Pertussis - WordPress.com
advertisement

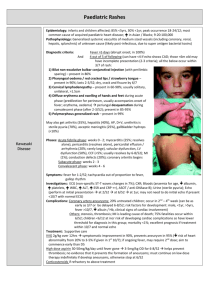
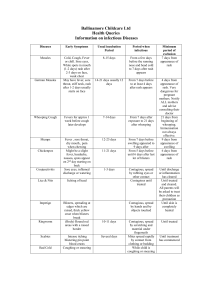
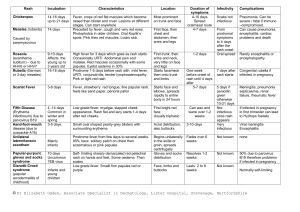
Pertussis / Parapertussis (Whooping Cough, 100 Day Cough) Epidemiology Mortality 0.5-1% if <6/12; 25% adult prolonged cough are due to pertussis Pathophysiology Aetiology: Bordatella pertussis (G –ive); parapertussis as common in 2-6yrs, but less common outside these Incubation period: 1/52 Symptoms 1-2/52 catarrhal phase 4-6/52 paroxysmal cough (assoc with vomiting, cyanosis; apnoea in young infants) recovery over 2-3/52 Complications Bronchopneumonia: in 25% <4yrs Seizures: in 2%; due to hypoxia from coughing Others: otitis media, intracerebral haemorrhage, subconjunctival haemorrhage, facial petechiae, encephalopathy, rectal prolapse, inguinal hernia Investigations NPA: do within 2/52 onset of cough Other: PCR, ELISA Management O2, suction Antibiotics: azithromycin: <6/12 = 10mg/kg OD PO >6/12 = 10mg/kg (max 500mg) PO 5mg/kg (max 250mg)OD PO for 5/7 Consider admission if: <6/12 (risk of apnoea) Contact prophylaxis: if <3 doses vaccine, >36/40, or attends their daycare; give azithromycin as above Differential Diagnosis Angioedema, diphtheria, laryngospasm, anterior mediastinal tumour, epiglottitis, bacterial tracheitis, retropharyngeal abscess, severe tonsillitis, foreign body aspiration Scarlet Fever Aetiology: Group A beta-haemolytic strep erythrogenic toxin Incubation: 2-4/7 (ie. Short) Symptoms: Acute onset fever, sore throat, headache, vomiting, abdominal pain exanthem develops over 1-2/7 Red tonsils and pharynx covered in exudates; Bright red / haemorrhagic spots on soft palate Tongue white coating through which red hyptertrophied papillae project (white strawberry tongue) White coating disappears after 4-5/7 red strawberry tongue After 12-48hrs Red, finely punctate 1-2mm blanching papules (rough sandpaper) on neck, axillae and groin Rapidly spreads to trunk and extremities Linear petechial eruptions in antecubital and axillary folds (Pastia’s lines) Facial flushing and circumoral pallor Fades at 6/7 Desquamates at 2/52, on hands and feet 1st Complications: otitis media, sinusitis, rheumatic fever, post-strep glomerulonephritis Investigations: ASOT, swab Treatment: Penicillin 10/7 Aetiology: RNA myxovirus Epidemiology: rare in immunised; now mostly seen in older patients; highly infectious (90% susceptible close contacts will become infected Incubation: 7-18/7 (av 10/7); 14/7 between exposure and rash; patient infectious from 5/7 before rash to 4/7 after rash Measles Case definition: 3-4/7 URTI rash 1. Fever >38 (ie. High) 2. Rash: fever always present at time of onset of rash; behind ears and at hairline spreads from head to feet, inc palms and soles; erythematous maculopapular, red blanching confluence esp on face copper-brownish hue as resolves desquamates after 3/7; lasts 1/52 3. 1 of cough / coryza / conjunctivitis / Koplick spots (white, bluish-white 1mm spots with red base on buccal mucosa; appear 1/7 before rash); may have generalised lymphadenopathy; may be diarrhoea Complications: otitis media (2.5%), pneumonia (4%; responsible for 50% deaths); encephalitis (0.1%; onset 1-2/52 after disease; mortality 10-15%; permanent neuro damage in 40%); subacute sclerosing panencephalitis (can occur 4-10yrs later, progressive mental deterioration and death); myocarditis, nephritis, hepatitis, pericarditis, keratitis Investigations: swab for PCR (will be +ive within few days, when serology may still be negative; also useful in immunocomp); blood for serology (IgM = infection, levels peak at 7-10/7; IgG = immunity; may be negative if <4/7 from onset fever, need to do repeat after 1/52, remains +ive for 3/12, sensitivity 100%, specificity 98%); double bag specs and don’t send through lamsen Treatment: Supportive; need infection control measures; notifiable disease; no school / child care for 5/7; admit if: poor PO intake, respiratory compromise, CNS complications Prophylaxis: Exposed if: enter same room within 2 hours of infected person leaving Non-immune if: not had 2x MMR and born after 1969, from 6/12 to 1st vaccine, if >4yrs and not had 2nd vaccine, pregnant, immunocomp, or prem <28/40 Offer MMR if <72hrs (not if pregnant); if immunocompromised / pregnant / >72hrs, consider Ig Henoch Scholein Purpura (HSP) is NOT a platelet problem Epidemiology: 2:1000; more Asian / Indian; usually 4-6yrs (2-11yrs) Aetiology: Allergic vasculitis, follows URTI, IgA mediated; associated with infection, drugs, vaccines; may be post Grp A strep Pathology: Small vessels (skin, GI tract, kidneys, joints) Symptoms: Palpable purpura on buttocks and legs (extensor surface) – presenting symptom in 50%; maybe also erythematous, urticarial, echymoses, petechaie Abdominal pain (+ nausea, vomiting, diarrhoea; in 60-80%; diffuse and colicky; occurs after rash; 50% have blood in stool; 5% get acute GI haemorrhage; 3% get intussusception) Migratory polyarthralgia (66-80%; presenting symptom in 25%; usually resolves after 24-48hrs; in gravity dependent