House Bill 216 Health and Aging Committee Proponent
advertisement

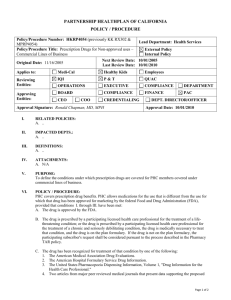
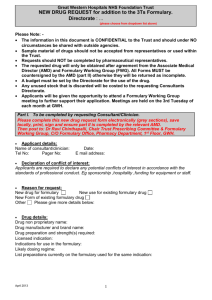
House Bill 216 Health and Aging Committee Proponent Testimony January 20, 2016 Carol Cairns, MSN, APRN-CNP and OAAPN Director, Prescriptive Authority Chairwoman Gonzales, Vice Chairman Huffman, Ranking Member Antonio, and members of the committee, thank you for the opportunity to speak this morning. I am Carol Cairns, a certified acute care nurse practitioner and adult hospitalist at Blanchard Valley Health System in Findlay, Ohio. I also am the OAAPN director for prescriptive authority. In earlier testimony, my colleague provided a brief overview of the formulary process. I am expanding on her comments to give insight into the complexity of the formulary and why it impedes patient safety, delays access to care and increases health care costs. Ohio is one of only five states with a prescriptive formulary. This fact means that 45 of 50 states, or 90% of the country, find a prescriptive formulary unnecessary for APRN practice. Of the five outlier states, Ohio is the only one with an inclusionary and exclusionary formulary, which indicates what may and may not be prescribed. The policy rationale for implementing the formulary 16 years ago was to ensure patient safety. However, in clinical practice, the exact opposite is occurring. This cumbersome formulary, which until a few months ago was 35 pages long and needed five pages of instruction to explain it, impedes patient safety as well as the efficient delivery of care. Page 1 of 4 The current formulary is constantly out of date, as new FDA approved drugs are made available to prescribing health care professionals. The Committee for Prescriptive Governance (CPG) uses a reference drug source that is not the existing standard in institutional and other health care settings. Additionally, this online reference requires a subscription that costs more than $700, making it financially unfeasible for the majority of prescribing APRNs to obtain. The CPG prescribing categories are chosen based on majority group opinion, not on evidencebased data, and by people who may not be prescribers or do not know APRN education or practice. Ohio’s convoluted APRN formulary confuses and frustrates prescribing providers. For example, APRNs may prescribe phentermine-topiramate, an extended release appetite suppressant, but not the base drug phentermine, an appetite suppressant. It also has confused local and national mail order pharmacies, which have refused to fill medications based on the complexity and misunderstanding of this formulary. In one recent case, a child’s seizure medication was delayed for days as the pharmacy incorrectly insisted on a signature from a physician. The diagnosis and care of the patient by the APRN was indeed appropriate, but the constantly changing formulary confused the pharmacy, resulting in the delay of the medication for days, and placed this child at undue risk of seizure. Last week, an APRN requested help to decipher the medications she could prescribe in a specialty clinic. She was “concerned” as she “did not want to get in trouble” if she ordered a different route of a medication listed “in accordance with the Standard Care Arrangement.” Additionally, the drug classification outlined in the existing formulary was unclear on what biologics she could prescribe. Her practice could not help her, as this was the first time they had an APRN onboard. Page 2 of 4 My organization as well as the Board of Nursing receives continual requests for assistance in deciphering the formulary. It is not unusual that a clear answer is not found because the formulary is flawed and nebulous. In fact, one of Ohio’s children’s hospitals developed an algorithm to help navigate the formulary. This tool illustrates how unreasonably complex and time consuming it is to determine the prescribing category of a medication. Is this acceptable in Ohio? Ohioans don’t deserve such a roadblock to care. It is important to understand why 45 of 50 states do not find it necessary to have any prescribing formulary and patient outcomes are excellent in those states. APRNs are already educated to prescribe medications based on their national certification, education and training, just as other prescribers do. A family practice physician would not treat a patient with intravenous chemotherapy, though legally able to do so. Likewise, an APRN does not prescribe medications outside of the certification scope. APRN specialty certification demonstrates the ability to provide differential diagnosis and treatment, which includes drug prescription. APRNs are educated in advanced pharmacology and prescribing ethics and law, as well as the treatment of any potential interactions or complications. There are multiple studies on APRN patient outcomes, which demonstrate quality care, as APRNs are safe prescribers. It is important to understand that an APRN’s standard of care, including prescribing, is based on evidence-based, national guidelines, the same as any other health care provider. This is true whether I admit a patient to the intensive care unit with a heart attack or respiratory failure, a primary care APRN sees a patient in the office with Page 3 of 4 uncontrolled diabetes, a nurse anesthetist provides anesthesia to a cardiac bypass patient, or a nurse midwife delivers a baby. This cumbersome and unnecessary formulary leads to delays in patient care and prescription refills, mistaken prescription denials and frustrated patients. As exemplified in my anecdotes, the formulary puts patients at risk and indirectly increases health care costs. The sad reality is that Ohio is not at the top of its health care game! Removal of barriers to APRN practice is key to improving patient access to care, patient safety and decreasing health care costs. As someone who works in a hospital setting treating patients with acute and critical illness, I can tell you that nothing is more important than the ability to meet a patient’s need quickly and safely, while providing outstanding, evidence-based care. APRN prescribing and care of the patient is based on the same standard as any other health care provider. House Bill 216 is a common sense prescription for better health in Ohio – directly in terms of patient care and safety, professionally for keeping talented advanced practice nurses, and fiscally for the bottom line of our state. I sincerely thank you for the opportunity to speak with you today. Page 4 of 4