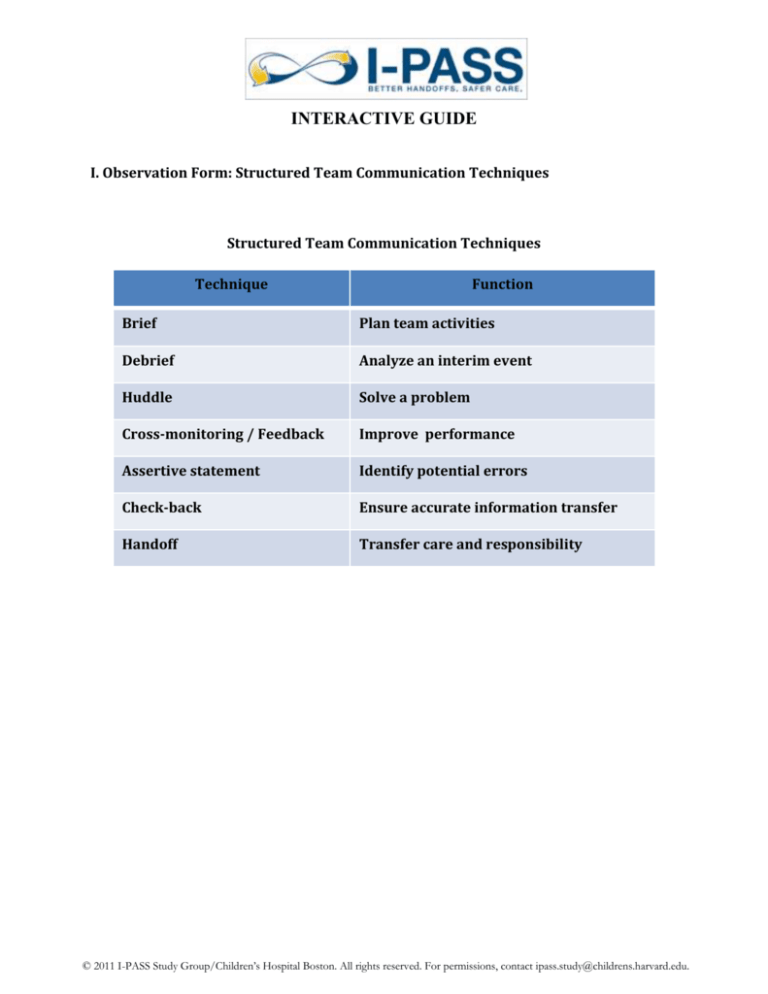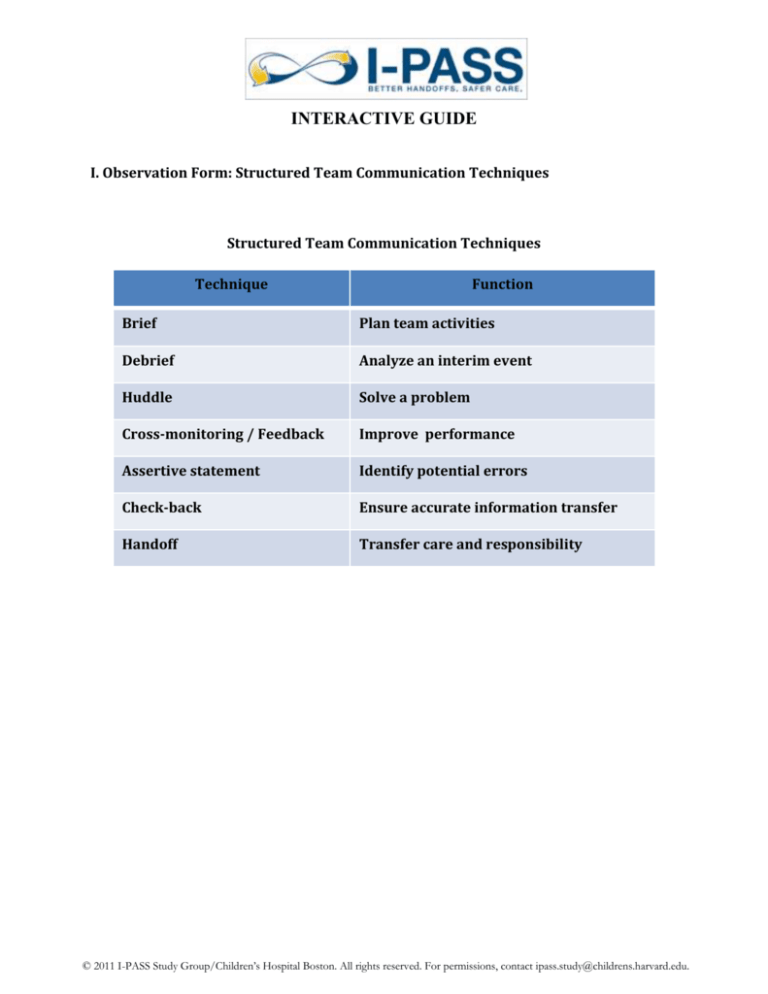
INTERACTIVE GUIDE
I. Observation Form: Structured Team Communication Techniques
Structured Team Communication Techniques
Technique
Function
Brief
Plan team activities
Debrief
Analyze an interim event
Huddle
Solve a problem
Cross-monitoring / Feedback
Improve performance
Assertive statement
Identify potential errors
Check-back
Ensure accurate information transfer
Handoff
Transfer care and responsibility
© 2011 I-PASS Study Group/Children’s Hospital Boston. All rights reserved. For permissions, contact ipass.study@childrens.harvard.edu.
Team Communication Technique #1 – Brief
A brief is a common short-term planning technique used to provide a team with an understanding
of the plans for the day or the shift, roles and responsibilities of team members, available resources,
workload, and any special circumstances. Briefs are “pre-game” team meetings.
Brief Checklist
During the brief, the team should address the following questions:
___ Who is on the team?
___ All members understand and agree upon goals?
___ Roles and responsibilities are understood?
___ What is our plan of care?
___ Staff and provider's availability throughout the shift?
___ Workload among team members?
___ Availability of resources?
As you watch the video clip, think about:
1. How does this technique contribute to the team’s better understanding of plans and resources?
2. What are some of the advantages of the use of this technique prior to daily inpatient rounds?
This video clip demonstrates the efficiency and effectiveness of briefs in day-to-day patient care.
Briefs are helpful to organize work and make explicit the contributions and needs of each team