joints) Renal failure (in 20-50%) – nephritic syndrome Generalized oedema (eg. Feet; often painful) Investigations: haematuria and proteinuria in 90%; urine, FBC (platelets normal); U+E’s Complications: Nephritic / nephrotic syndrome, ARF (<1%), HTN; if proteinuria = more severe and needs follow up; Intussusception (5%); bowel perforation Management: Usually resolves in 3-4/52; supportive; monitor BP and urine for 6/12; IV fluids if ill; NSAIDS; Consider prednisone 1mg/kg for 2/52 (if abdominal, joint or scrotal disease; may prevent renal complications (2% get long term renal impairment); helps joint pain, abdominal pain, oedema) Admit if: abdominal, renal complications; symptomatic relief Echovirus 9, Coxsackie virus A9 Enteroviruses Enterovirus (hand, foot and mouth disease) Coxsackie virus (herpangina) Transmission: Fecal-oral, oral-oral, respiratory-oral Symptoms: Non-specific febrile illnesses, respiratory tract infection, GI symptoms, meningitis; variety of rashes; Maculopapular rash beginning on face and neck, extending to trunk and feet; may be lesions on buccal mucosa and soft palate (resemble Koplik spots); maybe petechiae, vesicles, urticaria Duration: 5/7 Symptoms: Fever, anorexia, malaise, sore mouth 1-2/7 later, oral lesions then cutaneous lesions Oral lesions: painful 4-8mm vesicles on erythematous base on buccal mucosa, tongue, soft palate, gingiva ulcerate Cutaneous lesions: 3-7mm red papules grey vesicles on palms and soles (may be dorsum of feet and buttocks) heal in 7-10/7 Treatment: Hydration, analgesia, mouthwash Symptoms: Fever, mouth pain, oral ulcers Similar ulcers to hand, foot and mouth, but no skin lesions Rubella Erythema Infectiosum (Fifth Disease, Slapped Cheek) Incubation: 12-25/7 Symptoms: 1-5/7 fever, malaise, headache, sore throat irregular pink macules and papules on face, spreading to neck, trunk and arms; coalesces then clears Forchheimer spots: pinpoint petechiae on soft palate that coalesce Suboccipital and posterior auricular lymphadenopathy Treatment: Supportive Symptoms: Abrupt appearance of rash fiery red rash on cheeks; diffuse erythema of closely grouped tiny papules on erythematous base; edges slightly raised; circumoral pallor; sparing of eyelids and chin; lasts 4-5/7 1-2/7 after face rash nonpruritic macular/maculopapular erythema on trunk and upper limbs spreads; lasts 1/52; spares palms and soles; fades with central clearing Associated with fever, malaise, headache, sore throat, cough, coryza, nausea, vomiting, diarrhoea, myalgia Treatment: Supportive Herpes Transmission: HSV-2 genital, HSV-1 oral Symptoms: Herpes labialis, gingivostomatitis – painful umbilicated vesicles unroof and crust over Eczema herpiticum – break out on area previously affected by eczema Herpetic whitlow – distal fingers Treatment: Consider sexual abuse; Oral acyclovir; supportive Chickenpox Symptoms: Pruritic generalized vesicular exanthem with mild systemic symptoms; starts on trunk / scalp as faint red macules vesicular in 24hrs, on erythematous base dry and crust; widespread, palms and soles spared; may occur on mucous membranes Treatment: Supportive if uncomplicated; cleanse lesions to prevent secondary infection; antivirals only if immunocompromised If neonate exposed: nil treatment, present if develops chickenpox then treat with IV aciclovir Roseola Infantum (Sixth Disease) Impetigo Staph Scalded Skin Syndrome Erysipelas Scabies Symptoms: Abrupt onset of fever lasting 3-5/7, cough, coryza, anorexia, abdominal discomfort fever settles appearance of rash over 1-2/7. Erythematous, blanching, macular/maculopapular eruption, discrete rose / pale pink 2-5mm lesions; most on neck, trunk and buttocks; can also involve face and arms. No mucous membrane involvement. Lasts 1-2/7 fades rapidly. Treatment: Supportive Aetiology: Staph aureus, beta-haemolytic strep Symptoms: Lesions on face, neck, and extremities; usually no systemic symptoms Nonbullous: small erythematous macules and papules thin walled vesicles pustules rupture golden yellow crust smooth red surface underneath; may become confluent; local adenopathy Bullous: local; toxin causes separation of skin and bullae; thin walled bullae 0.5-3cm, filled with clear-yellow fluid, rupture easily Treatment: Nonbullous: topical; oral only if severe Symptoms: systemic; malaise, fever, irritability, tender skin; extensive areas of exfoliation; Nikolsky Treatment: inpatient, IVABx; may require admission to Burns unit Aetiology: Group A beta-haemolytic strep Symptoms: Fever, chills, malaise, vomiting; Local redness, heat, swelling; raised indurated border; well demarcated Treatment: Penicillin / erythromycin Symptoms: Severe pruritis; generalized eruption of linear burrows, papules, pustules, vesicles; mostly affect hand, feet, groin; excoriation from scratching Treatment: Permethrin Erythema Toxicum Seborrhoeic Dermatitis Symptoms: Erythematous macules 2-3cm on face, trunk, extremities; central 1-3mm pustules Treatment: None Symptoms: Greasy yellow/red scales, mostly on scalp; not pruritic Treatment: Mineral oil