muscle weakness and dysfunction of the heart, liver, kidneys, and endocrine organs. Mitochondrial disease may lead to ocular problems. Dominant optic atrophy (DOA) and Leber’s hereditary optic atrophy (LHON) are both non-syndromic optic neuropathies with mitochondrial aetiology. Optic nerve hypoplasia (ONH) has also been described in relation to mitochondrial disease. In a recently Swedish study (Fahnehjelm et al 2010), ocular or visual problems were much more common than previously reported, occurring in 12 of 13 patients with mitochondrial disease. Optic atrophy occurred in 5 out of the 12 patients with an ocular diagnosis. One patient had a unilateral thickening of the nerve fibre layer and teleangiectatic microangiopathy in his left eye, similar to previously reported findings in asymptomatic carriers with LHON mutations. Motility problems with dysmetric saccades, asymmetrical smooth pursuits, instability in fixation, and gaze paralysis were common indicating an involvement of extra ocular muscles, brainstem, basal ganglia and cerebellum, which also was confirmed with MRI pathology. Flash and/or pattern VEP were pathological in 60% of the patients. With regard to the extra-ocular muscles, it is interesting to note that the abundant mitochondria in these energy-demanding muscles have been shown to respire at slower rates than mitochondria in skeletal muscles. The activity of complex I has shown to be lower than in normal extra-ocular muscle, which could explain the eye movements abnormalities in the patient in the present study, since saccadic and pursuit movements are energy dependent and thus sensitive to mitochondrial dysfunction. In conclusion, patients with complex I deficiency suffer different ocular disorders including optic atrophy and eye motility problems. The patients with severe somatic dysfunctions and brain damage also had the most severe visual impairment, motility dysfunctions and ocular pathology. Conclusions Young patients with inherited errors of metabolism and ocular manifestations present challenges to paediatric ophthalmologists but also make everyday practice multi-dimensional and exciting. The patients offer an opportunity to cooperate with colleagues from different disciplines. This encourages new clinical research and supplies opportunities to design various multidisciplinary scientific studies, hopefully resulting in clinical progress, beneficial outcomes and clinically relevant follow-up programs/clinical guidelines for ocular manifestations in children with inborn errors of metabolism. References Fahnehjelm K T, Törnquist A L, Malm G & Winiarski J (2006): Ocular findings in four children with mucopolysaccharidosis I-Hurler (MPS I-H) treated early with haematopoietic stem cell transplantation. Acta Ophthalmologica Scandinavica 84: 781-785. Fahnehjelm K T, Törnquist A L, Olsson M & Winiarski J (2007): Visual outcome and cataract development after allogeneic stem-cell transplantation in children. Acta Ophthalmologica Scandinavica 85: 724-733. Fahnehjelm, K T, Olsson M, Naess K, Wiberg M, Ygge J, Martin L, V Döbeln U (2010: Visual function, ocular motility and ocular characteristics in patients with mitochondrial complex I deficiency. ACTA Ophthalmologica Jan 8. Epub ahead of print. Gillingham M, Van Calcar S, Ney D, Wolff J & Harding C (1999): Dietary management of long-chain 3-hydroxyacyl-CoA dehydrogenase deficiency (LCHADD). A case report and survey. J Inherit Metab Dis 22: 123-131. Gillingham M B, Weleber R G, Neuringer M, Connor W E, Mills M, van Calcar S, Ver Hoeve J, Wolff J & Harding C O (2005): Effect of optimal dietary therapy upon visual function in children with long-chain 3-hydroxyacyl CoA dehydrogenase and trifunctional protein deficiency. Mol Genet Metab 2005 Sep-Oct;86(1-2):124-33. Gullingsrud E O, Krivit W & Summers C G (1998): Ocular abnormalities in the mucopolysaccharidoses after bone marrow transplantation. Longer follow-up. Ophthalmology 105: 1099-1105. Tyni T, Kivelä T, Lappi M, Summanen P, Nikoskelainen E & Pihko H (1998a): Ophthalmologic findings in long-chain 3-hydroxyacyl-CoA dehydrogenase deficiency caused by the G1528C mutation: a new type of hereditary metabolic chorioretinopathy. Ophthalmology 105: 810-824. Tyni T, Pihko H & Kivelä T (1998b): Ophthalmic pathology in long-chain 3-hydroxyacylCoA dehydrogenase deficiency caused by the G1528C mutation. Curr Eye Res 17: 551-559. Wraith J E (2005): The first 5 years of clinical experience with laronidase enzyme replacement therapy for mucopolysaccharidosis I. Expert Opin Pharmacother 6: 489-506. Acknowledgements The Editors wish to thank Publications Produced or Supported by the Bernadotte Foundation 1. Retinopathy of Prematurity. Reports from the Nordic Countries. Hans Fledelius, Gerd Holmström, Gunnar Lennerstrand, Eds. Acta Ophthalmologica, Volume 71, Supplement 210, 1993. 2. Eye Movements in Reading. Jan Ygge and Gunnar Lennerstrand, Eds. Wenner-Gren International Series, Volume 64, Pergamon Press,Oxford, 1994. 3. Pediatric Ophthalmology; some recent advances. Gunnar Lennerstrand, Ed. Acta Ophthalmologica Scandinavica, Volume 73, Supplement 214, 1995. 4. Advances in Strabismus Research: Basic and Clinical Aspects. Gunnar Lennerstrand and Jan Ygge, Eds. Wenner-Gren International Series, Volume 78, Portland Press, London, 2000. 5. Barnögonsjukdomar. Aktuell svensk forskning. Maj Ödman and Gunnar Lennerstrand, Eds. Johansson & Skyttmo Förlag, Stockholm, 2000. 6. Advances in Pediatric Ophthalmology Research. Reports presented at the 20th anniversary of the Sigvard & Marianne Bernadotte Research Foundation for Children Eye Care. Gunnar Lennerstrand and Gustaf Öqvist Seimyr, Eds. 2010.