member.
2
© 2011 I-PASS Study Group/Children’s Hospital Boston. All rights reserved. For permissions, contact ipass.study@childrens.harvard.edu.
Team Communication Technique #2 – Debrief
A debrief is a recap of a situation or the day’s events for the purposes of process improvement. In a
debrief, team members review the content of the earlier brief in an attempt to trouble shoot and
correct problems or learn from errors.
Debrief Checklist
The team should address the following questions during a debrief:
___ Communication clear?
___ Roles and responsibilities understood?
___ Situation awareness maintained?
___ Workload distribution equitable?
___ Task assistance requested or offered?
___ Were errors made or avoided? Availability of resources?
___ What went well, what should change, what should improve?
As you observe the video illustrating this technique, please reflect on the following questions:
1.
How could you apply this tool to your day-to-day practice?
2. What potential is there for debriefs to identify systems-level problems that could further
enhance patient care?
This video clip illustrates the usefulness of structured team communication techniques in
improving team function.
3
© 2011 I-PASS Study Group/Children’s Hospital Boston. All rights reserved. For permissions, contact ipass.study@childrens.harvard.edu.
Team Communication Technique #3 – Huddle
The huddle is a technique to reinforce plans already in place for patient care or to assess the need
to change plans. It serves to develop a shared understanding among team members about what is
happening now and what to do next. Huddles typically occur in the pre-operative process to verify
key information.
Huddle Checklist
The team should address the following questions during a huddle:
___ Were teams members able to express concerns?
___ How could outcomes have been anticipated?
___ Contingency plans identified??
___ Resources assigned?
___ Was there a consensus?
As you watch this video clip, think about the following questions:
1. When was the last time that you participated in a huddle and what was the outcome of that
huddle?
2. In what other situations would a huddle be useful?
This video clip illustrates how using a structured technique for discussing critical issues and
emerging events are so important to maintain situation awareness and develop contingency plans.
4
© 2011 I-PASS Study Group/Children’s Hospital Boston. All rights reserved. For permissions, contact ipass.study@childrens.harvard.edu.
Team Communication Technique #4 – Cross-monitoring /Feedback
Feedback is used frequently as part of cross monitoring. Cross monitoring is monitoring the actions
of your team members to provide a safety net so that the team can address and correct errors in
real time.
Cross-Monitoring/ Feedback Checklist
Feedback should be:
___ Timely – given soon after the observed behavior occurred
___ Respectful – focus on behaviors, not personal attributes
___ Specific – be specific about what behaviors need correcting
___ Directed towards improvement – plan for future improvement
___ Considerate – deliver information with fairness and respect
In the video clip, please observe the scenario and reflect about the following questions:
1.
How well did the junior resident demonstrate the effective use of cross-monitoring?
2. Did you perceive receptivity of other team members to his comment?
This video clip illustrates how early detection with cross monitoring and direct, timely feedback
contributes to effective team function and enhanced understanding of team members.
5
© 2011 I-PASS Study Group/Children’s Hospital Boston. All rights reserved. For permissions, contact ipass.study@childrens.harvard.edu.
Team Communication Technique #5 – Assertive Statement
An assertive statement is made in the context of advocating for a patient. When team members’
viewpoints do not coincide with the decision maker, an assertive statement is made to prevent a
medical error and promote patient safety. A assertive statement is done in a firm and respectful
manner.
Assertive Statement Checklist
An assertive statement consists of five steps:
___ Open the discussion in a timely manner
___ State the concern, saying, “I am concerned…”
___ Offer a solution
___ Obtain agreement
As you observe the scenario in this video clip, reflect about the following questions:
1.
How did the medical student phrase her assertive statement to make it effective?
2. How does institutional culture contribute to the effective use of this technique?
Advocating for patients and making assertive statements across hierarchical boundaries are all
elements of an institutional culture of patient safety.
6
© 2011 I-PASS Study Group/Children’s Hospital Boston. All rights reserved. For permissions, contact ipass.study@childrens.harvard.edu.
II. LEARNING STYLE EXERCISE
What is your learning style?
Active --------------------------------------- Reflective
Sensing --------------------------------------- Intuitive
Visual ------------------------------------------- Verbal
Sequential --------------------------------------Global
What is your partner’s learning style?
Active --------------------------------------- Reflective
Sensing --------------------------------------- Intuitive
Visual ------------------------------------------- Verbal
Sequential --------------------------------------Global
Interview your partner, then share with the group:
What are at least two ways to enhance the way you receive information?
7
© 2011 I-PASS Study Group/Children’s Hospital Boston. All rights reserved. For permissions, contact ipass.study@childrens.harvard.edu.
III. THE I-PASS HANDOFF
I
P
A
S
S
Illness
Severity
Patient Summary
Action List
Situation Awareness &
Contingency Planning
If he develops more
tachypnea or
hypoxemia repeat
CXR, consider ICU
evaluation for CPAP
If cultures are
positive, adjust
antibiotics
accordingly
If significant clinical
change Dr. Smith is
the attending
hematologist tonight
please update him
Synthesis by
Receiver
M6E Barton, James
4/19/1998
MRN: 12345678
Visit: 45612
Adm Date: 3/13/11
Attending: Brown, Julie
Code Status:
Allergies: NKDA
Wt: 40 kg
Access:
Resident: Cameron, Jack
13 year old male w h/.o Sickle cell disease previously
complicated by recurrent pain crises, stroke, and acute
chest.
Medications
Ampicillin Sulbactam IV
Morphine PCA IV
Admitted 2 days ago with leg pain.
1 day PTA w/ worsening L calf pain not relieved by po
analgesics. Day of admission refusal to walk. In ED
afebrile, no signs acute chest, baseline neuro exam.
Now today with concern for onset of new fever, hypoxia
and RLL infiltrate.
Probable acute chest syndrome
New fever, hypoxia, and RLL infiltrate today,
tachypnea to 30s, hematology and ICU aware of
change in status; Plan to continue amp/sulbactam,
wean 2L O2 as tolerated, incentive spirometry,
follow cultures
Pain Crisis - Leg pain well controlled on a
morphine PCA; continue at current settings and
monitor pain scores
Anemia/hypertransfusion non-compliance transfused yesterday, HCT 8→10 today; plan to
follow daily hct and emphasize hypertransfusion
compliance with grandmother prior to d/c
History of stroke – residual right-sided weakness at
baseline this admission; plan to continue to monitor
Poor po intake - worsened since admission, felt
secondary to pain and respiratory status; continue
1.5x MIVF with D5 ½ NS
Respiratory check
now to get
baseline and at
least Q4 during
the night
Monitor pain
scores
Monitor ins and
outs
Follow up
electrolytes and
pending cultures
Handoff Video: What techniques did they use that were particularly effective? What pitfalls did you notice?
© 2011 I-PASS Study Group/Children’s Hospital Boston. All rights reserved. For permissions, contact ipass.study@childrens.harvard.edu.
SYNTHESIS
BY
RECEIVER
IV. PATIENT SUMMARY
Exercise 1
You are the night shift intern who admitted AJ and wrote the H&P below. It is 8am and your
shift is about to end. After reviewing the information below, compose an example of what a
patient summary for AJ might look like on the written handoff document.
HPI:
AJ is a 4 year old male who presented to the ED with a 2 day history of worsening intermittent,
productive cough and high fevers (Tmax 103°). Earlier today he developed acute worsening of
his respiratory effort, and per his mother his breathing was fast and labored. Deep, subcostal
retractions were also noted. Multiple family members were also sick at home. His mother
notes a decrease in his PO intake of fluids, though no diarrhea or vomiting. No complaints of
ear, abdominal, or joint pain, as well as no rash.
PMH:
Ex-26 week preemie due to preeclampsia in mom, intubated for two weeks following birth, no
history of BPD
3 prior admissions to general pediatric service for pneumonia
PSH: N/A
FH: Father – Asthma; Mother – Gestational diabetes, preeclampsia
SH: Lives with parents and 2 year old sister, attends preschool, no tobacco use in the home
Immunizations: Up to date for age per ACIP guidelines
ROS: Denies headache, lethargy, chest pain, hemoptysis, rash, dysuria, diarrhea, and vomiting
Allergies: NKDA
Medications: Ibuprofen PRN for fever
Physical Exam:
o Vitals – T 102.5°, RR 40, HR 120,
o Cardiac – Tachycardic, no murmurs,
Pulse Ox 89-91% on room air
and cap refill of 2-3 seconds
o Gen – Ill appearing, labored
o Lungs – Labored breathing and
breathing, crying and clinging to
retractions, crackles and decreased
mother
aeration at the left lung base, no
o HEENT – Normocephalic, tympanic
wheezing
membranes slightly erythematous
o Abd – Soft, non-tender, normal
though with good landmarks, dry
bowel sounds
oral mucosa, mild pharyngeal
o Musculoskeletal – No joint swelling
erythema though no exudate or
o Neuro – Grossly intact exam
tonsillar enlargement
o Skin – No rash, abrasions, or
o Neck – Supple, full range of motion,
petechial noted
no adenopathy
Labs:
o CBC: WBC 19K with 8% bandemia, Hgb/Hct 12.3/36, Plts 520K
o Electrolyte Panel: Na 130, K 4.5, Cl 107, HCO3 21, BUN 20, Cr 0.6
o ESR: 72, CRP: 21
o Capillary blood gas: 7.46/24/base excess of 6
Imaging:
o Chest X-Ray: Left lower lobe infiltrate
© 2011 I-PASS Study Group/Children’s Hospital Boston. All rights reserved. For permissions, contact ipass.study@childrens.harvard.edu.
ED course:
AJ was placed on 2L of supplemental oxygen therapy and an IV fluid bolus of 20 ml/kg of normal
saline was administered. His first dose of ampicillin was administered in the ED and he was
subsequently admitted to the floor with pneumonia, respiratory distress and hypoxia.
On admission to the floor:
AJ arrived to the floor with tachypnea and continued tachycardia. Maintenance IV fluids with D5NS
were continued. His oxygen was increased to 2.5 L for the respiratory distress. The parents and
nurses expressed concern about his status and that he may require closer monitoring in an ICU
setting if he did not improve. On admission, the working diagnoses for his hyponatremia included
volume depletion as well as SIADH.
Summary statement:
Events leading up to admission:
Hospital Course:
Ongoing Assessment by problem/diagnosis:
Plan by problem/diagnosis:
10
© 2011 I-PASS Study Group/Children’s Hospital Boston. All rights reserved. For permissions, contact ipass.study@childrens.harvard.edu.
Patient Summary Video Example
Did they capture all of the essential elements?
Did their verbal handoff differ from your written patient summary?
Patient Summary Exercise 2
HOSPITAL COURSE FOLLOWING ADMISSION:
The day following admission AJ’s respiratory status improved slightly and his oxygen
requirement decreased. His work of breathing improved and he was no longer tachypneic.
With hydration his Na improved to 136 by the afternoon and the D5NS was stopped, and his
fluids were switched to D5 ½ NS.
Early the in the morning on the following day he developed an increase in his oxygen
requirement and worsening respiratory distress. A stat chest X-Ray was ordered and revealed
worsening of the left sided infiltrate and a moderate sized effusion. AJ had an urgent
ultrasound of the chest obtained that should a moderate to large sized free-flowing effusion.
Plans for placement for a chest tube for drainage of the effusion were initiated. His Na that
morning was also found to be 139, and he was continued on maintenance IVF with D5 ½ NS
given his NPO status prior to the procedure. A chest tube was subsequently placed by
interventional radiology without complication later that morning and exudative fluid obtained.
The surgery service was consulted to assist with management of the chest tube. Following
placement of the chest tube AJ’s respiratory status improved and his oxygen was weaned to 1L.
In addition, his tachypnea and tachycardia improved throughout the day. His chest tube was
kept to low wall suction and he continued to have drainage of fluid from the tube throughout
the day.
You are the day intern leaving and need to handoff back to the night intern. Please compose
a patient summary on the patient now 48 hours into admission.
11
© 2011 I-PASS Study Group/Children’s Hospital Boston. All rights reserved. For permissions, contact ipass.study@childrens.harvard.edu.
Summary statement:
Events leading up to admission:
Hospital Course:
Ongoing Assessment by problem/diagnosis:
Plan by problem/diagnosis:
12
© 2011 I-PASS Study Group/Children’s Hospital Boston. All rights reserved. For permissions, contact ipass.study@childrens.harvard.edu.
V. Contingency Planning
Exercise
Refer to the patient summary you wrote about AJ, the 4 year-old ex-premie who was
admitted with pneumonia and hyponatremia.
What contingency plans would you recommend for this patient at the time of the handoff
after admission (before complication of the effusion)?
NOTES:
13
© 2011 I-PASS Study Group/Children’s Hospital Boston. All rights reserved. For permissions, contact ipass.study@childrens.harvard.edu.